Introduction
The prevalences of Atherosclerotic cardiovascular diseases (ASCVD) are rising worldwide. Atherosclerosis is the major pathophysiological process in ASCVDs. Atherosclerosis is a smoldering immunoinflammatory process where lipoproteins are acting as a fuel.1 Thus lipoproteins are the major contributor in atheromatous plaque formation. Among atherogenic lipoproteins LDLc has long been considered as major lipoprotein & thus it became major therapeutic target in all lipid lowering therapies. ASCVD risk is linearly associated with LDLc level. It has been demonstrated that with each mmol/lit decrease in LDLc level is associated with 20%-25% reduction in the risk of major ASCVD events. 2, 3 We have been assessing lipid derived ASCVD risk by looking at traditional lipid parameters for the last few decades. But traditional lipid parameters do not reflect the entire atherogenic lipoproteins in the plasma like Lp(a), apolipoprotien-B. 4 It has been found in several recent studies demonstrated that a subset of patients, even with optimal LDLc levels they continue to get ASCVD events & atherosclerosis process progression. This phenomenon has been termed as “residual lipid risk” which can’t be identified by measuring LDLc level alone. Residual lipid risk is the difference between the estimated LDLc value and the actual quantity of circulating atherogenic lipoprotein particles.5 Non HDLc comprises of cholesterol carried by all potentially atherogenis lipoproteins including LDLc, VLDL, Lp(a) , remnant lipoproteins. Apolipoprotien-B represents the total number of atherogenic lipoproteins in the plasma as each atherogenic lipoprotein particle contains one molecule of apolipoprotein-B.6 LDLc represents the total cholesterol concentration of LDL, IDL, Lp(a). However LDL cholesterol level does not reflect the LDL particle number & size.7 For example, at the same level of LDL cholesterol people with small sized LDL particle will have more number of LDLc particles than people with large sized LDL particle. As it takes more small sized LDL to traffic a given mass of cholesterol molecules per litre/deciliter. 7 We know small dense LDL is more atherogenic than large buoyant LDL particle. 8, 9 In most circumstances Apolipoprotien-B, Non HDLc are highly correlated with each other but not identical as apolipoprotien-B & non HDLc in addition to LDLc they also include triglyceride rich lipoproteins.10 Lipoprotein-a is included in all three measurements. Among statin treated patients more pronounced discordance exist between these parameters as statin lower LDLc more effectively than other two parameters. 11 So it is important to identify this concordance & discordance pattern particularly in statin treated patients, otherwise they might have discordantly high appolipoprotien –B levels and they remain at higher risk for ASCVD events despite attainment of optimal LDLc. If we are able to identify those subset of patients, we can take appropriate steps like statin intensification, addition of non-statin therapy or more aggressive procedure like lipid apheresis. To date very small number of studies have been conducted to examine this relationship between these lipid parameters in statin treated patients. So the present study was done to identify how many percentage of statin treated patients apolipoprotein –B & non HDLc were discordantly high that would help in identifying residual lipid risk among them.
Objectives
To find out % of study population who have achieved target LDLc goal after receiving statin therapy.
To find out % of study population in whom apo B level/ non HDLc level was not under desired target despite attaining target LDLc level.
To find out % of study population in whom LDLc levels were discordant with non HDLc and with apolipoprotein B.
Materials and Methods
This was an observational cross sectional single centre based study done in the department of General Medicine of Malda Medical College & Hospital, Malda,W.B. from April,2022 to May,2023.We included those patients who were at high risk for atherosclerotic cardiovascular diseases (ASCVD) and were on statin therapy for primary prevention .As per Lipid Association of India (LAI) recommendation, high risk for ASCVDs was considered in whom three or more major ASCVD risk factors were present or diabetes with one other major risk factor were present. 12, 13 We didn’t include those having history of CV events or features of target organ damage as they had more stringent lipid goal and supposed to get more intense statin therapy or non-statin therapy. We included only those patients who were on stable statin therapy for at least last three months. Those patients who had renal and hepatic impairments and in whom secondary causes of dyslipidemia like hypothyroidism, nephrotic syndrome, obstructive liver disease were present, they were not included in the study.After detail explanation of study procedure, informed consent was taken from each eligible participant and Institutional Ethical Clearance was obtained for the study. Detailed history, anthropometric measurements & clinical examination were carried out in all patients. Then 12 hour fasting blood samples were taken for estimation of lipid profile & apolipoprotein-B from all participants. Fully automated analyzer COBAS 6000 was used for lipid profile estimation & apolipoprotein –B level was measured by Immunonephelometry method. As per L.A.I. recommendation lipid goals for high risk patient that we consider in our study were LDL level less than 70mg/dl, non HDLc level less than 100mg/dl & apolipoprotein –B level less than 80mg/dl 14. If plasma triglyceride level was more than 150mg/dl,we considered as high & low HDLc means less than 40mg/dl & 50mg/dl in male and female respectively .Non HDLc was calculated as difference between total cholesterol & HDLc.
Statistical analysis
Categorical variables were presented as frequency and percentage whereas continuous variables were presented as mean ± standard deviation or percentiles. Independent t-test was used to compare mean (±standard deviation) of continuous variable between two groups. Pearson correlation test was used to assess correlation between two continuous variables. P value < 0.05 was considered statistically significant. As there was no standard cut-off point for discordance, this study selected the recommended target values as the cut-off
points. For high risk patients lipid goals are LDL-C: <70mg/dl, non-HDL-C:<100
mg/dl, apoB:<80mg/dl. To define discordance, which was defined as LDL-C ≥ the cut-off point and non-HDL-C or apoB < the cut-off point or vice versa.
Thus, participants were divided into four groups:
Low/low (LDLC < the cut-off point and non-HDL-C or apoB <the cutoff point),
Low/high (LDL-C < the cut-off point and non- HDL-C or apoB ≥ the cut-off point),
High/low (LDL-C ≥ the cut-off point and non-HDL-C or apoB < the cut-off point),
High/high (LDL-C ≥ the cut-off point and non-HDL-C or apoB ≥the cut-off point).
Results
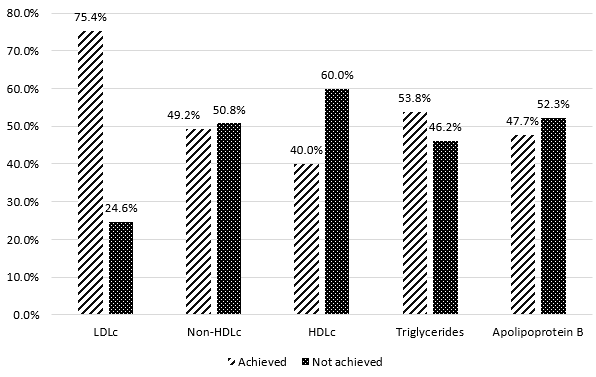
A total of 65 patients were enrolled in this study. The mean age of the study population was 53.48 ± 9.60 years. Among them 43.17% patients were between 50 to 60 years of age. Majority of enrolled patients were males (75.4%). A total 39 patients (60%) were overweight or obese as per Indian cut offs. Among the enrolled participants 32 patients (49.2%) had history of type 2 diabetes mellitus & 41 patients (63%) were hypertensive. A total 23 patients (35.3%) were smokers & family history of premature CVDs was present in 67.9 % cases. [Table 1] We observed over all 75.4%of study participants had achieved recommended LDLc goal with statin therapy & remaining 24.6% patients had not reached their LDLc goal despite statin therapy. We found 49.2% patients attended non HDLc goal & 53.8% patients attended triglyceride goal with statin therapy. We observed more than half of the study population 52.3% did not achieve their target apolipoprotien B level with the ongoing statin therapy. The plasma HDLc levels were low in 60% of study population that is below 40mg/dl for males & below 50 mg/dl for females.[Figure 1] The mean values of all lipid parameters including Apolipoprotien- B among study participants are given in Table 2. There was statistically insignificant differences in all lipid profile parameters between males & females.[Table 2] The mean value of LDLc with statin therapy was 63.08 ± 22.08 mg/dl & mean value of apolipoprotien B was 79.69 ± 21.05 mg/dl.The correlation between LDLc & apolipoprotien-B was found to be moderate and positive (r= 0.460, p>0.001). [Figure 2] That means with the increasing LDLc values, our participants had higher apolipoprotien –B values.On concordance & discordance analysis, when we compared LDLc versus apolipoprotien-B based on specific target values of these variables, we found 30.8% patients were categorized into low/high discordance group that means their plasma LDLc values were below target level that is below 70mg/dl but their plasma apolipoprotien –B values were out of target that is below 80mg/dl. The 44.8% patients fall into low/low concordance group that means they had attended recommended lipid goals both for LDLc & apolipoprotien-B with the statin therapy. The 21.5% patients were categorized into high/high concordance group means both the levels were beyond the target. [Figure 2a] Similarly when we compared them based on their median values 15.4 % patients were categorized into low/high discordance group, 32.3% patients were categorized into low/low concordance group, 35.4% patients had fallen into high/high concordance group and 16.9% patients were categorized into high/low discordance group. [Figure-2b]
Figure 2
a: Scatter plot of concordance and discordance between apolipoprotein B & LDL cholesterol by respective target values; b: Scatter plot of concordance and discordance between apolipoprotein B & LDL cholesterol by median values.(Median of LDL cholesterol = 63mg/dl; Median of Apolipoprotein B = 84mg/dl.)
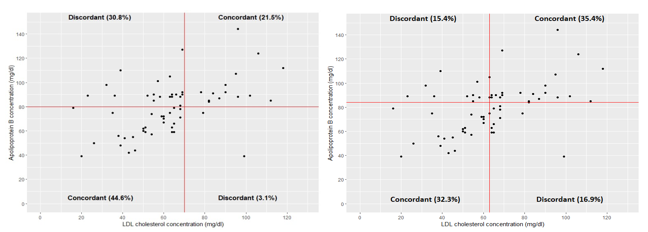
Figure 3
a: Scatter plot of concordance and discordance between non HDLc & LDLcholesterol by respective target values; b: Scatter plot of concordanceand discordance between non HDLc & LDL cholesterol by median values. Median of LDLcholesterol = 63mg/dl; Median of Non-HDL cholesterol = 100mg/dl)
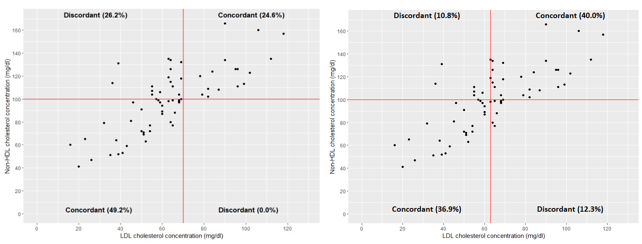
Table 1
Clinical profile of the study population (N=65)
Table 2
Mean ± SD study variables in the overall study population, males and females.
The correlation between LDLc & non HDLc was found to be high & positive & attained statistical significance. (r=0.07, p<0.001) When we compared LDLc versus Non HDLc based on their specific target values, we found 49.2% of study population had fallen into low/low concordance group, in whom both LDLc & non HDLc values were below the specific target after statin therapy. We observed 24.6% patients were categorized into high/high concordance group means their LDLc & non HDLc values were above the recommended goal despite statin therapy. We found 26.2% patients were categorized into low/high discordance group that means they attained LDLc goal but their non HDLc goal had not been met with statin therapy. We did not find any patients in high /low discordance group. [Figure 3a] Similarly when we compared them based on their median values of LDLc & non HDLc, we got 36.9% patients were categorized into low/low concordance group, 40% patients had fallen into high/high concordance group, 12.3% patients were categorized into high/low discordance group and 10.8% patients were into low/high discordance group. [Figure 3b]
Discussion
We observed maximum number of patients who were on statin therapy & had high ASCVD risk, were between 50to 60 years of age .This finding is consistent with our South-Asian ethnicity as we are developing cardio metabolic diseases one to two decades earlier than our western counterparts. 15 We found despite statin therapy 24.6% of study population were not achieved recommended LDLc goal. Although we didn’t look into whether they were put an optimal doses of statin & compliance was not calculated. Among our study participants prevalence of obesity, Hypertension, diabetes mellitus were 60%, 63% & 42.9% respectively. When we consider our national prevalence of these diseases, our study findings were much higher as we recruited selectively high risk patients .We observed more than half of study population (52.3%) didn’t met their recommended apolipoprotein –B goal that is as per LAI recommendation below 80 mg/dl. So they may need statin dosage intensification. Among statin treated patients, apolipoprotein –B discordantly high in respect to LDLc level in 30.8% cases & non- HDLc was discordantly high in 26.2% cases. This finding is consistent with the study done by Qu et al., 16 they observed LDLc to be discordant with apolipoprotein-B in 31% cases & with non HDLc in 20.1% cases in their study cohort. They also reported the brachial artery pulse wave velocity (baPWV) which is considered as a marker of subclinical atherosclerosis,17 was greater in those with higher apolipoprotein-B or non HDLc levels. In the adjusted logistic regression model, low LDLc and high apolipoprotein-B or non HDLc discordance were associated with risk of arterial stiffness (OR:13.41). 16 So these discordant group of patients need to be identified in order to take necessary steps to reduce the residual risk of CV events. The LDLc has long been considered as major therapeutic target of lipid lowering therapies while non HDLc & apolipoprotein –B are still controversial targets. Nevertheless many studies have demonstrated non HDLc and apolipoprotein-B are much superior predictors of arterial stiffness. In several studies conducted in China,non HDLc was found to be more stranger predictor of baPWV than other lipid parameters.18, 19 Jhanmesen et al.20 did concordance discordance analysis and they concluded that statin treated patients, elevated apolipoprotein –B and non HDLc ,but not LDLc , are associated with residual risk of all cause mortality & myocardial infarction. It has been observed that the amount of cholesterol within lipoprotein particles very substantially. The analysis of INTERHEART study demonstrated that when apolipoprotein in B level is higher than non HDLc level that is when cholesterol depleted apolipoprotein –B particles are present, cardiovascular risk is increased, where as when non HDLc level is higher than apolipoprotein –B level that is when cholesterol enriched apolipoprotein –B particles are present ,cardiovascular risk is less than the reference concordant group.21 When the mass of cholesterol per apolipoprotein –B particle is normal ,all three measures are concordant. But when mass of cholesterol within apolipoprotein –B particles is either greater or lesser, LDLc & non HDLc are discordant. In both the circumstances the number of apolipoprotein B particles is not accurately represented by measures of mass of cholesterol within them. 21 So, probably lipoprotein particle number, size are more critical determinant of cardiovascular risk than the mass of cholesterol within them.
An important observation of our study was majority of apolipoprotein –B discordantly high group of patients also had higher triglyceride level, so probably it supports the notion that in presence of high triglycerides, LDLc gets oxidized & becomes small dense form & that is considered more atherogenic than large buoyant LDL particle. 22 So elevated triglyceride level in statin treated patients may indicate higher CVD risk. So triglyceride can be the co-primary target in high risk patients while deciding optimal lipid lowering therapy. Another observation of the present study was, a significant number of statin treated patients (60%)had low HDLc levels that is below 40mg/dl. in males & below 50mg/dl in females. Whether statin has a causal role in this or it is due to presence of metabolic syndrome, we couldn’t conclusively comment upon this as we didn’t have baseline HDLc values in study cohort. Future studies only can ascertain this.