Background
Mentoring is a reciprocal and collaborative relationship by which student is mentored by experienced person to develop professional, academic and other relevant skills. 1 An effective mentorship association helps mentee through multiple crucial outcomes such as personality and professional identity development, achievement of career goals, bridging of gaps in generic skills and knowledge etc. 2
Due to substantial curriculum workload and competitive educational environment, medical students often face several challenges. One of the major problems perceived by medical students, particularly during early phase of training, are emotional and psychological related issues like poor self-confidence, fear of failure, anxiety about future, homesickness, difficulty in adjusting to the surroundings etc.3, 4 One study reported that around 60% of students had problems with their mental health.4 Interventions like ‘mentoring programmes’ are helpful to mitigate such negative influences on students’ formation. The need for well-designed and structured mentoring programmes in initial stage of medical course to address these issues is warranted.
Even though, several authors reported that mentoring is a key strategy for successful and satisfying career in medicine; the scientific data on the role of structured mentorship programmes in addressing mental health of novice medical students is sparse. 5, 6 The present study was intended to evaluate the effects of ‘Structured Mentorship Programme’ on psychological adjustment of first year MBBS students. An attempt was also made to assess the effectiveness of an intervention through feedback from students and mentors.
Materials and Methods
Study design and sampling methods
An interventional study was implemented between year 2015 to 2017 at one of the public tertiary health care teaching institutes in Mumbai City of Maharashtra, India. An Institutional Ethics Committee approval was obtained from the respective institution. After taking an informed consent, all 150 first year undergraduate MBBS students were enrolled as study subjects. Fifteen Preclinical faculty members of same institute who volunteered to be a part of mentorship programme were included as ‘Mentors’. These 150 subjects were divided into 15 small groups according to their roll numbers and each group was assigned to one mentor.
Procedures
Questionnaires
Three prevalidated, pilot tested, standardized questionnaires were used to assess psychological adjustment of study subjects. DASS (Depression, Anxiety, Stress Scale)7 measured the negative emotional states of depression, anxiety and stress. The scale of Psychological Wellbeing (SPW)8 was 18 items questionnaire consisting of a series of statements reflecting 6 core areas of psychological well being namely autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance. The responses were recorded on a ‘Likert Scale’ of 1 to 6 with 1 indicating strong disagreement and 6 showed strong agreement. Ten items version of General Self Efficacy Scale (GSES)9 was utilized to evaluate subjects’ ability to respond to novel or difficult situations and to deal with any associated obstacles and setbacks.
Sensitization programme and planning
Initial orientation was given to subjects and mentors separately regarding the study including, the need of mentorship programme, various interactive activities between mentors and subjects, conduction of workshops and assessment methods. Mentors were provided handouts, e- books and online learning modules to ensure their in-depth understanding of mentoring process. All three questionnaires were administered to subjects and their responses were recorded as pre intervention scores.
Interactive sessions
One-on-one mentoring sessions were held through face to face meetings between study subjects and mentors. Each subject spent one hour per fortnight with the assigned mentor. Mentoring sessions incorporated individualized activities like academic counselling, personality development, stress management, communication skills etc. The subjects were encouraged to meet mentors frequently as per their felt needs. A Logbook was used to document topics or issues discussed during meetings.
Assessment and statistical analysis
At the end of the study, the subjects completed all three similar questionnaires and their responses were recorded as post intervention scores. Subjects’ and mentors’ perceptions about mentoring programme were evaluated by ‘free response’ type of feedback. The data analysis was performed using SPSS (Statistical Package for Social Sciences) 20.0 (SPSS, Inc., Chicago, IL, USA). Descriptive statistics were calculated in terms of mean, standard deviation (SD) and percentiles. Pre and post intervention comparisons were computed by ‘Wilcoxon Signed Ranks Test’ and ‘Spearman's Rank Correlation Coefficient Test’. P value of <0.05 was considered as statistically significant.
Results
In the current study, out of 150, only 87 (58%) subjects [ 42 (48.27%) males and 45(51.72%) females] attempted pre and post test questionnaires. Of which, statistical analysis was done only for 62 (41.33%) subjects as the incomplete questionnaires of remaining 25 subjects were not considered and excluded. The percentage of subjects with unanswered questionnaires was 58%. All study subjects were 19-22 years of age.
The post intervention mean score (31.40) of subjects was higher than pre intervention score (29.77) and the difference was statistically significant (p<0.001) (Table 1). It indicates that overall mentoring process improved psychological problems of subjects on DASS scale. However, there was no statistically significant association (p>0.05) between individual components (stress, anxiety and depression) of subjects and mentoring programme (Table 2).
Table 1
Impact of mentoring on psychological components of subjects (n=62)
|
DASS Scale |
Mean value |
S.D. |
p-value* |
|
Pre intervention |
29.77 |
2.784 |
< 0.001 |
|
Post intervention |
31.40 |
3.159 |
|
Table 2
Impact of mentoring on stress, anxiety anddepression (n=62)
Correlation analysis did not report any significant correlation between pre and post intervention scores with ‘anxiety’ and ‘stress’. However, ‘depression’ showed moderate positive correlation with ‘anxiety’ (r =0.463) and ‘stress’ (r=0.621) and ‘anxiety’ had moderate positive correlation with ‘stress’ (0.714).
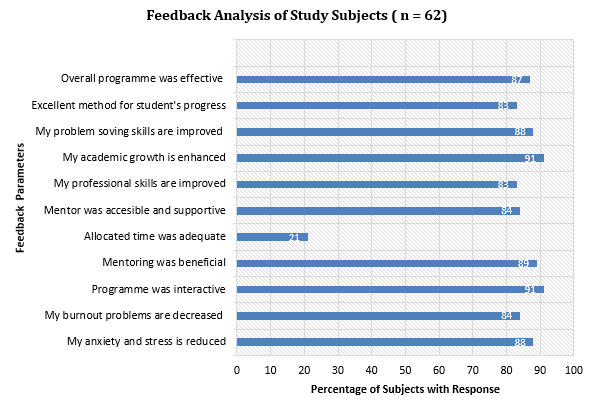
The study also revealed that ‘general self-efficacy’ of subjects was enhanced due to mentoring sessions. In present study, the majority (87%) of subjects appreciated mentoring programme as an effective method to improve psychological health (Figure 1). Around 89% of subjects found this methodology beneficial (Figure 1).
Almost more than two third of subjects stated that less time was allocated for mentoring meetings (Figure 1). Ten (16.12%) subjects felt that mentees should have flexibility in choosing their own mentors. Around 45% of subjects expressed the need of more mentoring sessions. One (1.61%) subject was in favor of availing financial support during mentoring programmes. All (15) mentors mentioned that mentoring assisted subjects to develop their personal and professional skills. Nine (60%) mentors opined that their subjects showed good academic improvement due to the intervention while 41% said that they were satisfied with the academic results of their subjects. All mentors believed that ‘student – teacher’ relationship was strengthened as a result of this methodology.
Analysis of subjects on SPW Scale also revealed significantly (p<0.05) higher scores after an implementation of mentoring sessions. These scores indicated a sense of greater wellbeing among subjects. However, the pre-intervention scores were found to be less among subjects before the commencement of mentoring programme.
Discussion
In our institution, formal mentorship programme existed since long time. This programme was restricted only to allotment of students and assigned mentors, at the entry of fresh undergraduate students. There was no induction training of mentors/ faculty and sensitization of students regarding the implementation of mentoring programme. Even, the lack of ‘blue print’ would not accomplish the predetermined goals of existing mentorship programme. Such programme was found to be ineffective to foster various skills of students. Considering the gaps into current programme, it was revised, structured and re-introduced with specific objectives, scheduling of mentoring meetings, capacity building of mentors and effective assessment methodologies.
After inculcation of modified mentorship programme, this study observed significant trend towards reduced psychological problems among subjects. This finding was consistent with previous limited literature. 10, 11, 12 Furthermore, the maximum subjects in this study thought that, their mentors embodied the features of ideal mentors, including accessible, conversant, intellectual and supportive. Such reflective feeling of subjects emphasizes on providing freedom for the selection of own mentors by mentees. This should be considered for an effective mentoring process.
In this study, mentors also perceived an array of multiple advantages like personal and professional development, knowledge sharing, achieving wider perspectives on career rejuvenation, rapport building etc. Positive self-reflection of mentors about entire mentoring process can augment their ability to learn new knowledge and skills and promote professional advancement which is one of the fundamental elements of medical education. 13
‘Mentors of same gender’ and ‘time constraints’ were noted to be the most identified challenges by subjects in the present study. Limited time and restricted number of sessions were also perceived as an obstacle to effective mentoring by Jaime Jordan et al. 10 In this study, mentor gender preferences were observed. Around 12% of subjects stated that mentor with similar sex should no be involved in mentoring process. This should be considered for further qualitative research to explore the reasons for the same. The published data suggests that mentor gender may influence the mentoring relationship even in a virtual environment. 14 Mentoring process cannot be successfully accomplished with gender differences and hence needs to be eliminated. The research shows that ‘quality of the mentoring and mentoring relationships’ is the central strategy for effective implementation of any mentoring programme. 14 Gender biases is always secondary to it and can be dealt with overcoming communication barriers and maintaining conducive relationship.
In concordance with the current study, several research works showed evidence to promote mental health of medical students through mentorship programmes. 15, 16 Psychosocial issues among aspiring doctors, especially in early phase of training is common and various structured mentorship models need to be incorporated as an integral part of medical curriculum to improve academic and mental wellbeing of the students. In our study, subjects suggested improvement strategies in terms of timeframe and communication modes. Appropriate time scheduling, increase in number of mentoring sessions and the use of alternative meeting online methods like Zoom, Microsoft Teams etc. may enhance the impact of programme.
There were some limitations in current study. It was carried out at only one institution, so the results could not be generalized. Due to time constraints and limited number of trained mentors, control groups were not included in the study. Subjects’ performance for longer period could not be evaluated which may be a crucial area of impending research.
Conclusions
The present study observed a positive gain in psychosocial adjustments of newly admitted medical students. Both students and mentors showed favourable attitudes towards the programme and perceived numerous benefits, including personal and professional development. Further research is contemplated to analyze the complex process of mental problems of medical students.