Introduction
Hyperglycemia (fasting plasma glucose 126 mg/dl and/or 200 mg/dl two hours after ingesting 75 g of glucose), glycosuria, hyperlipidaemia, a negative nitrogen balance, even ketoacidosis and other metabolic abnormalities are the hallmarks of diabetes mellitus.1, 2
In type I diabetes, beta cells are destroyed, which results in a complete lack of insulin. Most situations fall into one of two categories: Insulin shortage, insulin secretory disorder, and insulin resistance are all related in diabetes (type 2). The condition currently affects about 382 million people globally, but experts project that number will climb by the year 2035, to 592 million. Organization for World Health (WHO) estimates that up to 79.4 million people could be affected by DM by 2030. This is anticipated as a result of the concurrent rise in emerging countries' urban population, which will increase from 1.9 billion in 2000 to 3.9 billion in 2030.3 In different states of India, the incidence of polypharmacy ranges from 5.82% to 93.14%.
Most diabetic patients have at least one co-morbidity, and 40% of them have a minimum of 3 co-morbidities.4 Type 2 DM is linked to a number of co-morbid conditions, including cardiovascular diseases, hypertension, and hyperlipidaemias. About 70% of diabetic patients have hypertension, or raised blood arterial pressure, and diabetic patients have a twice as high chance of developing hypertension as euglycemic people.5 Dyslipidaemia has been proven to raise the risk of cardiovascular problems and is frequently linked to diabetes. According to a 2013 study conducted in Gujarat, India, 15.41% of patients were given the hypolipidemic medication atorvastatin; nevertheless, diabetic patients must also get antiplatelet therapy to lower their risk of ischemia.6
Diabetes mellitus and psychological comorbidity: A need for early diagnosis and therapy. Diabetes mellitus and psychological comorbidity: A need for early diagnosis and therapy. It is well-recognised that psychological problems and diabetes can exacerbate one another. Diabetes is a prevalent ailment. It is crucial to understand the negative effects that each illness has on the other because they frequently coexist, making it possible to manage both of these conditions successfully. Diabetes has a substantially greater frequency of depression and anxiety than the general population, with some studies reporting rates between 12 and 28%.7 Thyroid conditions, celiac disease, and vitamin B12 insufficiency are the three most common autoimmune comorbidities linked to type 1 diabetes.
With so many current therapy options, polypharmacy is unavoidable when managing a common chronic ailment like diabetes. Throughout time, as more therapeutic choices become accessible, the likelihood of polypharmacy will raise.8 When compared to patients with diabetes, diabetics with co-morbidities experience a greater annual economic burden. The 60% of patients in the research with 132 participants are hospitalised with comorbidities and are financially burdened by hospitalisation, travel, and other expenses like the cost of diagnostic.9
As there aren't many studies in this area, the current study's objectives are to assess co-morbidities in type 2 DM patients and current trends in antidiabetic medication use in type 2 DM patients.
Materials and Methods
It was a cross-sectional study that was conducted in a tertiary care medical facility's outpatient department of medicine. The study duration is of six months from July 2022 to December 2022. Prior to the study, ethic committee approval was taken.
The details of patients attending the outpatient department of medicine having diabetes mellitus with associated comorbidities are recorded in a case record form.
According to the source, the expected probability of at least one morbidity is 83%.
The formula for sample size is n=4pqL2, α =5%, β =20%.
So, the required sample size = 74
Results
We examined the prescriptions written for 80 type 2 DM patients who were receiving antidiabetic medications together with additional concurrent medications for comorbidities during the study period. The study's participants range in age from 31 to 90. 32 (40 %) were female and 48 (or 60%) were male. 53 (66.2%) of these patients were between the ages of 51 and 70, followed by 17 (21.2%) patients between 71 and 90 years old, and 10 (12.5%) patients between the ages of 31 and 50, as below in Table 1.
Table 1
Age wise- distribution of patients
|
Age (in years) |
No. of patients |
Percentage |
|
31-50 |
10 |
12.5 |
|
51-70 |
53 |
66.2 |
|
71-90 |
17 |
21.2 |
|
Total |
80 |
100 |
Table 2
Patients with other comorbid conditions
Patients with DM experience a variety of comorbidities. According to the current study, 58.7% of patients had hyperlipidemia and 82.5% of patients had hypertension., 46.2% from cardiovascular conditions, 40% from obesity & 30% from gastrointestinal disorders followed by others as shown in Table 2.
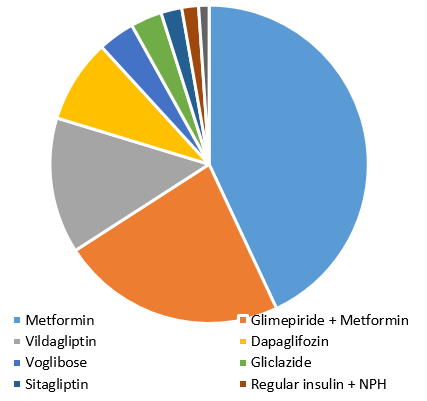
Metformin, which was prescribed to type 2 diabetic patients the most frequently (81%), was followed by glimepiride+Metformin 43%, Vildagliptin 26%, Dapaglifozin 16%, Voglibose in 7%, Gliclazide in 6%, Sitagliptin in 4%, regular insulin +NPH in 3.2% & glargine in 2% as shown in Figure 1.
Discussion
DM is frequently linked to both diabetic and non-diabetic related problems which increases the number of prescription medications. It not only increases the number of drugs but also the adverse drug reactions and chances of drug interactions. The present study evaluates polypharmacy and associated comorbidities in diabetes.10
In our study findings, (32) 40% girls and 48(60%) men made up the group. Among them, 53 (66.2%) patients were between the ages of 51 and 70, followed by 17 (21.2%) patients between the ages of 71 and 90, and 10 (12.5%) patients between the ages of 31 and 50. In a study conducted by Stuttard et al more male patients (55.6) as compared to females (44.4) suffer from DM. 11 Also, Acharya et al in their study observed that patients suffering from diabetes were 50.4% males and 49.6% females. 6 A study conducted by Upadhyay et al also showed that more no. of males 59.59% as compared to females 43.41% suffer from DM. 12 These findings were in accordance with our study in which the prevalence of diabetes among males was more as compared to females.
Diabetes is accompanied by a wide variety of comorbidities. Our current study found that 82.5% of the patients had hypertension, 58.7% had hyperlipidemia, 46.2% had cardiovascular diseases, 40% had obesity, and 30% had gastrointestinal illnesses as their primary diagnoses. In research by Stuttard et al, 30% of Type 2 DM patients at diagnosis and 60% of patients ten years later had three or more comorbidities. Traditional Type 2 DM disorders (hypertension (37%) and ischemic heart disease (10%), depression (15%), back pain (25%) and osteoarthritis (11%) were the comorbidities upon diagnosis. 11
Moreover, a review of national medical records found that hypertension, dyslipidemia, IHD, and respiratory issues are prevalent comorbidities with type 2 DM.13 Obesity (90.49%), dyslipidemia (93.43%), and hypertension (83.40%) were found to be prevalent comorbidities related to type 2 DM in research by Jelinek et al.14 Eighty-three percent of patients experienced one or more problems, including frequent renal involvement, and the majority of them had poor glycaemic control. In drug-use research conducted in Bengal, the majority of patients (74%) had coexisting diseases like hypertension (50.8% of patients), dyslipidemia (24.3% of patients), etc. Comorbidities raise the cost of treatment, the burden of the condition, and the quality of life.15 These findings confirm those of our recent study, which identified hypertension as the most common comorbid condition. In our analysis, the most frequently prescribed diabetes medications were metformin (81%), followed by glimepiride+metformin (43%), Vildagliptin (26%), Dapaglifozin (16%), Voglibose (8%), Gliclazide (6%), sitagliptin (4%), regular insulin +NPH (3.2%), and glargine (2%). According to a study done in Iraq, Biguanide (metformin) alone accounted for 22% of all anti-diabetic prescriptions. The most typical anti-diabetic medicine combination was biguanides (metformin) plus sulfonylurea, which was used in 19% of patients. In 23% of the patients, only insulin preparations were utilised, and Novomix was the most prevalent type (10%).16
Metformin was the most frequently administered oral hypoglycemic medication in research by Gour et al. in the monotherapy category, with 23.52%, followed by sulfonylureas like glimepiride, with 1.5%.17 The medication prescribed the most frequently in combination therapy was metformin + glimepiride (27.5%). In a study by Tiwari et al, patients with type 2 DM were most frequently provided oral anti-diabetic medications (72.33%). Five of these patients (3.35%) were receiving metformin alone, compared to 81 (54.36%) who were receiving a fixed-dose combination of glimepiride (SU) and metformin (MET). The aforementioned results are consistent with our study, which found that metformin and its combination with glimepiride are most frequently utilised.18 Several anti-diabetic medication therapies were given to type 2 diabetics in research by Sultana et al. Biguanides (metformin), The most frequently used medications were sulphonylureas (glimepiride), thiazolidinediones (pioglitazone), insulin, and alpha-glucosidase inhibitors (miglitol). prescribed classes of anti-diabetic medications.19 According to a study by Singla et al, sulfonylurea class of medications (66.9%) and metformin (79.6%) were the two most often prescribed medications.20 Metformin was identified by Satpathy et al. to be the most often administered medication (79.6%), followed by the sulfonylurea class of medications (66.9%) in their study.21
Vildagliptin (a DPP-4 inhibitor) and Dapaglifozin (a SGLT2 inhibitor) are other regularly utilised drugs in our study. Because there is a danger of hypoglycaemia and weight gain with sulphonylureas, novel agents with better safety profiles are required. Whereas (SGLT2) inhibitors decrease renal glucose reabsorption and promote urine glucose excretion, therapy with (DPP)-4 inhibitors reduces renal glucose reabsorption and stimulates insulin secretion in a glucose-dependent manner, improving hyperglycaemia. These medications are appealing alternatives for combination therapy with other glucose-lowering medications, such as insulin, due to their potential complementary mechanisms of action and good tolerance profiles.22
Conclusion
Hypertension, hyperlipidemia & cardiovascular conditions were the commonly associated comorbidities with type 2 DM. Metformin in 81% followed by glimepiride+ metformin 43%, Vildagliptin 26% & Dapagliflozin 16% were commonly prescribed. DPP-4 inhibitors and sodium-glucose co-transporter-2 (SGLT2) inhibitors are the potential new therapies with good safety profiles.