Introduction
COVID-19 is the disease caused by a new coronavirus called Severe acute respiratory syndrome coronavirus 2.1 Laboratory and imaging characteristics are crucial in diagnosis and assessment of severity of COVID -19 disease. An unfavorable clinical outcome is associated with elevated CT scores, heightened D-dimer levels, and a decreased absolute lymphocyte count. 2 Leukocyte and neutrophil counts serve as indicators of COVID-19 infection, with higher counts signaling increased infection severity. Additionally, COVID-19 patients may experience coagulation abnormalities, particularly thrombotic complications. Elevated D-dimer levels and their progressive rise throughout the disease course are linked to worsening conditions. Further, coagulation irregularities such as abnormal Prothrombin Time (PT), activated Partial Thromboplastin Time, increased fibrin degradation products, and severe thrombocytopenia can lead to the life-threatening condition known as Disseminated Intravascular Coagulation (DIC). 3 The incubation period is 1-14 days Around 7 to 14 days following the onset of the initial symptoms, a cytokine storm occurs, characterized by a surge in clinical manifestations and an increase in inflammatory mediators and cytokines. 4 The high level of cytokines also indicates a poor prognosis in COVID-19. 5 Present study is aimed to analyse these parameters of patients with COVID-19 infection.
Materials and Methods
The current research was carried out in academic teaching hospital of central India over a period of 2 years. Written consent of all patients or patients relatives were taken after explaining to them the whole procedure. All RT-PCR positive Covid-19 patients above 18 years of age were included. 300 patients were divided into 2 groups A and B. Group A included patients diagnosed as RT-PCR positive Covid-19 and admitted in non-ICU ward. Group B included RT-PCR positive patients admitted in ICU
On the first day of admission and on the 4th day of hospital stay samples were collected and were analysed in our hospital’s laboratory.
We included Adult patient > 18 years old of either sex with a RT-PCR positive for Covid 19.
And excluded pregnant patients, patients with previous known coagulopathy, patients already on treatment with systemic anticoagulants or antiplatelet therapy or vitamin K antagonists,subjects with short hospital stay (Less than 4 days).
Results
Table 1
Comparison of haematological, coagulation and biochemical parameters in ward and ICU patients on day 1
Table 2
Comparison of haematological, coagulation and biochemical parameters in ward and ICU patients on day 4
Table 3
Distribution of age among the study subjects (n=300)
|
Age Range (year) |
Ward |
ICU |
|
18-40 |
40 |
36 |
|
41-55 |
65 |
69 |
|
>55 |
46 |
44 |
Table 4
Distribution of sex among study subjects (n=300)
|
Sex |
Ward |
ICU |
|
Males |
85 |
75 |
|
Females |
68 |
72 |
|
Ratio |
1.25:1 |
1.04:1 |
The predominant age group in our study was 41-55 years, encompassing 134 patients, followed by the age group above 55 years, comprising 90 patients. Our study revealed a male preponderance, with a male-to-female ratio of 1.25:1. Furthermore, a majority of the deceased patients were observed in the age group exceeding 55 years. Total 92 patients died out of 300 patients.
Most common Comorbidity in our study was hypertension followed by diabetes mellitus.
Leukocytosis (mean total leukocyte count=13500/cumm) was observed in ICU patients and the TLC count was further increased in ICU patients on day 4. No significant correlation was observed between CT score and TLC count.
Neutrophil to lymphocyte ratio (3.2) was raised in ICU patients. We also found out that NLR value increased in ICU patients on day 4 compared to day 1. We also compared the NLR between dead and alive patients and found out that in dead patients NLR was significantly increased.
Thrombocytopenia was observed in ICU patients on day 1 and the platelet count further decreased on day 4.(124500/l)
PT and Aptt were slightly increased in ICU patient. We also found out that PT value was on higher side in dead patient compared to alive patients.
D-dimer was raised in ICU patients (2325ng/ml) whereas we found an increasing trend in value of D-dimer in both ward and ICU patient on day 4 compared to day 1. Positive correlation was found between CT score and D-dimer for predicting patients severity and clinical outcome.
Fibrinogen levels were normal in ward patients whereas it were raised in ICU patients (5 6g/l).
There was mild increase in S.LDH value in ward patient on day 1 as well as day 4. In ICU patients S.LDH values were further increased on day 4 (945.5IU/l) in ICU patients compared to day 1. S.LDH values were on higher side in dead patients compared to alive patient, thus from our study S.LDH could be used as a prognostic marker for predicting the prognosis of Covid-19 patients.
CRP values showed increasing trend in both ward as well as ICU patients whereas CRP values were significantly more in dead patient compared to alive patient.
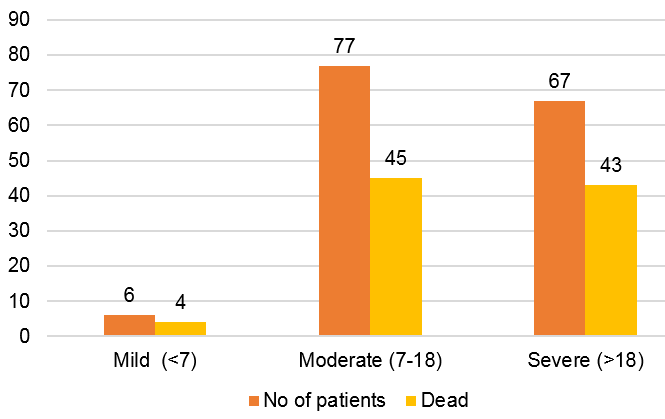
Majority of patients i.e 77 patients had CT score in the moderate range i.e CT score (7-18). 67 patients had CT score in the severe range i.e CT score (>18).
Discussion
Coronavirus disease pandemic is a rapidly involving global emergency. Emerging researches have described that Covid-19 disease is involving plethora of patient’s factors including demographic, clincal, immunologic, hematological, biochemical and radiographic findings. 6
Mean age of patients in our study was 48.5yr.
In our study Majority of patients were seen in the age group 41-55y. This was in Concordance with study conducted by M. Bairwa et.al. 7
Out of total 300 patients, 160 patients were male i.e 53.3%. Huan Han et.al 8 study included 94 patients and had 48 males i.e 51%. Thiago correa et.al 9 had total 30 patients out of which 15 were males i.e 50%
Most common co-morbidity found in patients in our study was hypertension (18%).
In the present study the mean± standard deviation of haemoglobin was 11.2 ± 2.5 g/dl whereas the study conducted by M. Bairwa et.al 7 had values of 12.4 ± 2.3 g/dl.
Leukocytosis was observed in ICU patients. Lymphopenia was observed in 13% of patients in a study conducted by Bhuiyan.M.N et.al 1
The NLR was in normal range in ward patients whereas it was raised in ICU patients. The Neutrophil-to-Lymphocyte Ratio (NLR) emerges as a valuable prognostic indicator for forecasting disease severity in individuals with Covid-19 (P value = 0.0023). Zhang et al.10 study found that an NLR of ≥ 8 is linked to heightened 28-day mortality.
Ward patients exhibited a normal platelet count, whereas ICU patients displayed thrombocytopenia. A decreased platelet count could serve as an indicator for mortality in individuals with Covid-19 (P value = 0.002). Notably, a study conducted in Wuhan revealed that thrombocytopenia upon admission in Covid-19 patients was linked to a 4.24-fold increased risk of inpatient mortality. 11
PT and Aptt was normal in ward patients whereas they were slightly increased in ICU patient. Lang wang et al 12 study concluded that 18.8% patients showed prolonged PT and the PT and APTT were significantly longer in those who died.
D-dimer was raised in ICU patients whereas we found an increasing trend in value of D-dimer in both ward and ICU patient on day 4 compared to day 1. . D-dimer was significantly raised in dead patients. (P value =0.008)Thus it could be a reliable prognostic marker for in-hospital mortality in patients of Covid-19. Mukesh et al 7 study had mean ± standard deviation of D-dimer values of 723 ± 702 ng/ml showing increasing values in COVID-19 infected patients.
S.Fibrinogen levels were raised in ICU patients. Zhenzhou Wang et al 13 study had mean ± S.D values of 4.5 ± 1.5g/l and they found out that serum ferritin and CRP related to inflammation affect fibrinogen levels, and are positively correlated with fibrinogen.
Both S.LDH and CRP values were increased in ICU patients. Elevated LDH levels appear to indicate that multiple organ failure and injury may have a more significant impact and clinical consequences in COVID-19 patients.
The correlation between elevated CRP levels and unfavorable outcomes may be attributed to the disease's severity, aligning with the 'cytokine storm' theory in COVID-19. This theory suggests that the activation of the innate immune system releases TNF-alpha, IL-6, and IL-1, contributing to the observed association. 14
67 patients had CT score in the severe range i.e CT score (>18). A CT score of ≥ 18 was associated with an increased mortality risk and was found to be predictive of death both in univariate and multivariate analysis. 15
Our study was limited by missing data because not all patients, particularly those with mild symptoms admitted in isolation wards had daily laboratory tests performed. Our data set did not include the baseline laboratory findings for ICU patients moved from other facilities. Since it was a pandemic, it was not possible to get the radiological findings of ward patients.
Conclusion
COVID-19 is a systemic infection that markedly influences both the hematopoietic system and hemostasis. Factors like leukocytosis, thrombocytopenia, increased NLR, increased D-dimer, Increased S.LDH and CRP could be used as a marker for severity and hospital based mortality in Covid-19 infected patients. Thrombocytopenia and increased D-dimer levels were associated with higher CT score.
Laboratory and imaging characteristics are crucial in diagnosis and assessment of severity of COVID -19 disease. Therefore, a meticulous assessment of baseline and evolving laboratory parameters can aid clinicians in tailoring treatment approaches, enabling timely initiation of intensive care support for patients, preventing complications such as organ failure or shock.