Salivary gland tumors: Features not to be missed on cytology. A study of five cases
Article Type : Null
Author Details:
Volume : 4
Issue : 1
Online ISSN : 2581-3706
Print ISSN : 2581-3714
Article First Page : 50
Article End Page : 53
Abstract
Fine needle aspiration cytology (FNAC) plays a crucial role in the diagnosis of salivary gland lesion and hence advantageous to patient and treating surgeon since it is safer and faster than excision biopsy. Interpretation of cytological findings is difficult in salivary gland tumors because of many pitfalls like uncertainty as to the site, aspiration material, lack of architectural patterns and mainly overlapping cytological features. In our study we have discussed pitfalls of FNA cytology of salivary gland tumors in five discordant cases. We discuss five such cases were cytological diagnosis was missed due to numerous factors. An insight into technical and interpretational factors is discussed.
Keywords: Cytology, Salivary gland tumors, Pitfalls in cytology.
Fine Needle Aspiration Cytology (FNAC) of salivary gland has a wide-range of diagnostic sensitivity (62-97.6%) and specificity (94.3-100%).[1]Because of superficial location and easy accessibility, FNAC is a simple and inexpensive technique for diagnostic evaluation of these tumours.[2] Owing to lack of characteristic clinical and radiological features that are specific for particular diagnosis, FNAC assumes greater significance in diagnosing salivary gland tumors.[1]
Factors such as uncertainty of site, tissue actually aspirated, aspiration of minimal material, lack of architectural pattern in smears have a huge impact on specific cytological diagnosis.[3]The aim of the present study is to discuss cytological pitfalls in specific diagnosis of some types of salivary gland tumors.
Institutional ethical clearance was taken before start of the study. At our centre routinely tumour aspirations were performed by the standard procedure using 21gauge - 23 gauge needle and 10 ml syringe. Patients were subjected to repeat aspiration if initial aspirate was found to be inadequate for interpretation. Air dried smears were stained with Giemsa stain and alcohol fixed smears were stained with Papnicoloau (PAP) and Hematoxylin and Eosin (H&E) stains. Excised tumors are grossed according to standard protocol. Tissue bits are processed, paraffin blocks were made. 5 micro meter thick sections are then stained with Hematoxylin and Eosin stain. Special stains were done whenever required. In this retrospective analysis of cases cytology records of two years from June 2015 to June 2017 were audited and two hundred and nine (209) cases of salivary gland aspirations were analyzed. Five cases of salivary glands tumors in which cytology and histopathology diagnosis did not correlate were studied.
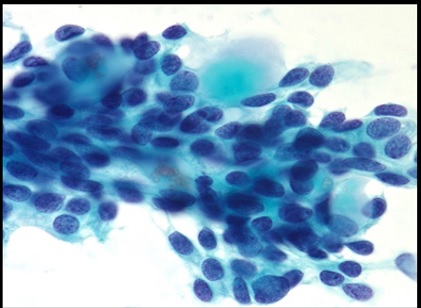
Case 1: 65year male patient with swelling in Left hard palate since 2 months. Aspirates showed A diagnosis of Adenoid cystic carcinoma (ACC) was made on cytology due to presence of hyaline globules surrounded by tumor cells having scant cytoplasm, monomorphic nuclei, coarse chromatin and prominent nucleoli with nuclear moulding in few cells (Fig. 1).
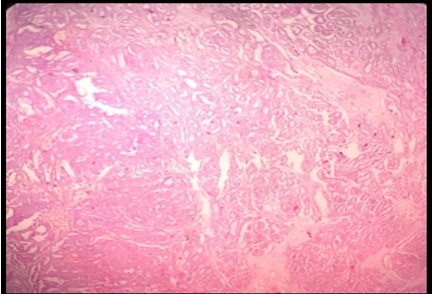
On histopathology presence of diversed growth patterns and uniform, bland cytologic features diagnosis of Polymorphous Low Grade Adenocarcinoma was made (Fig. 2).
When cytology slides were reviewed back; tumor cells had variable cytomorphic patterns like single cells, small cohesive ductal groups and trabecules. Cells were monomorphic, cuboidal to columnar cells with moderate amount of pale eosinophilic cytoplasm, round to oval nuclei, with open, finely stippled chromatin and indistinct nucleoli. These cells were mistaken for basaloid cells with angled and hyperchromatic nuclei of ACC. Hyaline globules seen on cytology smears also mislead in making interpretation of ACC.
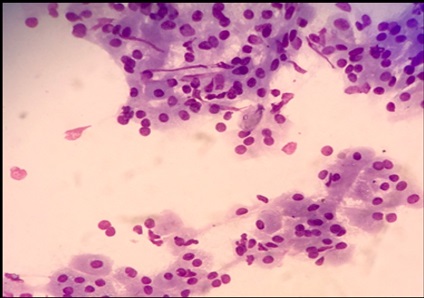
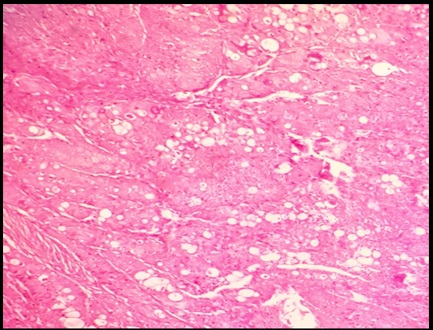
Case 2: 64year male patient with bilateral swelling in parotid glands. On cytology differential diagnosis of Warthin’stumor and Oncocytoma was given due to the presence of benign oncocytic cells in papillary clusters, sheets and singles in a background of scant lymphoid cells (Fig. 3). On histopathology polygonal cells with abundant clear cytoplasm, eccentric placed nucleus having vesicular nuclei was seen. These cells were arranged in lobules, and was seen infiltrating between the normal acinar cells. Hence a differential diagnosis of Clear cell variant of acinar cell carcinoma, Clear cell variant of oncocytic carcinoma was made. On seeing cytology smears again, it was discovered that cells were not truly oncocytes as the cytoplasmic granularity was not as fine or tightly packed as that seen in a true oncocytes (Fig. 4).
Case 3: 28year male patient treated for Mucoepidermoid carcinoma came with nodular growth from left parotid region of 4 months duration. Aspirate contained thick abundant mucoid material with numerous cyst macrophages. No definite malignant cells were seen. A cell block prepared from left out material did not reveal any tumor cells. On histopathology of the nodular area revealed small foci of low grade mucoepidermoid carcinoma. A focus of mucoepidermoid carcinoma was missed on cytology.
Case 4: 70 year male patient with swelling in the right side of neck since 1 month. On repeated FNAC, we aspirated only cyst fluid with hypocelluar smears only. Hence a definitive diagnosis could not be given based on FNA. A diagnosis of Warthin‘s tumor was made on histopathology. Only cystic areas were aspirated and solid area was not needled on cytology.
Case 5: 60year male patient presented with swelling on the left cheek since 3 months. Diagnosis of Monomorphic Adenoma was made due to presence of monomorphic epithelial cells arranged in acinar patterns with scant inflammatory infiltrate.(Fig. 5) On histopathology Mucoepidermoid carcinoma was diagnosed due to presence of sheets of epidermoid cells, intermediate cells and mucous cells. Diagnosis of dysplasia was missed on aspirated cells which lead to wrong diagnosis of Monomorphic adenoma. (Fig. 6)
 |
Click here to view |
Fig. 1: Cytology features showing monomorphic cells admixed with hyaline globules- Adenoid cystic carcinoma (May Grunwald Giemsa stain, 40 X 100 Magnification).
 |
Click here to view |
Fig. 2: Histopathology section showing diversed growth pattern of tumor cells- Polymorphous Low Grade Adenocarcinoma. (Haematoxylin and Eosin stain, 10 X Magnification)
 |
Click here to view |
Fig. 3: Benign oncocytic cells on cytology- Differential diagnosis of Warthin’s tumor and Oncocytoma. (Haematoxylin and Eosin stain, 10 X Magnification)
 |
Click here to view |
Fig. 4: Histopathology sections shows polygonal tumor cells arranged in lobules of varying sizes- differential diagnosis of Clear cell variant of acinar cell carcinoma, Clear cell variant of oncocytic carcinoma. (Haematoxylin and Eosin stain, 10 X Magnification)
 |
Click here to view |
Fig. 5: On cytology epithelial cells arranged in acinar patterns- Monomorphic Adenoma (May Grunwald Giemsa stain, 10X Magnification)
 |
Click here to view |
Fig. 6: On histopathology sheets of epidermoid cells along with areas of intermediate cells and mucous cells- Mucoepidermoid carcinoma (Haematoxylin and Eosin stain, 10 X Magnification).
Salivary gland tumors constitute 5-15%of all tumors with pleomorphic adenoma being most common benign tumor, and mucoidepidermoid carcinoma being the most common malignant tumor.[1]Diversecytomorphogical patterns and overlapping features projects a diagnostic challenge to pathologist to give a precise diagnosis. As they say “Forewarned is forearmed”, by being aware of few specific diagnostic difficulties in salivary gland cytology one can avoid these errors.[4]
Polymorphous Low Grade Adenocarcinoma is an uncommon salivary gland tumor which requires interpretation of architectural patterns for correct diagnosis that may be missed on cytology.[5]Cytologically, PLGA is characterized by variable cytomorphological patterns like tumors arranged in singles, papillae, small cohesive ductal groups and trabeculae. Though papillarygroup’s aidsin distinguishing PLGA from ACC they may not be found in all cases.Presence of hyaline globules prompted us to make a diagnosis of ACC.[4][5],[6]Literature analysis revealed that hyaline globules are not pathognomic of ACC. Presence of cylindrical and finger like structures, few basaloid cells with well-preserved cytoplasm, angulated nuclei, coarse nuclear chromatinare some of thediagnostic features of ACC.[7],[8]Hyaline globules are not indigenous to ACC, they can also be encountered in smears of other benign tumors like Basal cell adenoma, malignant tumors like in PLGA and Epitheial-Myoepitheial carcinoma.[9]Though cytological features of PLGA overlap with Low grade ACC, nuclear chromatin of cells in PLGA are deceptively bland compared with that of ACC.[9] Because of these cytomorphologicoverlap between PLGA and ACC, distinction among them will be challenging.
As hyaline globules can be seen in many variants of salivary gland tumors, they are not pathognomonic of any tumor of salivary glands. Close attention to minute cellular morphological details will avoid wrong diagnosis.[9]
In second case only oncocytes were aspirated which leads to wide spectrum of benign and neoplastic salivary gland lesions presenting with oncocytic or oncocyte like features. Warthin s tumor composed with true oncocytic cells in highly cohesive clusters and low to moderate nuclear grades.[4] Nearly 80% of Warthin s tumor can be diagnosed based on cytological features by FNA, Oncocytic variant of WT, subset of WT exhibits variationsdepending on presence of predominant cell population whether lymphocyte or oncocytes. These can pose diagnostic problems in poorly sampled cases.[10]
Classic Aciniccell carcinomas are polygonal cells with abundant delicate vacuolated cytoplasm that range from slightly basophilic to eosinophilic. Background of ACC usually clean and approximately 10% of subset will have mixed lymphoid including lymphohistiocytic aggregates.[4]
In second case clear cell changes in oncocytes were misinterpreted and a differential diagnosis of clear cell variant of acinic cell carcinoma was considered. Most common diagnostic challenges with oncocytic cytological picture differentiating the benign tumor, Oncoytomaandoncocytic predominant Warthin’s tumor from Low grade carcinomas with oncocytic predominance, ACC. At low magnification, these entities appear similar, but at higher magnification and Romanowsky stain shows acinic cells having delicate cytoplasm with small vacuoles that are PAS+ Diastase while Oncocytoma or oncocytes predominate Warthin’s tumor have densely granular to waxy appearing cytoplasm without vacuoles and shows PTAH positivity, a stain for mitochondria.[4],[10]
Cystic lesions are estimated to account for up to 8% of all salivary gland tumors. The overall diagnostic accuracy of FNA for the evaluation of cystic salivary gland lesions is approximately 40%, this is mainly because of sample adequacy problems.[4] The most common causes of false negative FNA of cystic lesions is low grade Mucoepidermoid carcinoma since most of the times aspiration shows only cystic contents.[4]Pauicellularity due to sampling error or cyst fluid diluting the tumor cells, presence of occasional mucus cells, mucinous background and lymphocytes contribute to this underdiagnosis.[11] The epithelial cells are cytologically bland and mucin containing cells can easily be misinterpreted as histocytes or mucinophages. These mucus cells haveeccentrically placed indented nucleus, low N: C ratio, presence of abundant delicate pale staining mucoid cytoplasm, whereas foamy histiocytes and muciphages have more multivacuolated cytoplasm with centrally place round nucleus.[12] When aspirating mucinous cyst, it is important to always aspirate any residual solid mass that remains after the successive FNA.[4],[10],[11],[13]
The second most common errors of cystic lesions of salivary gland tumors of cytology misinterpretation are Warthin’s tumor. Main problem in interpretation may be due to relative lack of classical features of Warthin’s tumor, if sparse material obscured by inflammation and debris along with cyst macrophages.[11]In both the scenarious, ultrasound guided FNA is very useful, aspiration of solid areas, in combination with clinical correlation helps to minimize false negative cases.[14],[15]
Monomorphic adenoma of salivary gland exhibits exceptional cytomorphologic diversity including a wide variety of metaplastic changes, which may pose diagnostic challenges.[16]Monomorphic adenoma represents a heterogenous group of tumor with wide variety of cytomorphologicalthat depends on type of cell, cellular arrangement and embryologic development. In our case predominance of epithelial, limited or no matrix component, lack of dense cytoplasm, moderate focal nuclear atypia mislead to diagnosis of monomorphic adenoma.[16]Usually epithelial predominant aspirates raise a diagnostic difficulties in salivary gland on cytology, cytopathologist should be aware of broad spectrum of entities with biphasic morphology including both benign and malignant salivary gland tumors, because of potential for discrepant diagnosis.[4],[16],[17]
Conclusion
In conclusion pitfalls in specific diagnosis of salivary gland tumor on FNAC may be overcome by looking into technical as well as non-technical aspects of diagnosis. Technical aspects such as multiple aspirations, techniques like guided FNAC and cell block preparations can help us in subtyping of salivary gland tumors. Added to this a thorough examination of all smears by pathologist under a strong basis of clinical suspicion of malignancy will have additional value in clinching diagnosis. In the absence of arriving at definitive diagnostic characteristics, only detailed descriptive and probable differential diagnosis can be entertained.
Conflict of Interest: None.
Doi No:-10.18231/2581-3706.2019.0009