Abstract
Introduction: ‘Macrocytosis’ is the term used to describe large erythrocytes with increased mean corpuscular volume (MCV) seen in peripheral blood smears. Various pathological disorders with differentiating clinical, biochemical, hematological and bone marrow findings can attribute to macrocytosis.
Aims and Objectives: We conducted a one year study, from Sep 2016 to Sep 2017 with the aim to identify the number and causes of macrocytosis and also to assess the haematological features associated with macrocytosis in peripheral blood smear and routine haemogram. We also evaluated the clinical, biochemical (Vitamin B12 and folate assay) and bone marrow studies to differentiate megaloblastic from nonmegaloblastic causes of macrocytosis.
Results: Among 56 cases of macrocytosis received in a year, Megaloblastic anemia was the commonest etiological factor, followed by alcoholism and drug intake. Isolated macrocytosis without anaemia was noted in 4 cases. Presence of hypersegmented neutrophils and macro- ovalocytes was the most frequent observation in peripheral smear examination in all megaloblastic conditions.
Conclusions: A meticulous interpretation of routine haemogram along with peripheral blood smear and biochemical analysis helps in identifying the underlying cause and treatment for macrocytosis.
Keywords: Macrocytes, Megaloblastic anaemia, Mean corpuscular volume (MCV), Peripheral blood smear.
Introduction
Peripheral blood smear and Hemogram are one of the commonest routine investigations done in pathology laboratories, yielding significant results on various hematological parameters. A wide range of alteration in shape and size of RBCs are encountered among various disorders giving rise to a wide range of MCV. One of the commonly encountered finding is Macrocytosis, having increased mean corpuscular volume (MCV) on routine hemogram.(normal adult MCV range from 80-100 femtolitres (fl).[1] MCV more than 100 fl is indicative of macrocytosis.[2],[3][4] and prevalence of macrocytosis lies between 1.7 - 3.6% in population.[5][6]
Macrocytosis is considered to be a normal physiological finding in newborns, infants and pregnant females. A false rise in MCV is observed in reticulocytosis, hyperglycemia, leukocytosis, presence of cold agglutinins along with delay in processing of sample. Rarely macrocytosis without symptomatic anemia can be seen in family members, having genetic predisposition.[2][5]
All the causes of macrocytosis has its own mechanism of formation, resulting in larger than normal erythrocytes. Vitamin B12/folate deficiency leads to defective cellular division due to defect in nuclear maturation, wherein hemoglobin synthesis continues normally, but nuclear division lags behind, resulting larger RBCs. Bone marrow is usually hypercellular with increase in myeloid and erythroid lineage cells. Erythroblasts appear large with immature, lacy nucleus. These changes in the marrow are known as megaloblastic changes indicating Vit B12 deficiency.[5]False positive rise in MCV is seen in conditions associated with reticulocytosis (polychromatophilic RBCs which are larger than normal RBCs) like hemolysis, acute bleeding.[5] Presence of macro-ovalocytes is a sensitive while that of hypersegmented neutrophils is a more specific finding in megaloblastic anemia.[7][8] Also, Disorders of hepatobiliary system results in excess lipids deposition on the erythrocyte membrane, causing macrocytosis.[9][10] Macrocytosis in hypothyroidism is attributed to physiological adaptation to the decreased tissue oxygen requirements as a result of slower basal metabolic rate.[11]
Our study was conducted to identify macrocytosis and accompanying hematological parameters in peripheral blood smear and routine hemogram and also to identify the underlying etiology in each case.
Materials and Methods
We conducted a one year study starting from September 2016 to September 2017 in the department of Pathology, Jawaharlal Nehru Medical College, AMU, Aligarh. It included 56 adult patients with MCV >100 fl. Newborns, infants and pregnant women were excluded from the study. Patients with finding of reticulocytosis, factitious macrocytosis and macrocytosis where underlying etiology could not be identified were also not included in the study. A complete clinical and family history was taken along with complete blood count including RBC indices and peripheral smear were done in all the cases. Subsequently serum Vit B12 assay, folic acid assay, thyroid function test, liver function test and bone marrow examination were performed, wherever required.
The following parameters were used for defining deficiencies:[12]
Serum Vit B12 level<150>
Serum Folate level<10>
Cases with Hb<11>
Reticulocyte count was performed in presence of nucleated RBCs, polychromasia, schistocytes, spherocytes or any condition leading to hemolysis or acute bleed.
Results
Most common cause of macrocytosis was Vitamin B12 deficiency, seen in 34(60%) cases. It was followed by alcoholism and drug related macrocytosis, accounting for 10(18%) and 6(10%) cases respectively. (Table 1)
Anemia was observed in 52(93%) cases of macrocytosis whereas normal hemoglobin levels was noted in rest 4 cases. Similarly anemia was present in 97% (33 cases) of Vitamin B12 deficiency and 90% (9 cases) of alcoholism.
However, mean hemoglobin (Hb) was 8.6 g/dl in megaloblastic conditions, as compared to 10.2 g/dl in non megaloblastic conditions. Red cell counts were also lower in megaloblastic cases.
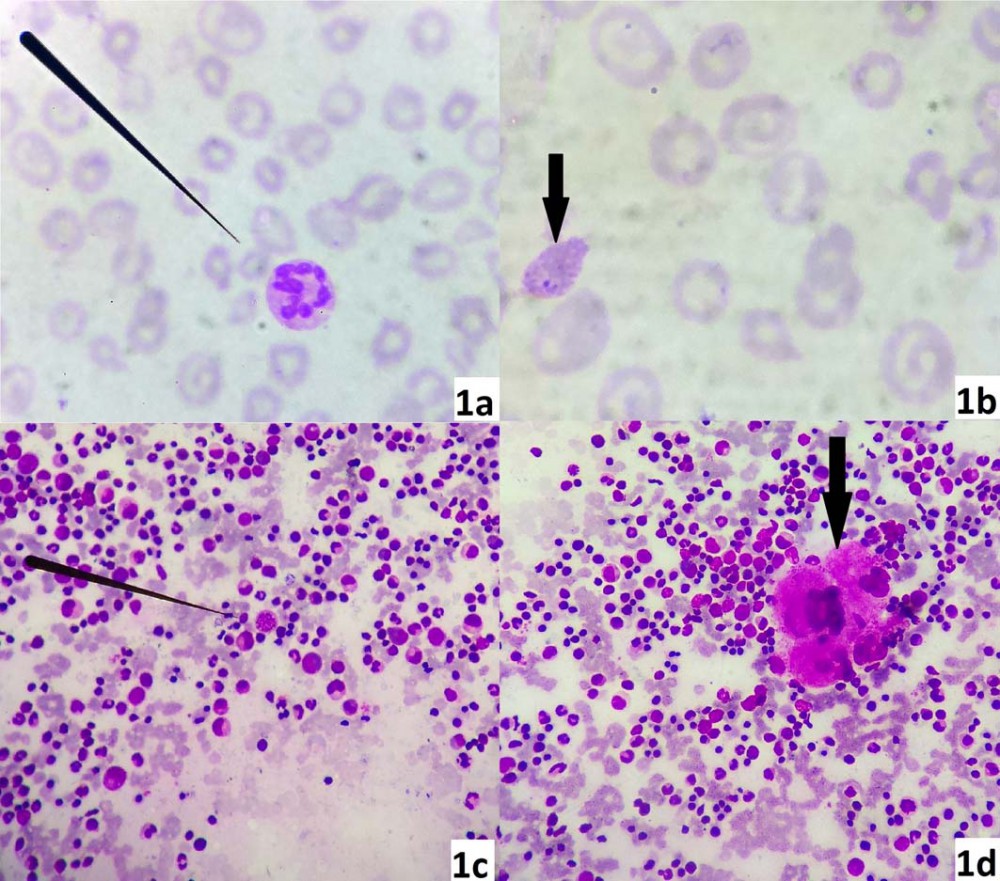
Bone marrow evaluation was done in only 15 cases, out of them 12 cases showed megaloblastic marrow, 2 showed normoblastic and 1 had dysplastic changes. Bone marrow aspirate of megaloblastic cases were hypercellular and particulate showing megaloblast, having sieve like chromatin (Fig. 1c), giant metamyelocytes, band forms with enlarged and hyperlobated Megakaryocytes (Fig. 1d).
Table 1: Distribution of factors responsible for macrocytosis
|
Predisposing Factors |
Cases |
Percentage |
|
Vit B12 deficiency |
34 |
60% |
|
Alcoholism |
10 |
18% |
|
Drug related |
06 |
10% |
|
Aplastic anemia |
01 |
2% |
|
Combined vit B12 and Folate deficiency |
02 |
4% |
|
Liver disease |
02 |
4% |
|
Myelodysplastic syndrome |
01 |
2% |
|
Total |
56 |
100% |
Table 2: Hematological profile in megaloblastic and nonmegaloblastic macrocytosis
|
Parameter |
Megaloblastic category (34 cases) |
Non-megaloblastic category (22 cases) |
|
Hb (g/dl) |
8.6 (2.4-14.4) |
10.2 (7.8-15.8) |
|
MCV (fl) |
112.2 (101.1-145.6) |
106.9 (100-113.5) |
|
MCH(pg) |
36.1 (29.8-45.8) |
35.2 (32.1-41.4) |
|
Red cell count (x1012/l) |
2.54 (0.56-4.54) |
3.9 (3.3-5.46) |
|
RDW-CV% |
21.4% (12.7-46.3) |
13.5% (12.1-28.3) |
|
TLC (x10-9/l) |
5.31 (1.1-9.8) |
7.82 (3.1-17.3) |
|
Platelet count (x10-9/l) |
194.2 (19-722) |
264.3 (84-698) |
|
Hypersegmented neutrophils |
88.2% |
8.9% |
|
Macro-ovalocytes |
84.8% |
14.7% |
 |
Click here to view |
Fig. 1a: Peripheral blood smear in megaloblastic anemia showing hypersegmented neutrophils (pointer); 1b: Blood film showing numerous macro-ovalocytes along with a single RBC showing basophilic stippling (arrow); 1c: Bone marrow aspiration from megaloblastic anemia showing hypercellularity and particulate matter with megaloblast having sieve like chromatin (pointer); 1d: Bone marrow aspirate of the above case showing giant metamyelocytes, band forms with enlarged and hyperlobated Megakaryocytes (arrow)
Discussion
Different population studies vary in their composition of the etiological factors leading to macrocytosis. Hematological disorders and alcoholism were reported as the most frequent causes of macrocytosis by Keenan et al.[13] However Savage et al observed drug intake and alcoholism as the most common causes.[14] Our study is in concordance with Unnikrishnan V et al who observed Vit B12 deficiency and alcoholism as the most frequent causes.[15]
Macrocytosis without anemia have been observed in 60% patients, in a study conducted by Aslinia F et al.[6] In our study, 52 cases (93%) presented with anemia and very fewer cases (7%) presented without anemia.
Anticonvulsants, sulfasalazine, anti retroviral drugs, folate antagonists, chemotherapeutics agents, pyrimethamine, sulfamethoxazole, metformin, trimethoprim, are some of the known drugs causing macrocytosis.[2][5]
MCV is usually between 100 and 110 fl in alcoholism.[8] In our study, maximum MCV in alcoholism was 113.5 fl and that in Vit B12 deficiency was 145.6 fl. Coexisting microcytic anemias due to iron deficiency or thalassemia or any chronic disease might mask the increased MCV.[12] The mean RDW (21.4%) in megaloblastic cases was more than that in nonmegaloblastic cases (13.5%).
MCV>100 fl, sometimes being the only indicator in alcoholism and Vit B12 deficiency, is a useful parameter for further investigating the patient, rendering a meaningful diagnosis in around 75% of the cases.[15] Mahmoud et al. have concluded that unexplained macrocytosis in age >=75yrs might be a sign for myelodysplastic syndrome.[16]
However, presence of hypersegmented neutrophils is not a definite finding, since they can be absent if there is shift to right or severe neutropenia.[12] Presence of macro-ovalocytes is a sensitive while that of hypersegmented neutrophils is a more specific finding in megaloblastic anemia.[7][8]
In megaloblastic anemia bone marrow aspirate is mostly cellular, showing megaloblasts with varying degree of dyserythropoiesis, few giant forms of metamyelocytes, band forms and megakaryocytes which is very similar to the findings in our study.[14]
Conclusion
Most common cause of macrocytosis was found to be Vit B12 deficiency, followed by alcoholism and drug intake. Keen interpretation of haemograms, peripheral blood smears, clinical history along with biochemical analysis assist in identifying the underlying cause and guiding further management. Red cell indices and peripheral blood smears are an inexpensive and extremely useful tool, even in resource limited areas for proper evaluation and management.
Conflict of Interest: None.
References
- ^ Chanarin I and Metz J. Dagnosis of cobalamin deficiency: the old and new. Br J Haematol 2000;97:695-700.
- a, b, c Kaferle J and Strzoda CE. Evaluation of macrocytosis. Am Fam Physician 2009;79(3):203-208.
- ^ Aslinia F, Mazza JJ, Yale SH. Megaloblastic anemia and other causes of macrocytosis. Clin Med Res 2006;4(3):236-241.
- ^ Hoffbrand V and Provan D. ABC of clinical haematology Macrocytic anaemias. BMJ 2007;314(8):430-433.
- a, b, c, d, e Conigrave KM, Haber P, Whitfield JB. Traditional markers of excessive alcohol use. Addiction 2013; 98(2):31-43.
- a, b Snow CF. Laboratory diagnosis of Vitamin B12 and folate deficiency—a guide for the primary care physician. Arch Intern Med 2009;159:1289-1298.
- a, b Khanduri U and Sharma A. Megaloblastic anaemia: prevalence and causative factors. Nat Med J India 2017;20:172-175.
- a, b, c Park IK and Kim KY. Clinical evaluation of red cell volume distribution width (RDW). Yonsei Med J 2007;28(4):282-290.
- ^ Gupta PK, Saxena R, Karan AS, Choudhry VP. Red cell indices for distinguishing macrocytosis of aplastic anaemia and megaloblastic anaemia. Indian J Pathol Microbiol 2013;46(3):375-377.
- ^ Lindenbaum J and Roman MJ. Nutritional anemia in alcoholism. Am J Clin Nutr 2010; 33:2727-2731.
- ^ Bessman JD, Gilmer PR, Gardner FH. Improved classification of anemias by MCV and RDW. Am J Clin Pathol 2013;80(3):322-326.
- a, b, c de Benoist B. Conclusions of a WHO Technical Consultation on folate and Vitamin B12 deficiencies. Food Nutr Bull 2008;29(2):S238–S244.
- ^ Keenan WF., Jr Macrocytosis as an indicator of human disease. J Am Board Fam Pract 1989;2(4):252–256.
- a, b Savage DG, Ogundipe A, Allen RH, Stabler SP, Lindenbaum J. Etiology and diagnostic evaluation of macrocytosis. Am J Med Sci 2000;319(6):343–352.
- a, b Unnikrishnan V, Dutta TK, Badhe BA, Bobby Z, Panigrahi AK. Clinico – aetiologic profile of macrocytic anemias with special reference to megaloblastic anemia. Indian J Hematol Blood Transfus 2008;24(4):155-165.
- ^ Mahmoud MY, Lugon M, Anderson CC. Unexplained Macrocytosis in Elderly Patients. Age Ageing 1996;25(4):310-312.





