Introduction
ACS belongs to a group of syndromes that encompass unstable angina (UA),ST elevated and Non ST elevated myocardial infarction that suddenly obstruct the blood flow to the heart. Among adults, the estimated prevalence of coronary heart disease in urban population is 8-10%.1 ACS usually affects the geriatric population. Sudden cardiac death, Acute myocardial infarction (AMI) and UA are among the consequences of atherosclerosis that are influenced by platelets.2
As the plaque ruptures in coronary arteries, there is platelet hyperactivity with activation of platelets which increases platelet mass and volume that aid in thrombus formation. Platelet activation causes the release of prostaglandins and leukotrienes which is a potent vasoconstrictor and platelet aggregating substance amplifying acute inflammatory response.3
Larger platelets are more aggregative and adhesive than smaller platelets. Large platelets contain higher procoagulatory surface proteins such as P-selectin and glycoprotein IIIa. Activated platelets cause conformational change in glycoproteinIIb/ IIIa which has a higher affinity for fibrinogen. Fibrinogen binds to two different platelets promoting aggregation and cross linking.4 Larger platelets have higher level of metabolic and enzymatic activity than smaller ones. Thromboxane A2 is elevated in larger platelets due to increased alpha granules, thus having a high expression of adhesive glycoproteins.5
The most sensitive indicators of myocardial damage are creatine kinase, troponin T and troponin I. Levels of Troponin I and Troponin T rise at 2 to 4 hours and the peak occurs at 48 hours. After AMI, creatine kinase begins to increase in 2 to 4 hours, peaks at approximately 24 hours and returns to normal in around 72 hours.6
The current study aimed to compare platelet indices among ACS patients and healthy controls It helps to predict ACS in patients with high platelet indices. The platelet indices are inexpensive and can be calculated by blood sample using simple complete blood count analysis which can be performed at basic medical health facility like Primary Health Centre.
Materials and Methods
A case control study was performed prospectively in a tertiary care centre with 100 cases and 100 controls for six months. All patients clinically diagnosed with ACS were included in the analysis and compared with controls.
Method of collection of data: The study was conducted on 100 healthy controls and 100 cases clinically diagnosed with ACS. Demographic data was collected from patient files. Using a 5ml syringe, the patient’s blood samples were extracted from the antecubital vein and mixed right away with EDTA vacutainers. The sample was analysed using the 5-part differentiated automated haematology analyser within 2 hours of the venepuncture. A complete blood count was made such as “Total platelet count”(TPC) and platelet indices such as PCT (Plateletcrit), P-LCR (“Platelet Large Cell Ratio”), P-LCC (“Platelet Large Cell Count”), PDW (“Platelet Distribution Width”), and MPV(“Mean Platelet Volume”). The automated haematology analyzer runs on the impedance principle for platelet indices calculation. Relevant cardiac enzymes such as Troponin I and CK-MB were studied. Data was compiled in MS Excel 2021 and statistically analyzed based on frequency, percentage, mean and standard deviation in SPSS software. P value was calculated to determine the statistical significance of each platelet parameter in cases and controls. Statistically significance was considered as P <0.05. Institutional Ethical clearance is obtained.
Results
A total of 200 individuals were assessed which included 100 cases and 100 controls. The mean age of the cases in our study was 65 years. Most of the cases diagnosed as ACS belonged to the 7th decade of life (38%) followed by 6th decade (26%) of life.(Table 1)
Table 1
Age distribution of ACS patients
|
Age range of cases |
Percentage (%) |
|
21-30 |
2 |
|
31-40 |
10 |
|
41-50 |
6 |
|
51-60 |
10 |
|
61-70 |
26 |
|
71-80 |
38 |
|
81-90 |
8 |
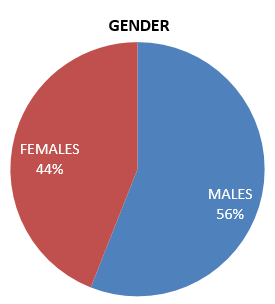
The current study showed a predominance of males in Cases of ACS which comprised 56% males and 44% females.(Figure 1)
In clinically diagnosed ACS cases, CK-MB and Troponin I Levels were done. As per our study 98% of cases showed raised CK-MB levels and 28% cases were positive of Troponin I.
The platelet indices such as TPC, PCT, PDW, MPV, P-LCC and P-LCR were assessed among patients with ACS and compared with control groups.
Table 2
Comparison of platelet indices among cases and controls
Table 3
MPV distribution in previous studies
|
Studies |
MPV in Cases (µm3) |
MPV in Controls (µm3) |
p value |
|
Jasani et al7 |
11.02 |
7.98 |
<0.05 |
|
Piplivali et al8 |
11.97 |
10.7 |
<0.05 |
|
Subrayan et al9 |
8.69 |
7.89 |
<0.001 |
|
Shilpa N et al10 |
15.54 |
14.87 |
<0.001 |
|
Present study |
9.85 |
8.54 |
<0.001 |
Table 4
PDW distribution in previous studies
|
Studies |
Mean PDW in Cases (µm3) |
Mean PDW in Controls (µm3) |
p value |
|
Piplivali et al8 |
15.23 |
13.25 |
<0.001 |
|
Subrayan et al9 |
16.70 |
11.97 |
<0.001 |
|
Shilpa N et al10 |
15.54 |
14.87 |
<0.001 |
|
Present study |
14.582 |
12.88 |
0.0001 |
The current study showed a rise in P-LCR, PDW and MPV among ACS cases than controls. P value was calculated and found to be statistically significant that is <0.05.However low TPC and low PCT were encountered in cases with respect to controls. P-LCR is the ratio of P-LCC to platelet count. P-LCC among cases and controls was not statistically significant as the p value was 0.48 in the current study.(Table 2)
Discussion
ACS is one of the main causes of mortality. Patients most commonly experience crushing chest pain associated with nausea and sweating.11 Cardiac changes in ECG take time to appear, hence ECG may not be helpful during the initial hours. Specific cardiac biomarkers like CK-MB, troponin I and myoglobin help diagnose ACS early during the initial hours with reasonable accuracy. These tests are costly and not routinely available. Hence platelet indices such as TPC, MPV, PDW, P-LCR and PCT can be easily obtained in complete blood examination using an automated analyser.12 These platelet indices can be of importance in predicting ACS patients.
Vascular occlusion is caused mainly by platelet aggregation thus, analysing parameters related to platelet is important for preventing new episodes of cardiovascular attacks.5 Platelets are heterogeneous in terms of size, density and activity.13 Platelet size and function correlate as giant platelets are formed from activated megakaryocytes in the bone marrow which seem more reactive than normal platelets. Large platelets are more active than small platelets as they contain more secretary granules and mitochondria. 3
Satpathy et al showed 87.4% males and 12.6% females concordant with the current study.13 The first index is the TPC. Larger platelets have a lower absolute count so as to maintain the total effectiveness of platelet mass. 4 The present study shows reduced mean TPC in cases with a p value of 0.01 compared to controls. The survey done by Ridwan et al and Gargi et al also presented a similar reduction in the TPC of AMI and UA patients. 14, 15
MPV of ACS cases and controls in our study were statistically significant and correlated with studies done by Jasani et al, Piplivali et al, Subrayan et al and Shilpi et al illustrated in Table 3. Increased MPV has been related to cerebrovascular illness, hypertension with evidence of target organ damage, coronary artery disease and AMI. 2
We found statistically significant PDW in patients of ACS which were also seen in studies performed by Piplivali et al, Subrayan et al and Shilpa et al.(Table 4)
Pervin S et al, Nandwani S et al and Khandekar MM et also expressed in their studies that platelet indices including MPV, PDW and PLCR were notably greater in patients with ACS as compared to controls similar to this study. 16, 17, 18 As per the study done by Biradar et al platelet volume indices PDW, MPV and PLCR were raised in patients with AMI and UA compared to control group. 19 In present analysis PLCR was increased in ACS patients. This is similar to the study done by Pipliwal et al, Dehghani et al and Abuzar et al 8, 20, 21
The current study showed a decrease in PCT in ACS patients which correlated with study done by Pipliwal et al and Assiri et al. 8, 22 However a study done by Siva Prasad Akula et al showed increased PCT in ACS patients. 23 In the study by Satpathy et al platelet parameters like PCT and P-LCR were significantly greater in ST elevated myocardial infarction (STEMI) group than in UA group. P-LCR and PCT increase are considered to be risk factors for development of ST elevated myocardial infarcts than UA. Therefore, when compared to UA in ACS patients, they may act as straightforward yet crucial early indicators for predicting the development of STEMI. 13
A study by Gururajprasad et al presented a significant increase in platelet indices like P-LCR, PDW and MPV in MI patients as compared to stable patients or controls. 24 Huang et al reported that MPV was elevated in ACS cases than in non ACS cases and documented MPV as an independent predictor of ACS.25 Abdullah et al observed a notable correlation of ACS with MPV and PDW. 26
Conclusion
Irrespective of the spectrum of ACS platelet indices are strongly related with each other in a positive way. Platelet indices are easy to perform, reliable, simple, non-invasive and economical. As per the present study increase in PDW, MPV as well as P-LCR were detected among ACS patients. Thus these platelet indices may play a significant role in predicting the risk of ACS.