Introduction
It is indeed a challenging task to assess fetus during labour.1 Monitoring of fetal heart rate is the way to check fetal wellbeing in patients in labour. Fetuses who are becoming hypoxic and those who can benefit from caesarian section / instrumental vaginal birth, can be identified by montoring fetal heart beat.2 Intermittent monitoring can be done using fetal stethoscope, or by an ultrasonic Doppler device.3 The heart beat can also be checked in a continuous manner by cardiotocograph machine. This method is Electronic Fetal Monitoring. It produces a paper tracing of the fetal heart rate and labour contractions of the mother.
But still now there is a high intra and inter observer variation in assessment of fetal heart rate patterns. Fetal reactivity is a very important CTG characteristic used to diagnose fetal distress, but interpretation is still uncertain, Furthermore, there are no reliable auscultatory indicator of fetal distress other than extreme changes in fetal heart rate.4 Thus both electronic fetal monitoring and auscultation has not been proven to reduce perinatal mortality inspite of large clinical trials. There is debate about effectiveness of cardiotocograph as well as the relative merits of its routine application in low risk pregnancies verses use for high risk pregnancies.5 These two commonly used modalities for intrapartum fetal heart rate monitoring has been extensively reviewed but there is no high quality evidence that these techniques perform better than the other in low risk pregnancies.6
The possible advantages of CTG are more measurable parameters related to fetal heart rate patterns and that it gives a continuous recording of the fetal heart rate and uterine activity. This is a physical record. It is useful in clinical audits, counselling of parents when there is any adverse outcome, and also medico-legal situations. The possible disadvantages of CTG can be complexity of the fetal heart rate patterns due to which standardisation becomes difficult. It also prevents mobility and use of methods like massage, different labour positions and/or immersion in water becomes restricted which are used to improve maternal comfort, and as coping strategies during labour. It causes shift in the focus of the staff and the resources away from the mother. Some studies focussing at women’s preferences found that it was more important to get support from staff and labour companions than the monitoring type.7, 8
There are concerns about the safety and efficacy of routine use of continuous CTG in labour.9 So a reassessment of this practice is warranted as there is contradiction between the extensive use of continuous CTG and recommendations to limit its use routinely.10
Objectives
In this study, the very target was to evaluate whether continuous cardiotocography has any impact in changing the outcome of labour in comparison to intermittent auscultation. So the role of CTG monitoring in active stage of labour was reviewed. Presently cardiotocography is associated with increased false positive fetal distress rates and increased incidence of operative or instrumental delivery. Furthermore cardiotocography impairs the mobility of the mother in first stage of labour. Our study tried to find out the outcome of the labour and well being of the mother and neonate comparing both ways of fetal heart rate monitoring. The study gave emphasis on the mode of delivery comparing both ways of fetal heart sound monitoring.
The proposed hypothesis was that Intermittent auscultation is equally effective in monitoring labour in low risk pregnancies in comparison to cardiotocographic monitoring which rather has increased incidence of operative and instrumental delivery.
Materials and Methods
The study was conducted in Department of obstetrics and gynaecology of a tertiary medical college in eastern part of India. It is an observational study where 200 Pregnant mothers in active first stage of labour in their singleton term pregnancy with spontaneous onset of labour were included in the study and divided into 2 groups by simple randomization, one group being monitored by continuous cardiotocographic monitoring and the other group by intermittent auscultation. Patients having obstetric or medical complications were excluded from the study including previous caesarean section patients. The outcomes measured were mode of delivery, fetal heart rate patterns, maternal comfort level, amniotic fluid colour, cord blood pH, neonatal ICU admissions and complications.
Results
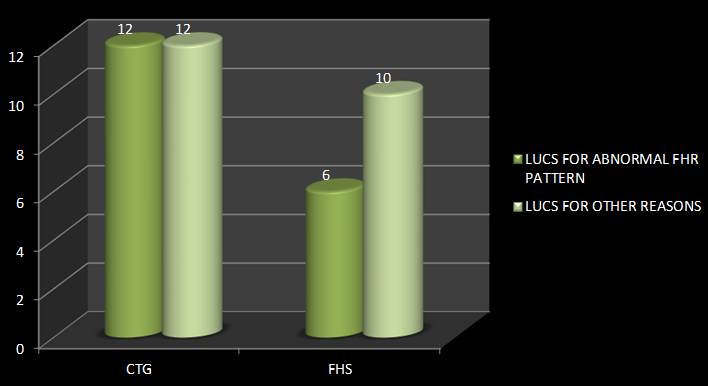
The distribution of patients according to age and parity was similar. The most important outcome that was being studied in this study was the mode of delivery. Out of 100 cases, 24 undergone caesarean section of which 12 were due to abnormal FHR pattern. Out of 100 controls, 16 patients undergone caesarean section of which 6 were due to abnormal FHR. This indicates there is 1.5 times higher C-section rate in the ctg group (r=1.5, 95% CI=0.64 to 3.51) and 1.33 times higher risk of caesarean section for abnormal fhr pattern in the ctg group(r=1.33, 95% CI=0.46 to 3.84).(Figure 1)
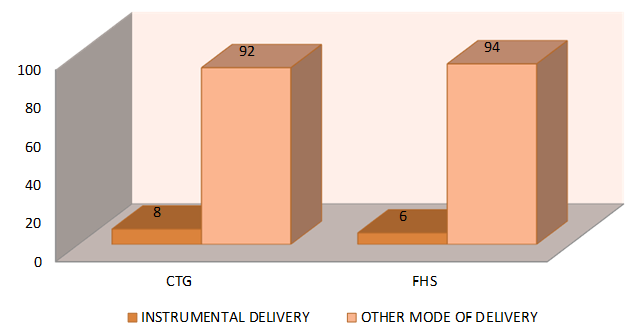
The other mode of delivery studied was incidence of instrumental delivery (forceps delivery or vacuum extraction). Out of 100 cases there was 8 instrumental deliveries of which 6 were due to abnormal fhr pattern. Out of 100 controls there were 6 instrumental births of which 4 were due to abnormal fhs. This indicates 1.33 times higher instrumental delivery in ctg group (95% CI=0.31 to 5.8) and 1.125 times higher chance of instrumental delivery due to abnormal fhr in ctg group (95% CI=0.42 to 2.99).(Figure 2)
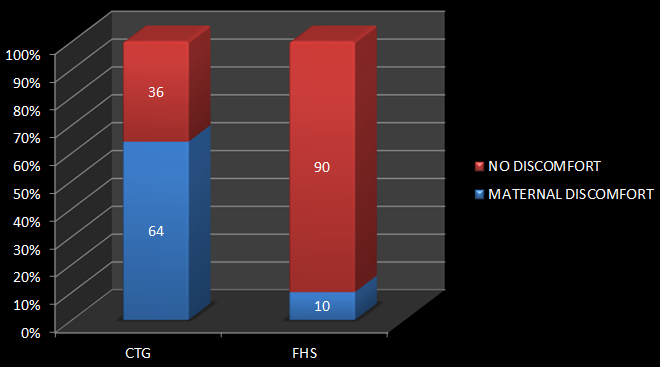
Maternal comfort level during use of either of the method for fhr detection was studied through questionnaire. Out of 100, 64 patients complained of serious discomfort during use of ctg, whereas only 10 patients monitored through fhs auscultation complained of any discomfort during fhs auscultation. This means 6.39 times more complaints of discomfort in ctg monitored cases (95% CI=3.49 to 11.73, p value <0.0001. So this association is considered to be extremely statistically significant.(Figure 3)
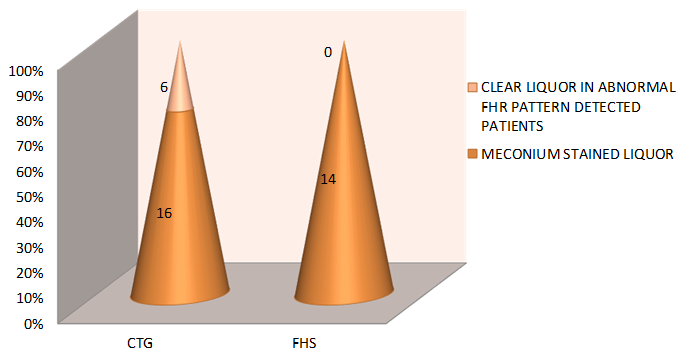
Out of 22 patients detected to have abnormal fhr pattern by ctg, 16 were found to have meconium stained liquor while all 14 out of 14 patients detected to have abnormal fhs by auscultation had meconium stained liquor. So correlation of abnormal fhr finding with meconium stained liquor is weak in case of ctg group when compared with the fhs group (r=0.72, 95% CI= 0.51 to 1.04, p=0.7325).(Figure 4)
Out of 100 ctg patients, 18 were found to have cord blood pH <7.25, whereas out of 100 fhs group 16 patients were found to have cord blood acidosis. If cord blood acidosis is taken to be a definite marker for fetal distress, then specificity of ctg (abnormal fhr pattern 22) will be 97.8%, and sensitivity almost 100%. But in case of fhs auscultation group (detection of abnormal fhs in 14), its specificity though being 100%, its sensitivity comes to 87.5%.(Table 1, Table 2 )
Table 1
Sensitivity of CTG is 100% and specificity is 97.8%
|
|
Cord blood acidosis |
||||
|
Yes |
|
No |
|
||
|
Abnormalfhr pattern in ctg |
Yes |
True positive |
18 |
False positive |
4 |
|
No |
False negative |
0 |
True negative |
78 |
|
Table 2
Sensitivity of IA group is 87.5% and specificity is 100%.
|
|
Cord blood acidosis |
||||
|
Yes |
|
No |
|
||
|
Abnormal fhr pattern in auscultation group |
Yes |
True positive |
14 |
False positive |
0 |
|
No |
False negative |
2 |
True negative |
84 |
|
The neonatal nursery admission rates are compared in both the groups and there was no difference in the nursery admission rates in both the groups. Perinatal death rate of both the groups were also same.
Discussion
In a similar study done in Melbourne in 1981 by Wood et al, 11 regarding caesarean section the relative risk was 1.95 (95% CI= 0.91 to 4.18) where n=445 and in a study in Seattle 1987, 12, 13, 14, 15, 16 the risk was 1.02(95% CI=0.57 to 1.82) in which patients were selected irrespective of obstetric risk. In another study in Dallas 17, 18 in 1986 by Leveno KJ et al, the relative risk for caesarean section for abnormal fhr pattern was 2.30 (95% CI= 1.48 to 3.58) in ctg group.
In the study done in Melbourne 11 in 1981, the relative risk for instrumental delivery in ctg group was 1.29 (95% CI=1.02 to 1.62) times higher than fhs auscultation group.
Maternal comfort level during use of either of the method for fhr detection which was studied through questionnaire, was 6.39 times more of discomfort in ctg monitored cases (p <0.0001). Thus in the ctg monitored group, many patients complained of restricted mobility and uneasiness. In a study done in UK, women’s perspective on routine continuous CTG in labour was taken and a lack of discussion about CTG’s need and appropiateness was identified. To add that, women also felt that CTG limited their movement ability and also that the machine becomes the focus of attention for the expectant mother and her partner. 19
When comparing the two groups, cord blood acidosis has been found to be 1.125 times more incident in the ctg group than the fhs group. According to the study done in Athens in 1993, the relative risk of getting cord blood acidosis was 1.58 in the ctg group (high and low risk combined) than IA group( 95% CI =0.89 to 2.81). 20, 21
There was no difference in the nursery admission rates in both the groups in this study. But in Melbourne study37 in 1981 it was 1.33 (95% CI =0.93 to 1.91) i.e it was more in ctg group. The study shows perinatal death rate of both the groups were same. According to Dallas study in 1986 it was 0.80 (95 % CI= 0.22 to 3.0). 17, 18
Continuous CTG monitoring was introduced in clinical practice with a belief that it would reduce the incidence of perinatal deaths and hypoxia related brain injury. There was no statistically significant difference in the rate of perinatal deaths between continuous CTG group and intermittent auscultation group. But to think that any type of intervention in intrapartum period in modern obstetric care will reduce perinatal deaths significantly is unrealistic. To test the hypothesis that continuous CTG will be helpful in preventing one death in one thousand births (0.1%), a large number of women close to 50,000 has to be randomised. So it will be more logical to concentrate on maternal and fetal morbidity.
Our study here showed no better outcome in patients monitored by ctg in low obstetric risk patients than intermittent auscultation. Though it detects more patients having abnormal fhr pattern, it increases the rates of caesarean or instrumental vaginal deliveries compared to intermittent auscultation. Cardiotocographic monitoring also causes maternal discomfort and is disliked by many of the patients.
Conclusion
The study done to evaluate whether there is any significant impact of continuous cardiotocography in comparison to intermittent auscultation on perinatal outcome performed in patients in active stage of labour shows that in low obstetric risk patients, there is no significant difference in most of the parameters.
Though our study showed an increased risk of caesarean sections and instrumental vaginal deliveries but that too is not in significant numbers. The debate on risk verses benefit will continue to focus on operative deliveries. So the increased risk of distress of the newborn delivered by C-section, the increased risk of injury to the bladder, further rerquirement of surgery, need for hysterectomy, development of thromboembolic disease, and other problems in future pregnancies and maternal mortality all need to be taken into consideration. Rather our study showed significant increase in maternal discomfort in cases of continuous ctg monitoring particularly in advanced stage of labour due to restricted mobility and feeling of tightness of the transducer belts. However it is undoubted that ctg has better detection ability for fetal heart rate abnormality. The sensitivity of detecting fetal heart rate abnormality is more in ctg monitored patients but the specificity is more in case of intermittent auscultation group. The neonatal outcome were not different in both the groups. So in low obstetric risk patients, perinatal morbidity or mortality does not depend on the mode of fhr monitoring.
In a country like ours or other developing countries, where resources are poor, and CTG requiring trained personnel , one to one care, CTG has not been cost effective in comparison to intermittent auscultation rather IA has sometimes outweighed CTG in terms of fetal heart rate monitoring efficiently. Women, medical practitioners as well as policy makers should consider the fact that there is no evidence that continuous CTG monitoring has any better impact on low obstetric risk patients when compared to intermittent auscultation.