Abstract
Introduction: Information on epidemiological profile of supratentorial tumors pathology is scant in developing countries like India hence; more institutional data are needed to know the tumor burden in pediatric population, to undertake necessary research and to improve the therapeutic modalities in any given locality.
Aim: To study the distribution of various supratentorial tumors in pediatric age group according to age, sex, anatomical location and histological type and correlate findings from our institute with other institutional studies.
Materials and Methods: We conducted a retrospective study to analyze the data on archived surgical samples of 45 pediatric patients (0-18 years) with supratentorial brain tumors, operated over a period of 10 years (January 2008 to December 2017). Data regarding age, gender, site of the tumor and histopathology were considered for the analysis. The results obtained were compared with the available published literature data matching to our study on Indian population.
Results: The most common pediatric primary brain tumors occupying supratentorial region were astrocytic tumors (33.3%) followed by craniopharyngiomas (20%) and meningiomas (13.4%). The most common astrocytic tumor was pilocytic astrocytoma. Pediatric brain tumors were more common in males (60%) as compared to females (40%) with male to female ratio of 1.5: 1.
Conclusion: Astrocytomas and craniopharyngiomas were observed to be the common supratentorial tumors among pediatric age group at our institute consistent with other multicentric studies conducted in India.
Keywords: Astrocytoma, craniopharyngioma, Pediatric tumors, Supratentorium.
Introduction
Tumors associated with brain and central nervous system (CNS) in pediatric population of 0 to 18 years of age claim major cause of morbidity and mortality and it was observed that such incidences are higher during the first year of life. Worldwide, CNS tumors account for at least 15-35%,[1] of solid tumors accounting for major cause of death in pediatric cancers after leukemia.[2] In India, brain tumors constitute about 11.4%–20.1% of all childhood tumors.[3][4][5][6] Although, this is not epidemiological data of the country as a whole, but were only institutional incidences. Recent multi‑centered study by Jain A et al (2011)[7] revealed a report with data from 7 top ranked tertiary care centers of India, suggesting that pediatric CNS tumors account for an average of 14.8% (10-20%) of total intracranial tumors. Moreover, global reports indicated that increased incidences of pediatrics CNS tumors especially the brain tumors pose higher mortality rate eventually challenging the neurooncologic fraternity. The exact histological diagnosis and location of CNS tumor is essential not only to predict the prognosis of the patients but also influence the treatment modality while investigating the risk factors. Brain tumors are classified by histology according to World Health Organization (WHO) classification. Glial tumors which are most common type of brain tumors include astrocytoma, ependymoma, glioblastoma, oligodendroglioma, and such others.[8][9] The prognostic outcome of the patients with certain given treatment is not only influenced by histological examination but also the location of the tumor and the associated metastasis. Information on epidemiological profiles of these tumors is scant in developing countries like India hence; more institutional data are needed to understand the tumor burden in pediatric population, to undertake necessary research and to improve the therapeutic modalities in any given locality. The study was done at a tertiary care hospital in Eluru, Andhra Pradesh. The objective of the present study is to assess the distribution of various supratentorial tumors in pediatric age group according to age, sex, anatomical location and histological type and correlate the epidemiology and histological profile at our institute with other institutional studies.
Materials and Methods
This is a retrospective study approved by our Institutional Ethics Committee. Archived data of 45 patients with supratentorial pediatric brain tumors was accessed from the neurosurgery department from January 2008 to December 2017 and diagnosis was verified with pathology department.
Inclusion and Exclusion Criteria
All the patients with the age of ≤18 years operated for supratentorial brain tumors and proven histopathologically positive were only included. All cases with supratentorial pathology due to infections, congenital malformations, trauma or cerebrovascular accidents and patients with recurrent or residual primary tumors or secondary tumors were excluded from the study.
Archived data regarding age, gender, site of the tumor, and histological type, were collected and analyzed. Patients with tumor-like cystic lesion (arachnoid cysts, epidermoid cysts and colloid cysts), space occupying lesion of infectious etiology and vascular malformation were excluded from the study. The hematoxylin and eosin (H&E) stained slides of all 45 cases were studied and categorized according to the World Health Organization (WHO) classification of brain tumors. The results obtained were compared with available other Indian population data.
Results
In the present study of 45 supratentorial tumor cases, males (60%) are predominant when compared to females (40%) with male/female ratio of 1.5:1 as shown in table 1. Age group of patients varied from 1 month to 18 years. The general age distribution was as follows: 0-5 years : 8 (17.8%), 6-10 years: 8 (17.8%), 11-18 years: 29 (64.4%), the mean age being 12.65 years (33.33%). Among all age groups except 0-5 years, male preponderance was seen and most of the patients were in the age group 11-18 years. In the current study, the most common anatomical site in supratentorial region was cerebral hemispheres (48.9%) followed by sellar region (31.1%), ventricles (15.6%) and thalamus (4.4%).
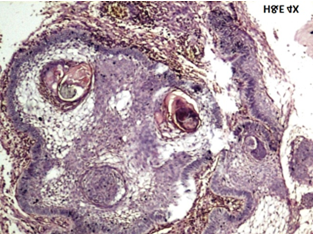
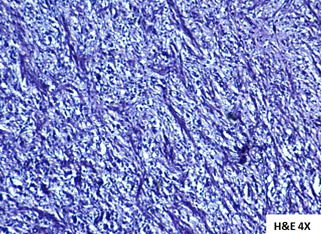
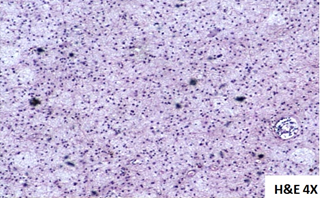
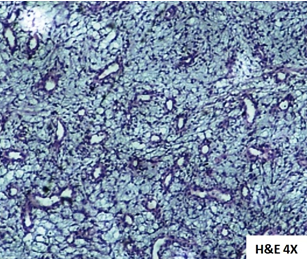
Comparing the histological subtypes of pediatric brain tumors revealed that astrocytoma was the commonest tumors in supratentorial region with an average highest incidence of 33.3%. Craniopharyngioma (20%) (Fig. 1) was the second most common tumors followed by meningioma (13.4%). Less common entities included mesenchymal, mixed neuroglial and embryonal tumors constituting 2.2% each. Among the astrocytomas, WHO Grade I tumors pilocytic astrocytomas (Fig. 2) and sub-ependymal giant cell astroytoma (SEGA) were more common (33.3%) followed by Grade II diffuse and pilomyxoid astrocytomas (Fig. 3 & 4) and Grade IV (GBM) accounting for 26.7% each. Low grade astrocytomas (grade I & II) were common in the age group 0-10 years and high grade astrocytomas were predominant in the age group of 11-18 years. Overall, Astrocytoma was the predominant histologic type among all the age groups. Craniopharyngioma was the second most common type in 11-18 years age group.
Table 1: Clinico pathological presentation of the cases
|
Variable |
No of Cases (n=45) |
in % |
|
Gender |
||
|
Males |
27 |
60 |
|
Females |
18 |
40 |
|
Age (Years) |
||
|
0-5 |
08 |
17.8 |
|
06-10 |
08 |
17.8 |
|
11-18 |
29 |
64.4 |
|
Location of the tumor |
||
|
Cerebral Hemisphere |
22 |
48.9 |
|
Sella |
14 |
31.1 |
|
Ventricles |
07 |
15.6 |
|
Thalamus |
02 |
4.4 |
|
Histology Type |
||
|
Astrocytomas |
15 |
33.3 |
|
Craniopharyngioma |
09 |
20 |
|
Meningioma |
06 |
13.4 |
|
Glioma |
05 |
11.1 |
|
Pituitary adenomas |
04 |
8.9 |
|
Ependymoma |
03 |
6.7 |
|
Embryonal tumor |
01 |
2.2 |
|
Mixed neurological tumor |
01 |
2.2 |
|
Mesenchymal tumors |
01 |
2.2 |
|
Grade of the tumors |
||
|
Grade I (Pilocytic+SEGA) |
15 |
33.30 |
|
Grade II (Diffuse+Pilomyxoid) |
12 |
26.70 |
|
Grade III |
06 |
13.30 |
|
Grade IV |
12 |
26.70 |
 |
Click here to view |
Fig. 1: Craniopharyngioma
 |
Click here to view |
Fig. 2: Pilocytic astrocytoma
 |
Click here to view |
Fig. 3: Diffuse astrocytoma
 |
Click here to view |
Fig. 4: Pilomyxoid astrocytoma
Discussion
Supratentorial pediatric brain tumors are a heterogeneous group of neoplasms and are leading cause of cancer related deaths in children. In our study, the most common supratentorial pediatric brain tumors were male preponderance 60%, whereas females were 40%. Of 45 supratentorial cases, 64.4% of patients were in the age group 11-18 years and 36.6% of the patients were in ≤ 0-10 years of age group.[10]
49% of the tumors were cerebral hemispheric in location followed by sella (31.1%), Ventricles (15.6%) and Thalamus (4.4%). Our results are consistent and in agreement with the findings of Vinay kumar et al (2014)[11]and Mohan Rao et al (2014)[10] that demonstrated the predominance of cerebral hemispheres location over other regions, pertaining to supratentorial cases.
Overall, 33.3% of the cases were astrocytomas followed by craniopharyngioma, meningioma, glioma, pituitary adenoma, ependymoma and one case in each histology type of embryonal, mixed neurological and mesenchymal tumors. As per our data and accumulated literature available from various other clinical studies from India, we observed that astrocytomas are most predominant and prevalent in supratentorial tumors. Our results are in close correlation with other Indian hospital based studies,[11][12][13] in assigning second place for Craniopharyngiomas and third place for meningioma. Meningioma data was consistent with western studies along with Indian studies which occupies the prevalence as third most common tumors.[7][14]
Among 45 cases of supratentorial tumors, 33.30% of cases were Grade I (Pilocytic +SEGA), 26.70% of the cases were Grade II (Diffuse+Pilomyxoid) falling under the age group of 0-10 years and 13.30% cases are Grade III and 26.70% Grade IV tumors falling under the age group of ≥ 11 -18 years respectively. We found that grade I tumors are highly predominant and Grade II and Grade IV are in equal prevalence in nature whereas Grade III tumors are less prevalent. Our results were consistent with other Indian patient data where low grade tumors exhibited more prevalence than high grade tumors. [11][10]
This clinically relevant data potentially estimates the disease prevalence for assessing the epidemiological disparities associated with the patterns of supratentorial tumors of pediatric population. This data is much needed in healthcare system to ascertain the required modality for efficient management of disease.
Conclusion
The present study not only showed the prevalence of disease, but also revealed the consistency in the frequencies of foremost histology patterns and grade of the tumors which were with complete agreement with the clinical data from other Indian hospitals. We strongly believe that our study adds to the requirement of much needed initiatives by the health care sector for planning and distribution of needed infrastructures and necessary deliberate efforts in the management of pediatric supratentorial brain tumor burden in India.
Financial Support and Sponsorship: Nil
Conflicts of Interest: No
References
- ^ Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. “Cancer statistics, 2006”. CA Cancer J Clin 2006;56:106-130.
- ^ Rosemberg S, Fujiwara D. “Epidemiology of pediatric tumors of the nervous system according to the WHO 2000 classification: A report of 1,195 cases from a single institution”. Childs Nerv Syst 2005;21:940-944.
- ^ Nandakumar A, Anantha N, Appaji L, Swamy K, Mukherjee G, Venugopal T, et al. “Descriptive epidemiology of childhood cancers in Bangalore, India”. Cancer Causes Control 1996;7:405‑410.
- ^ Kusumakumary P, Jacob R, Jothirmayi R, Nair MK. “Profile of pediatric malignancies: A ten year study”. Indian Pediatr 2000;37:1234‑1238.
- ^ Swaminathan R, Rama R, Shanta V. “Childhood cancers in Chennai, India, 1990‑2001: Incidence and survival”. Int J Cancer 2008;122:2607‑2611.
- ^ Arora RS, Eden TO, Kapoor G. “Epidemiology of childhood cancer in India”. Indian J Cancer 2009;46:264‑273.
- a, b Jain A, Sharma MC, Suri V, Kale SS, Mahapatra AK, Tatke M, et al. “Spectrum of pediatric brain tumors in India: A multi‑institutional study”. Neurol India 2011;59:208‑211.
- ^ Aryal G. “Histopathological pattern of central nervous system tumor: A three year retrospective study”. J Pathol Nepal 2011;1:22‑25.
- ^ Masoodi T, Gupta RK, Singh JP, Khajuria A. “Pattern of central nervous system neoplasm: A study of 106 cases”. JK Pract 2012;17:42‑46.
- a, b, c Mohana Rao P, Suchanda B, Aniruddh Kumar P. “Outcome of supratentorial intraaxial extra ventricular primary pediattric brain tumors: A prospective study”. J Pediat Neurosci 2014;9:216-220.
- a, b, c Vinay kumar DP, Akshata M, Deb Kumar Boruah, Gogoi R.K, Skandesh B M, Arjun Prakash, et al. “CT Evaluation of pediatric supratentorial tumors”. IOSR J Dent Med Sci 2014;13: 87-108.
- ^ Margam SR, Gadgil NM, Kshirsagar GR, Gaikwad VP, Kumavat PV, Chaudhari CS. “The Histopathological and epidemiological study of pediatric brain tumors in a tertiary care hospital, Mumbai”. Ann Pathol Lab Med 2016;3:374-381.
- ^ Madhavan R, Kannabiran BP, Nithya AM, Kani J, Balasubramaniam P, Shanmugakumar S. “Pediatric brain tumors: An analysis of 5 years of data from a tertiary cancer care center, India”. Indian J Cancer 2016;53:562-565.
- ^ Shah H, Ubhale B, Shah J. “Demographic and histopathologic profile of pediatric brain tumors: A hospital-based study”. Pediatr Oncol 2015;4:146-148.





