Introduction
Acute appendicitis is commonly considered as a disease of the young, but has bimodal presentation. Life time risk for appendicitis ranges from 8.6 to 11 cases per 10,000 person years with slight male predilection. Though it remains most common surgically correctable cause of abdominal pain, its clinical diagnosis remains challenging. There lies a long list of differential diagnosis including both abdominal as well as extra abdominal causes because many of its signs and symptoms are non-specific. A delay in diagnosis and surgery in cases of acute appendicitis may lead to increasing rate of complications (appendicular abscess and perforation) where as an incorrect diagnosis subjects patients to an unnecessary surgical procedure. Despite of advances in imaging modalities, the diagnosis of acute appendicitis still can’t be made with certainty and histopathology examination remains the gold standard for confirming the diagnosis. There also have been evidence that grossly normal appendices may also have abnormal incidental findings on biopsy affecting patient management, which further highlights the importance of routine histopathological examination of all appendicectomy specimen.1, 2, 3, 4
Aims and Objectives
This study was aimed at analyzing the histopathological findings of post appendicectomy specimens in patients with presumptive clinical diagnosis of acute appendicitis so as to confirm clinical diagnosis, find complication rate, negative appendicectomy rate as well as incidences of pathological findings other than inflammation (carcinoid, tuberculosis, neuroma, malignancy, endometriosis etc.). This study also provides an insight on demographic data of appendicitis in the southern part of Odisha as well as incidence of various complications and associated pathology.
Materials and Methods
This prospective clinico-pathological study was done in (Department of pathology, MKCG MCH) in 541 routine cases with clinical diagnosis of Acute appendicitis, admitted to department of General surgery, MKCG MCH, Berhampur between 2020 to 2022. All appendicectomies were done by open technique under spinal anaesthesia.The duely labelled formalin fixed specimen was sent to pathology department along with histopathology request forms and relevant clinical data and intra-operative note. Specimen received in histo-pathology section of department of pathology, MKCG MCH. After thorough gross examination, three sections given from tip, body and base from each specimen and routine H&E stained specimens were examined. Incidental abnormal findings were reviewed. Study was focused on confirming clinical diagnosis i.e., acute appendicitis and complication rate, negative appendicectomy rate, abnormal incidental findings whether these abnormalities were suspected on gross examination during surgery and its effect on prognosis and management of patient. The study was also used to find out incidence in males and females across different age groups and variation in incidence of complications with gender. Relevant clinical data like patients age, sex. Pre-operative clinical presentation and operative findings were noted.
Inclusion criteria
All patients admitted to department of general surgery, MKCG MCH with clinical diagnosis5 of acute appendicitis. (2020-22). All emergency as well as interval appendicectomies done in cases with clinical suspicion of acute appendicitis were included.
Exclusion criteria
Patient who underwent incidental appendicectomy during other surgeries like hemicolectomy.
Case definition
In histopathology examination in cases of acute appendicitis, neutrophils were observed in mucosa and muscularis propria of appendix. Congested blood vessels with fibrinous exudates in serosa were present. 6, 7 in suppurative appendicitis associated obstruction, abscess formation within wall and evidence of necrosis in the mucosa were present. The ones with normal histological findings of specimen were noted as Negative appendicectomy.
Results
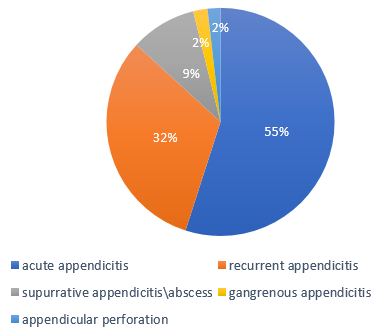
Out of 541 specimens that were examined, 499 (92.57%) histopathology findings were consistent with acute inflammation (acute appendicitis (50.3%), recurrent appendicitis (29%), abscess (8.5%) perforation (1.7%) and Gangrenous appendicitis (1.8%). The distribution of acute appendicitis is as in the Table 2. Out of the specimen with features of inflammation, 12 had intraluminal parasite, E. vermicularis and 78 had fecolith and 14 were fibrosed. The distribution of various histopathology findings of acute appendicitis with gender and age group is shown in Table 2. Rate of complication was 12.2%, (Figure 1) and more common in males. (Table 2). Findings in thirteen appendicectomy specimens were normal (2.4%) and twenty specimens (3.4%) showed abnormal incidental findings. There were 311 males and 188 females and male: female ratio was found to be 1.6:1. The mean age for male was 26 years with a range of 10-70 years and mean age in female was 21 years with a range of 3months to 60 years.
Table 1
Histopathology findings.
Evaluation of specimen with unusual histopathology findings
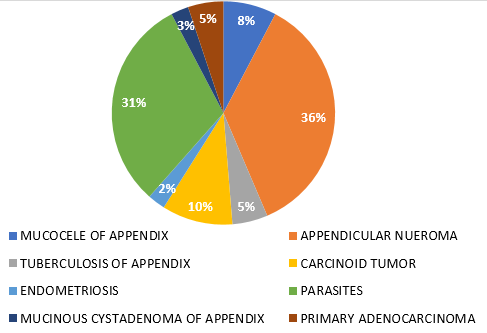
Twenty specimens were detected with unusual histopathological findings including fourteen appendicular neuroma, two Tuberculosis of appendix, one endometriosis, four carcinoid tumour, four LAMN, two adenocarcinoma. Fifteen of these were females and five males. The patient with appendiceal endometriosis was female, married and blessed with 2 children and was not previously diagnosed with endometriosis prior to appendicectomy. Two patients with granulomatous inflammation were not a known case of tuberculosis/ Crohn’s disease. Moreover, clinical as well as abdominal ultrasonography of these patients were suggestive of acute appendicitis. None of the four patients with histological diagnosis of carcinoid tumour were diagnosed with the same. 2 of the carcinoid cases were subcentiemtric and had yellowish small lesion at the tip on appendix gross examination. Other 2 carcinoid cases, tumor was more than 2cm in size and invaded serosa on histopathology, patients underwent right hemicolectomy post histopathological diagnosis. Hemicolectomy specimen sent for histopathology showed no evidence of residual disease. 4 LAMN cases underwent colonoscopy post histological diagnosis. There was no colonic epithelial lesion noted, and patients were followed up. The two cases of adenocarcinoma were primary tumours, had enlarged and thickened appendix in gross specimen, had node negative disses and the patient underwent right hemicolectomy post histopathological diagnosis.
Table 2
Incidences of acute appendicitis and complications in various age groups and sex predilection.
Discussion
Acute appendicitis is considered one of most common acute surgical conditions and several studies have reported abnormal histopathological findings in appendectomy specimens; however, sending all appendicectomy specimen to histopathology is not yet routinely done in resource limited setups. The primary pathology in a case of acute appendicitis is luminal obstruction which increases the intra-luminal pressure within the appendix, and leads to ischemia. Bacteria translocate causing inflammation, Infarction and perforation can happen leading to complications. Early diagnosis and surgical intervention may aid in decreasing such complications. In this study the rate of complication was found to be 12%. Thus this study supports appendicectomy in cases with clinical and imaging suspicion of acute appendicitis. Study also reveals Enterobius infection is often associated with acute appendicitis by causing intraluminal obstruction, and may be effectively eradicated by anti-helminthic treatment.
Maximum number of patients who underwent appendectomy were in the age group of 21-30 years which was in line with findings of Marudanayagam et al. 8. i.e most of the appendicectomies (64.58%) were performed in the second decade of life. In this study greater percentage of appendicectomies (57.5%) were performed in males as compared to females (41.5%) and the results are comparable with those of Nabipour 9 and Makaju et al. 10
Out of all the specimen examined acute appendicitis was confirmed in 50.3% specimen and 92.6% had findings suggestive of inflammation. In this study of 541 appendicectomy specimens, 532 (98.3%) were found to be involved by non-neoplastic conditions and only 9 (1.6%) cases were involved by neoplastic lesions which was in line with findings of Blair et al. 1 who reported in their retrospective study that 80% of appendectomy cases were found to be involved by non-neoplastic inflammation. Chronic fibrosing appendicitis (Appendicular neuroma) was seen in 2.6% of cases in this study, in contrast to findings by Edino et al.2 i.e. 17% cases of chronic fibrosing appendicitis. Diagnosis of endometriosis was made in just 1 (0.18%) case in the present study in contrast to Gustofson et al. 3 who studied 133 female patients and found endometriosis to be present in 4 (3%) cases. In the present study, diagnosis of LAMN was made in 4 (0.75%) of cases which was in line with findings of Marudanayagam et al. 8 (0.6%). In the present study carcinoid tumour was in 4 (0.7%) cases which was in contrast to findings of Jones and Paterson (0.1%). Polat et al 11 report an intra-operative detection rate of less than 50% for all types of appendiceal tumour. Deans et al, 12 suggested that surgeons missed abnormal pathological findings in 10 out of 13 patients, the majority of which required further investigation or treatment but in the present study only 20 cases (3.4%) had abnormal findings requiring specific management. Connor et al. 13 in their retrospective study of 7970 cases showed a discrepancy between the surgeon’s opinion of the macroscopic appearance of the appendix and the pathologist’s opinion in 14.5% of their cases and most of these were neoplastic conditions but in the present study malignancy was reported in only 1.7% cases.5
In this study, histopathological diagnosis of acute appendicitis was made in 51% of clinically diagnosed acute appendicitis cases. In 13 cases, no significant abnormality was seen histopathologically and these were labelled as normal appendices, thus accounting for negative appendicectomy rate of 2.7% as compared to study by Joshi et al14 who reported it to be as high as 14%. Negative appendicectomy rate was higher in females, especially of reproductive age group (4.5%) as compared to males. Such difference may be attributed to conditions like ovarian and tubal pathologies mimicking features of acute appendicitis clinically.
The routine histopathological examination of the appendicectomy specimen allows the diagnosis of acute appendicitis to be confirmed, especially where this is not evident intra-operatively as well as it may disclose additional pathologies that may not be evident on gross examination intra-operatively and may affect subsequent clinical management of the patient.15 Specimens reported as negative for acute appendicitis can aid in eliminating acute appendicitis as a cause of symptoms and hence allowing further investigations to be done for persisting symptoms. Even in these cases of negative appendicectomy, symptoms usually disappear in post-operative period. It has been suggested that in these cases there may be evidence of an early sub-clinical appendicitis. 6, 7, 16
This study highlights that the unusual incidental findings played a role not only in confirming acute appendicitis as a cause of the presentation in some cases but also discovering etiologies that mimic it with great impact on patient management.
Conclusion
The findings in this study suggest that the clinical as well as intra-operative diagnosis of acute appendicitis is not always reliable and various other significant histopathology diagnosis were noted after examining the routine appendicectomy specimen, thus highlighting the need and relevance of routine histopathology examination of all appendicectomy specimen. This study also suggests that the incidence of complications is more in males in age group of 20-45 and thus supports the appendicectomy in cases with clinical suspicion of acute appendicitis so as to avoid complications (perforation, abscess etc). The rate of negative appendicectomy is more in cases of females of reproductive age group, hence warrants more vigilant clinical examination and imaging studies to rule out other potential causes (ovarian cyst, endometriosis, diverticulitis, malignancy etc) mimicking acute appendicitis. Abodminal CECT though investigation of choice ,is not accessible to all health care facilities, hence post op routine histopathological evaluation,which is the gold standard, should be performed to confirm the clinical diagnosis and to rule out other pathology.
Author Contribution
Dr. B Rautaray collected, complied and analysed the data (patient information, clinical correlation and follow up) and Dr. S Tripathy was among the senior pathologists who examined the routine appendicectomy specimen, gave diagnosis and drafted the article Dr. I Gopal reviewed the draft and suggested necessary corrections for improvement.