Introduction
Fractures of the tibia, one of the most commonly occurring long bone fractures, are particularly prevalent due to its location just beneath the skin.1 Males are affected approximately three times more frequently than females, and the average age of patients experiencing these fractures is around 37 years.2, 3
Among adults, distal metaphyseal fractures of the tibia, with or without extension into the joint, throws a formidable challenge to Orthopedic surgeons.4 The clinical outcome is influenced by several critical factors, including the type of fracture, associated soft tissue injury, treatment method, and the quality of realignment.
Determining the optimal treatment strategy for distal tibial fractures has been a subject of ongoing debate among orthopedic surgeons. There are various treatment strategies and options of implants available. Each technique has its own set of advantages and disadvantages. Recent studies indicate that MIPO may be a superior method; however, it is not without limitations, as it requires technical proficiency and may not always achieve direct realignment of fractured fragments. Our study aims to compare anterolateral plating with medial plate in distal tibia fractures.
Materials and Methods
After due approval from hospital scientific and ethical committee a prospective study was conducted at NIMS Hospital from July 2019 to May 2021. Patients were enrolled in study after taking required consents for the study. A total of 36 patients who met the inclusion criteria were enrolled, operated and followed up periodically. Patients who had anterolateral plate and medial plate were divided into group A and B respectively. Group A had 22 and Group B had 14 patients. The inclusion criteria included patients above 18 years of age of both sexes with closed or compound Grade I fractures. Patients with compound Grade II and III fractures, chronic moribund conditions, pathological fractures, and those unwilling to participate were excluded. Upon admission, standard ATLS protocol was observed and anteroposterior and lateral radiographs of the ankle joint and full-length tibia were taken, with additional oblique views if necessary. In cases where fracture geometry assessment was insufficient, CT scan with 3-D reconstructions was performed. Fractures were classified according to the OTA5 classification system. All procedures were performed under regional anesthesia by the senior surgeon himself or under his direct supervision. The anterolateral and medial plating was performed by standard anterolateral and medial approach respectively. The associated fibula fracture received fixation using a one-third tubular or recon plate through a lateral or poster lateral approach to the fibula.
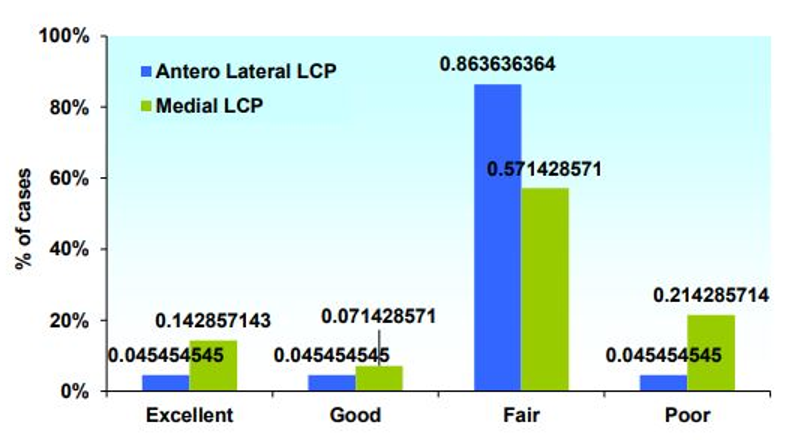
Patients were followed up at regular intervals, including at 6 weeks, 18 weeks, 24 weeks, 36 weeks, and 48 weeks after surgery. At each follow-up, clinical and radiological assessment was performed. Functional scoring was performed at each follow up and any complications if seen were noted. Tenny and Wiss6 functional score which is a 100-point scale grading the results as excellent, good, fair and poor was used for functional scoring. Superficial infections, deep infections requiring debridement, wound dehiscence and neurovascular injuries were classified as early complications while hardware prominence, implant failure, malunion and nonunion requiring secondary surgeries were classified as late complications. Data was analyzed using the Statistical Package for the Social Sciences (SPSS) software. A p-value of less than 0.05 was considered statistically significant.
Observations and Results
The study included a total of 36 patients with distal tibial fractures, and the average age of the participants in group A and group B was 40.5 years and 36 years, while overall average age was 38.78 years, with a standard deviation of 9.09 years. Among the participants, 83.3% were male, while 16.7% were female. The fractures were evenly distributed between the left and right sides, with each side accounting for 50% of the cases. Road traffic accidents were the most common mode of injury, accounting for 61.1% of the cases. Falls were responsible for 38.9% of the fractures.
The fracture characteristics were classified according to the OTA classification system. The distribution of fractures was as follows: A1 - 13.9%, A2 - 47.2%, A3 - 19.4%, C1 - 19.4%. Associated fibular fractures were seen in 88.9% of the participants.
The majority of fractures seen in patients (n=28, 77.8%) were closed, grade 1 compound fractures were seen in 8 (22.2%) patients.
The mean interval between injury and surgery was 8.50 ± 3.62 days. The majority of patients (50%) underwent surgery between 5 to 7 days after the injury. The 22 patients (61.1%) underwent anterolateral approach, and 14 patients (38.9%) had the medial approach and had anterolateral LCP and medial locking LCP respectively
Number of early and late complications were 3(13.63%) and 2(9.09%) in group A while 8(57.14%) and 2(14.29%) in group B respectively with a p value of <.05 suggesting significant association of higher early complications in group B. The mean time taken for patients to achieve full weight-bearing and radiological union was 17.4 weeks in group A and 18.2 weeks in group B. Mean functional score5(Tenny & Wiss score) was 80.82 in Group A and 78.50 in Group B with a p value of 0.523 which was not statistically significant. This score corresponds to a ‘fair’ outcome, suggesting that the majority of patients achieved moderate functional outcomes following surgical intervention. No significant correlations were found between OTA fracture classification and outcomes, as indicated by the p-values (>0.05) for each fracture classification. This suggests that the type of fracture classification did not significantly impact the clinical outcomes in this study population. Similarly, no significant correlations were observed between the implant used and functional outcomes. The p-values (>0.05) for each outcome category indicate that the choice of implant did not have a significant effect on the functional outcomes in this study population.(Figure 1)
Discussion
With the advancement of locking plate technology and a better understanding of the soft tissue envelope surrounding the distal tibia, there has been a resurgence in the use of open reduction and internal fixation with pre-contoured locking plates. The aim of this study was to evaluate the outcomes associated with the use of pre-contoured anterolateral and medial locking plates in the management of distal tibia fractures and compare among them and with the existing literature.
The mean age of patients in our study who sustained distal tibia fractures was 38.8 years, with a standard deviation of 9.09 years. This is comparable to the mean age of 38.3 years reported in studies by Vallier H A et al. 7 and Redfern D J et al. 8 These findings highlight that distal tibia fractures predominantly affect the younger and economically productive segment of society.
Out of the 36 patients, 30 (83.3%) were male and 6 (16.7%) were female. Jyotish K et al.9 reported 73.3% male patients and 26.7% female patients while Rakesh K Gupta et al.10 found that 79% of their patient cohort consisted of men.
Our study revealed that 61.1% of fractures were caused by road traffic accidents, 22.2% resulted from falls from height, and 16.7% were due to simple falls or low-energy trauma. These findings are consistent with studies by Pierre Joveniaux et al. 11 and Ghulam Shabbir et al.12 who also reported road traffic accidents and falls from height as the primary causes of distal tibia fractures. These findings emphasize the importance of preventive measures to reduce the incidence of such injuries.
Most of the fractures in our study were classified as extra-articular in nature, with OTA 43 A2 type fractures being the most common (47.2%). This is in line with the literature, as various authors have also reported a higher incidence of extra-articular fractures in distal tibia fractures.
The majority of patients in our study (88.9%) had an associated fibular fracture, highlighting the importance of stabilizing the fractured fibula to maintain tibial length, control rotational forces, and prevent malunion and post-traumatic ankle arthritis. This finding is consistent with the study by Yih-Shiunn Lee et al.13 which emphasized the significance of fibular osteosynthesis in the management of these fractures.
The mean time interval between injury and surgery in our study was 8.5 days, with most patients undergoing surgery within 10 days of the injury. This timeframe is similar to the study by Shreshta D et al.14 which reported an average interval of 4.45 days. These findings suggest that tissue edema settles and the condition of the skin improves within this time frame, allowing for safer surgical intervention. Skin condition assessment revealed that none of the patients had unhealthy skin pre-operatively, but 9 patients developed unhealthy skin on the third post-operative day, which reduced to 7 patients at the time of stitch removal. This indicates the importance of careful handling of the tissue envelope to prevent complications such as infection.
The average duration of radiological union in our study was 17.4 weeks in group A and 18.2 weeks in group B. These findings are consistent with studies by Aksekili et al.15 which reported mean union times of 18.5 weeks and 20.7 weeks, respectively. These results underscore the need for patience during the healing process and highlight the importance of monitoring radiological signs of union.
Regarding complications, our study found a higher rate of both early and late complications in the medial plating group compared to the anterolateral plating group. Superficial infection was the most common immediate complication observed in both groups. These findings align with the literature which reports a higher rate of superficial infection in the medial plating group.
The mean clinical score in our study indicated a fair outcome in both the anterolateral plating and medial plating groups. This finding is consistent with the study by and Garg S et al.16 which reported better functional scores for lateral plating techniques. These results suggest that both approaches can yield good functional outcomes in the treatment of distal tibia fractures.
Conclusion
The use of pre-contoured locking plates in the management of distal tibia fractures has shown promising outcomes. Both medial plating and anterolateral plating techniques can achieve good functional outcomes, although the rate of complications is higher in the medial plating group. Anterolateral plating offers advantages and a lower complication rate compared to medial plating. However, further research with larger sample sizes and longer follow-up durations is needed to establish standardized treatment protocols and gain a deeper understanding of distal tibia fractures.