Introduction
Critical care or intensive care is an important part of obstetric practice. We don’t have any consistent definition of Maternal critical illness. A critically ill obstetric patient is a women who develops complications because of normal or abnormal pregnancy, delivery, puerperium and abortion, or as a result of the effects of systemic disease, which puts her existence in danger. Such a patient needs thorough observation and proper treatment. Early identification and prompt treatment of critical illness is necessary for a favourable fetomaternal outcome. Maternal sepsis is the main cause of avoidable maternal critical illness in India, and thus it adds up to a significant proportion of maternal deaths and admissions to the intensive care unit (ICU).1 The economic burden, mortality, and morbidity are remarkable. 2 During pregnancy, women have various physiological and anatomical changes. Moreover, pregnancy causes complicated immune responses, which causes an increase in infection.3 Sepsis causes an unchecked host response to the infections resulting in organ damage, and the most vital organs can be affected. The source of infection in puerperal sepsis can be either pelvic or nonpelvic. Most commonly the origin of antepartum cases of sepsis are nonpelvic. The intrapartum and postpartum cases of sepsis usually have a pelvic origin. 4, 5
The maximum number of cases of sepsis usually present within 24-48 hours of delivery, abortion, or rupture of membranes.6 We don’t have much knowledge about the epidemiology, causes, incidences of maternal morbidity caused as a result of sepsis. Moreover, the outcome of maternal sepsis is unknown in developing countries like India.
We, therefore require a unanimous definition of severe infection in the clinical diagnosis for uniformity all over the world. This will allow proper management and facilitate accurate incidence reporting, which will influence health strategy and research, and prevent heterogeneity in these areas. The Confidential Enquiry into Maternal and Child Health in the United Kingdom pointed the significance of early identification and treatment of severely ill pregnant women and routine use of modified early obstetric warning scores (MEOWS) to be used for obstetric patients. 7
WHO developed an obstetric specific consensus definition in 2017, stating that: “Maternal sepsis is a life-threatening condition defined as organ dysfunction resulting from infection during pregnancy, childbirth, post-abortion, or postpartum period.”8 Sepsis-3 defined septic shock as sepsis associated with vasopressor requirements to maintain a mean arterial pressure (MAP) ≥65 mmHg in the absence of hypovolaemia and a serum lactate >2 mmol/l. 9 A large number of maternal deaths are related with risk factors like lack of care, delivery in absence of a trained birth assistant, inaccessibility to healthcare facilities etc. 10, 11
We can reduce the risk of maternal mortality and morbidity from sepsis by improving the healthcare facilities. Since the rates of sepsis are increasing worldwide and there is less data from developing countries like India, we did this study to analyze the clinical profile, fetomaternal outcome of maternal sepsis and percentage of sepsis in critically ill pregnant, postpartum and postabortal women.
Material and Methods
This study was done from 1stJanuary 2020 to 31st December 2020 in the department of Obstetrics and Gynaecology, Dr. Ram Manohar Lohia Institute of Medical Sciences, Lucknow. It included all critically ill pregnant women irrespective of the period of gestation and women within 42 days of delivery or abortion(excluding accidental or incidental causes). The selection criteria for the study were as follows -
Inclusion criteria
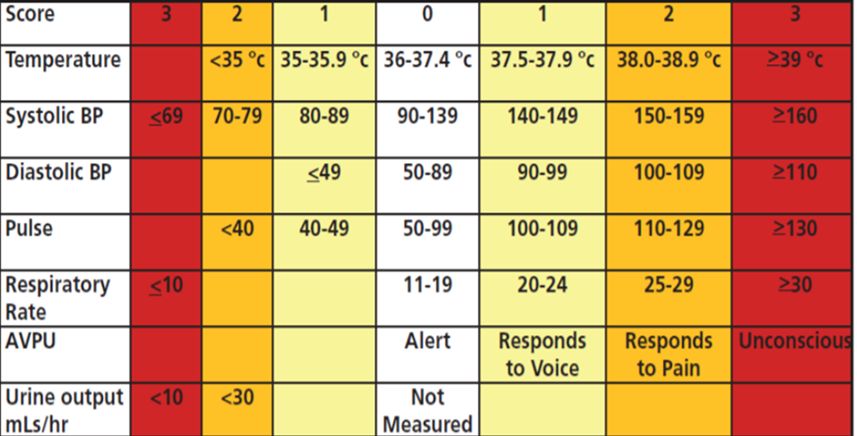
All pregnant women, irrespective of the period of gestation and all women within 42 days of delivery or abortion who had a score ≥2 in the MEOWS (Figure 1).
Exclusion criteria
Patients who refused to give consent.
Patients presenting with sepsis after 42 days of delivery or abortion.
Patients with sterile culture.
Covid positive patients.
All women who fulfilled the inclusion criteria were enrolled in the study and two groups were defined out of the cases selected. The groups were-
Group S – Patients who fulfilled the criteria of sepsis/septic shock.
Group O – Patients who had critical illnesses excluding sepsis.
Criteria of sepsis
Two of the following on atleast 2 occasions, at an interval of 4 hours:
Temperature >38°C or <36°C
Heart rate ≥100 beats/min
Respiratory rate ≥20/min
WBC =>17x109/l or =<4x109/l.
PaCO2 <32 mmHg
Or
Criteria for septic shock
Persistent hypotension requiring vasopressors to maintain mean arterial pressure (MAP) ≥65 mm Hg.
A serum lactate level >2 mmol/L despite adequate volume resuscitation.
The cases were selected prospectively after recording their findings in MEOWS chart. The investigations done were complete blood counts, renal function tests, liver function test, serum electrolytes, blood sugar and coagulation parameters. Bacterial agents were identified by cultures of clinically indicated sites, including urine culture, vaginal swabs, episiotomy wound swabs, and caesarean wound swab. Chest Xray, ECG, MRI Brain, Oxygen saturation, CRP, serum lactate, serum pro-calcitonin, arterial blood gas analysis was done for all indicated cases. Patient’s age, booking status, parity, gestational age, post-abortal or postpartum status, medical comorbidities, obstetric risk factors, organisms and their sources of infection was noted. The treatment strategy was individualized for each patient and was according to the protocols of our Institute. Maternal outcome were assessed in terms of admission to HDU/Intensive care unit, timing and mode of delivery and maternal death. Foetal outcomes were studied in the form of abortion, preterm birth, term birth, NICU admission, perinatal death. Ethical approval was taken from the Institutional Ethics Committee. The findings were recorded in a predesigned proforma.
Statistical Analysis was done using the Chi-Square test. Statistical analyses were performed with SPSS version 21.0 for windows.
Results
During the study period, 6571 deliveries occurred in our hospital. 181 patients were clinically diagnosed as critically ill as per our inclusion criteria. Out of 181 patients, 55 patients fulfilled the criteria of sepsis and 126 patients had critical illnesses excluding sepsis. The prevalence of sepsis and other critical illnesses was 8.3 per 1000 deliveries (55/6571) and 19.2 per 1000 deliveries (126/6571) respectively.
Demographic characteristics of patients of our study are given in Table 1. The mean maternal age was 30.0 years in Group S and 32.0 years in Group O. Majority of the patients were multipara in both the groups, 58.2% (32/55) in Group S and 67.4% (85/126) in Group O. 69.1% cases were unbooked in Group S, and 77.7% cases were unbooked in Group O. Both the groups had majority of patients from rural background, 70.9% (39/55) in Group S and 68.3% (86/126) in Group O. Most of the patients in both the groups had home delivery (67.3% in Group S and 53.17% in Group 0).The duration of hospital stay was similar in both the groups. None of the demographic parameters had significant variation in between the two groups. This means that Group S and Group O had almost similar demographic profile.
Table 1
Characteristics of cases
Sepsis was the most common cause which had 55 out of 181 cases (30.4%). Other causes were severe preeclampsia (21.5%), eclampsia (12.2%), postpartum haemorrhage (9.4%), ruptured ctopic (8.3%) and antepartum haemorrhage (7.2%) followed by haematological disorders (2.2%), renal disease (1.7%), dengue (1.7%), DVT (1.7%), cardiovascular diseases (1.7%).(Table 2)
Table 2
Causes of critical illness
In this study, sepsis was most common in the postpartum period (52.6%) while other critical illnesses were more commonly seen in antepartum period (86.8%). This result was highly significant.
Preterm deliveries were less common in Group S (38.2%) as compared to Group O (52.4%). Group S had 22(41.8%) admissions to ICU and 11(36.4%) admissions to HDU. While in Group O there were 34(9.5%) and 114(28.6%) admissions to ICU and HDU respectively. The incidence of HDU admissions was substantially higher in Group O as compared to Group S(p value<0.05). The mortality from sepsis was significantly higher (p value<0.05) in Group S (62%, 16/26) as compared to Group O (8%, 10/26).
Among the 55 women in Group S, there were 22 preterm births (40%), 19(34.5%) term births, 7(12.7%) perinatal deaths and 18(32.7%) NICU admissions. In Group O, there was a higher tendency of preterm births (44.4%), 35(27.8%) term births, 19(15.1%)perinatal deaths and 50 (40%) NICU admissions.(Table 3)
Table 3
Maternal and neonatal outcome
Genital tract infection was present in 47.2% of the women with sepsis. This was followed by wound infection (23.6%), urinary tract infection (18.2%) while in 11% of the patients, the site of infection remained undiagnosed (Table 4).
Discussion
After one year of this study, we came to the following conclusion that maternal age group between 21 to 35 years of age was most commonly associated with critical illnesses in obstetric population. The mortality rate were significantly higher in unbooked women than in booked women. This was similar to that found in the study by Shivananda et al12 where maximum number of patients were also in the same age group. Majority of the female who had critical illnesses were multipara. Similar results were seen in the study done by Kumari et al13 where 51% were multipara. Sepsis alone was responsible for 30.4% of maternal critical illnesses. The most common source of infection was genital tract infection (26/55, 47.2%) which was similar to the study done by Acosta et al.14 Majority of the females had sepsis in the postpartum period(29/55, 52.7%), while other critical illnesses were more common in the antenatal period(104/126, 82.5%). In the study done by Knowles et al, 15 Percentage of sepsis was 17%, 36% and 47% in the antenatal, intrapartum and the postpartum period respectively. In the study done by Timezguid et al16 perinatal complications were more in maternal sepsis, this was different in our study. Our study showed more perinatal deaths in Group O.
The mortality from sepsis was significantly higher (p value <0.05) in Group S (62%, 16/26) as compared to Group O (8%, 10/26). This is considerably greater than the data mentioned in other studies from India. Since our hospital is a tertiary care institute, patients from all cities around Lucknow are referred to our institute. 75% of the patients in our study were unbooked and were referred from peripheral health centres, who are usually not having availability of blood components, HDU and ICU facilities. This also has huge impact on the condition of the patient on arrival to our hospital as usually there is delay to seek adequate treatment and the golden time period of management is lost. This study has a limitation that the data that has been collected is small to conclude and apply these results for a bigger population.
Conclusion
Critical illnesses have a very high fatality rate in obstetric patients. Currently, lack of data on the incidence, etiology, epidemiology, and outcomes in the pregnant population, especially in the developing countries, makes comparison and estimation of the burden difficult. Moreover, this lack of data makes it essential to research this subject to build a foundation for further studies and to decrease maternal and neonatal mortality and morbidity. So, we collected this one-year data on maternal critical illness with special reference to sepsis was and through this we came to the conclusion that lack of antenatal care and delay in referral to tertiary care centre negatively affects the results in critically ill pregnant, postpartum and postabortal females. Sepsis is alone responsible for significant proportion of maternal critical illnesses, thus increasing maternal morbidity and mortality. Critical illnesses other than sepsis have an increased risk for preterm delivery, NICU admissions and perinatal deaths. Hence, to improve maternal critical care, the goal must be early recognition of the warning signs and timely intervention. Pregnancy is a physiological condition, and both maternal and foetal prognosis remains good if she receives timely intervention and management by a multidisciplinary teamin case of a critical illness.