Abstract
Abstract
Introduction: Visual loss due to tuberculous optochiasmatic arachnoiditis (OCA) is one of the devastating complication tuberculous meningitis. The inflammatory exudates in tuberculous meningitis have a strong prediction to the basal cisterns of the brain resulting in OCA. The commonly ascribed causes of visual impairment in tuberculous meningitis are direct involvement n of the visual pathway structures (optic nerve, choroid, retina and retinal vasculature), optochiasmatic arachnoiditis, optic nerve granuloma, increased intracranial pressure and ethambutol toxicity. Apart from tuberculosis other causes for OCA are sarcoidosis, neurocysticercosis and trauma.
Aim This study evaluates the clinical, demographic profile, biochemical parameters, imaging profile, severity of visual impairment and response to treatment, and its predictors in OCA patients.
Materials and Methods: The patients who were admitted with TBM (Tuberculous meningitis) in the neurology wards and medical wards of a tertiary care hospital were evaluated for the occurrence of this complication and only those patients were enrolled in the study. Of the TBM (n= 78), 15.38% (n=12) patients developed TCA. They developed impairment of vision at a presentation during admission or during the course of illness.
Results: Analysis revealed that the affected were predominately females (n=9, 75%) and especially postnatal women. Assessment of clinical severity of TBM (done by MRC grading) showed that 7 patients (58.33%) were in stage III illness, 5 patients (41.66%) in stage II illness. On the clinical assessment of visual acuity 83% were blind (by Indian def. of visual acuity), and 17% had lesser grades of visual impairment. Those who were legally blind had cerebrospinal fluid (CSF) protein more than 500mg/dl. Analysis of the images showed that apart from exudates in the basal cistern, there was evidence of other associated complications.
Conclusion: This study reveals that the occurrence of optochiasmatic arachnoiditis in patients with TBM has to be predicted in the age group (20-25), female sex, postpartum women, patients in stage II, stage III illness, significantly elevated CSF (cerebrospinal fluid) proteins (> 500mg/dl), The affected patients showed a poor response to treatment.
Keywords: OCA - Tuberculous Optochiasmatic arachnoiditis, TBM - Tuberculous meningitis CSF – cerebrospinal fluid.
Introduction
Tuberculous Optochiasmatic arachnoiditis (OCA) is the most devastating form of tuberculous meningitis.[1]
Optochiasmatic arachnoiditis is defined as inflammation of the arachnoid mater of the optic nerve and chiasmatic cisterns and is associated with varying degrees of visual disturbances. Optochiasmatic arachnoiditis, originally known as the Syndrome de Balado, has also been recognized as a clinical entity since a detailed description by Balado and Satanowsky in 1929.
The impairment of vision in patients with optochiasmatic arachnoiditis is often of insidious onset and slowly progressive, but rarely it can be of acute onset. The vision loss may be unilateral or bilateral, and frequently blindness is complete. In addition to the visual loss, impaired pupillary response to light and optic atrophy have also been described as manifestations of tuberculous optochiasmatic arachnoiditis.
India is a developing country with a high incidence of tuberculosis [2]and TBM accounts for 1% of all cases of Tuberculosis and so TBM and OCA can be an important cause for the development of vision loss. Though a lot of treatment strategies have been reported the outcome of treatment depends on the stage of initiation of treatment and most often vision loss has been left back as permanent residual sequelae.
Aims
This study evaluates the clinical, demographic profile, biochemical parameters, imaging profile, severity of visual impairment and response to treatment, in TCA patients.
Materials and Methods
All Patients admitted with TBM in the neurology wards of a tertiary care teaching hospital over a period of 2 years formed the material for this study. Tuberculous meningitis patients (n= 78) who developed impairment of vision at a presentation during admission or during the course of illness were enrolled. A complete neurological examination was done, and diagnosis of TBM was made applying Ahuja et al. criteria.[3] The diagnosis of tuberculous optochiasmatic arachnoiditis (n=12) was made based on a complete clinical assessment of vision and imaging (MRI with gadolinium). The patients were subsequently were followed up for a period of 9- 12 months. The patients with TBM were staged according to MRC staging.[4] The British Medical Research council distinguishes three clinical stages of TBM based on three parameters. 1. Level of consciousness 2. Focal neurological deficits 3. Presence of seizures, meningism, and behavioral changes. After diagnosing symptomatic OCA, 12 were continued on treatment with ATT (anti-tubercular treatment) (INH, Rifampicin, Ethambutol and Pyrazinamide) + oral steroids (dexamethasone 0.1 mg/kg/day in divided doses for 1 month and then a tapering schedule over the next 2 weeks). The patients enrolled were given strict advice regarding the necessity to follow up and to adhere to drug compliance.
Diagnosis of OCA was made based on detailed clinical evaluation, vision assessment and imaging (MRI with Gadolinium contrast). Perichiasmal enhancement and hypertrophy of chiasma, a cisternal segment of the optic nerve as evidence of optochiasmatic arachnoiditis.
The clinical features and other associated complications that developed during the course of illness was documented. The visual acuity (Snellen chart), pupillary light reflex and swinging flash test was done at enrollment and subsequent follow-up.
Results
OF the 78 adult patients with TBM, 12(15.38%) patients had TCA among which there were 9 females (75%) and 3 males (25%). The age distribution was 2 patients in 15 – 19, 8 patients in 20 – 24, 1 patient in 25 to 29 and 1 patient 30 -34 years. The mean age was 24 years. The affected individuals were predominantly in the 20 to 24 year age group 6 patients were postnatal women
Assessment of clinical severity of TBM (done by MRC grading) showed that 7 patients (58.33%) were in stage III illness, 5 patients (41.66%) in stage II illness and none of them were in stage 1 illness. The patients with TBM were staged according to MRC staging.[4]
Table 1: Severity of visual impairment
|
S. No. |
Visual Impairment |
n=12 |
WHO Definition |
Indian Defintion |
|
1. |
6/6 – 6/18 |
- |
- |
- |
|
2. |
<6> |
2(16.66%) |
Visually impaired |
Low vision |
|
3. |
<6> |
3(25%) |
Severe Visual impairment |
BLIND |
|
4. |
<3> |
3(25%) |
BLIND |
BLIND |
|
5. |
<1> |
2(16.66%) |
BLIND |
BLIND |
|
6. |
NPL |
2(16.66%) |
BLIND |
BLIND |
Ten out of 12 patients (83.33%) were blind according to the standard WHO definition for visual impairment. Seven patients were in stage III illness and 3 in stage II illness, none in stage I illness. Two patients (17%) had had lesser grades of visual impairment. They were in stage II illness. All had absent menace and absent aversion to bright light and were classified as "Blind" according to WHO definition for visual impairment or "Social blindness" according to the NPCB criteria.[5] The patients diagnosed to have OCA, n=12 were treated with antitubercular drugs (ATT-INH, Rifampicin, Ethambutol and Pyrazinamide) with oral steroids (dexamethasone 0.1mg/kg/day in divided doses for 1 month and then a tapering schedule over the next 2 weeks). None of these patients improved with treatment and they continued to have the same severity of visual impairment.
Clinical, radiological, CSF and other laboratory parameters were compared and analyzed in patients with TBM with OCA
Table 2: Radiological Features
|
Variable |
OCA (n=12) |
|
Infarct |
2 |
|
Hydrocephalus |
3 |
|
Meningeal enhancement |
5 |
|
Basal Exudates |
6 |
|
Granuloma |
6 |
 |
Click here to view |
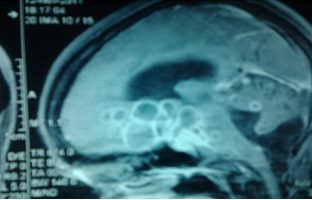
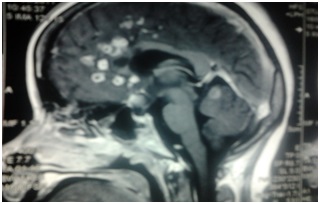
Fig. 1: T1W contrast (gadolinium) sagittal MRI images; shows multiple rounded and confluent ring and nodular enhancing lesions in the suprasellar cistern involving the optic chiasmatic region.
 |
Click here to view |
Fig. 2: T1W contrast (Gadolinium sagittal) MRI images; multiple rounded and ring and nodular enhancing lesions and exudates in optochiasmatic region.
Associated hydrocephalus (communicating type) was present in 3 /12 patients. Basal exudates in 6/12 and meningeal enhancement in 6/12 patients.
Table 3: CSF Parameters
|
Proteins mg/dl |
n=12 |
|
200 – 500 |
3 |
|
501 – 1000 |
6 |
|
> 1 GM |
3 |
Nine (75%) had CSF proteins more than 500mg/dl and all nine were legally blind. Those who were legally blind had CSF protein more than 500mg/dl.
Discussion
In our study, we found 15.38% of people with TBM developed TCA. A study done by Aaron et al[6] shows 14% of people affected with TBM developed TCA. A study done by sinha et al[7] shows vision impairment occurred in one- fourth of patients with tuberculous meningitis and the main causes of vision loss were OCA and optochiasmal tuberculoma. In our study women were predominantly affected, the female to male ratio was 3:1. The age group affected were 20 to 24 years. The robust immune response in younger individuals may explain the higher incidence of OCA in this age group.
Our study shows that Early postpartum women are more likely to develop tuberculosis than nonpregnant women.[8] The maternal hormones and placental products produce immunomodulation, and hence pregnancy is considered to be an immunosuppressed state and in the postpartum period, there is immune reconstitution. Hence the postpartum period induces active diseases mostly with extrapulmonary or disseminated lesions from the latent state mainly due to immune reconstitution after delivery. This could be the reason for the occurrence of this fulminant complication in postpartum women.
Once established, none of our patients showed improvement with treatment, emphasizing the need to prevent this complication. Early recognition may be helpful in preventing this complication. Improvement of sensorium and/or neurological deficit was observed in patients on treatment with intrathecal hyaluronidase.[9]Other treatment modalities that have been tried in treating tuberculous arachnoiditis are thalidomide [10]and microsurgical intervention[11]
Conclusion
A strong degree of anticipation of OCA is needed while treating patients with TBM. The predicting factors for this complication are young females, especially postpartum women, patients with high levels of CSF protein, and patients with higher stages of TBM. Starting corticosteroids along with ATT may help in preventing this complication.
Conflicts of Interest: None.
References
- ^ Garg RK, Paliwal V, Malhotra HS. Tuberculous optochiasmatic arachnoiditis: a devastating form of tuberculous meningitis. Expert Rev Anti Infect Ther 2011 Sep;9(9):719-29. doi: 10.1586/eri.11.93.
- ^ Chakraborty AK. Epidemiology of tuberculosis: current status in India. Indian J Med Res 2004;120:248-276
- ^ Ahuja GK, Mohan KK, Prasad K, Behari M. Diagnostic criteria for tuberculous meningitis and their validation. Tuber Lung Dis 1994;75:149-152
- a, b Medical Research Council Report: Streptomycin treatment of tuberculous meningitis. Lancet 1948;1:582-596.
- ^ Bachani D, Limburg H. National Programme for Control of Blindness in India: Course material for training district programme management, New Delhi. Ophthalmic Section. Directorate General of Health Services, Ministry of Health and Family Welfare 1996.169.
- ^ Aaron S, Mathew V, Anupriya A, Sunithi M, Maya T, Goel M, et al. Tuberculous optochiasmatic arachnoiditis. Neurol India 2010;58:732-735.
- ^ Sinha MK, Garg RK, Anuradha HK, Agarwal A, Singh MK, Verma R, et al. Vision impairment in tuberculous meningitis: predictors and prognosis. J Neurol Sci 2010;290:27-32
- ^ Shinohara T, Kagawa K, Okano Y. Disseminated tuberculosis after pregnancy progressed to paradoxical response to the treatment: report of two cases. BMC Infect Dis 2016;16:284.
- ^ Gourie-Devi M, Satish P. Hyaluronidase as an adjuvant in the treatment of cranial arachnoiditis (hydrocephalus and optochiasmatic arachnoiditis) complicating tuberculous meningitis. Acta Neurol Scand 1980;62:368-381.
- ^ Stefan DC, Andronikou S, Freeman N, Schoeman J. Recovery of vision after adjuvant thalidomide in a child with tuberculous meningitis and acute lymphoblastic leukemia. J Child Neurol 2009;24:166-169.
- ^ Navarro IM, Peralta VH, Leon JA, Varela EA, Cabrera JM. Tuberculous optochiasmatic arachnoiditis. Neurosurg 1981;9:654-660.





