Introduction
In the recent decades, stress has become a term of popular parlance with respect to psychobiology. Stress denotes the aftereffects of failure of an organism or human to adapt appropriately to emotional or physical challenges, whether actual or imagined.1 The relationship between stress and illness is not linear. It varies from person to person and depends on personality make up, genetic vulnerability, coping skills and social support.
Stress has become an unavoidable part of our daily lives. With the increase in needs of an individual or family and tight competition for essentials of living, stress has started to affect the emotions and reactions of an individual. Busy lifestyles, tight competition at work, financial commitments, marital problems, bereavement, chronic illnesses are some of the common causes of stress that leads to ill effects. We cannot evade from stress in our lives and stress at certain level is not always harmful. Consequences of stress depends on its type, intensity, duration and temporal association. 2
Most of the effect of stress on mind and body are due to the increased activity of the sympathetic nervous system and increased secretions of adrenaline, cortisol, neurotransmitters, prostaglandins and some enzymes. The areas mainly affected by stress are brain and nerves, muscles, joints, cardiovascular system, stomach, skin and reproductive system. Stress response in controlled by the hypothalamus.3
For better understanding of stress and its consequences, it would be just to quantify the effects of stressful life events. A life event is a significant occurrence involving a relatively abrupt change that may produce serious long-lasting effects. 4 Stressful life events can result in a variety of mental and physical health problems. Perception of stress is a subjective phenomenon and hence, same life event can be stressful to some and not to others. An individual’s personality make-up and vulnerability influence his perception of stress and in turn determines his reaction to the same. 5
Depressive disorders are characterized by persistent low mood, lack of interest in otherwise pleasurable activities, easy fatiguability, persistent sleep and appetite problems, lack of confidence, memory lapses etc. The universal prevalence of depression is around 3.8%.6 While the genetic liability of depressive disorder is around 30-40%, there is increasing evidence that it is caused by interplay between neuronal circuitry and stressful life events in vulnerable individuals.7 Decrease in gene expression of BDNF and the glucocorticoid receptor following stressors has been well documented.8 There is a large body of evidence suggesting the pivotal role of life events before the onset of depressive episodes.9, 10, 11, 12
Schizophrenia is a major psychiatric illness which can affect the thought, cognition, perception and behavior of the affected individual. The universal prevalence of schizophrenia is around 0.32%.13 The role of life events in the onset of schizophrenia is not as robust as in depressive disorders. Lukoff and Ventura, in a study reported in 1984, observed that stressful life event clustered around 3-4 weeks prior to the onset of schizophrenic episode.14 Several studies have linked stress to relapse in schizophrenia patients rather than the onset.15, 16, 17
For better conceptualization of stressful life events preceding psychiatric illnesses, one has to move from vague notion of stress to a concise and measurable description of the nature of life events with a degree of reliability and specificity. In this study, we aim to compare the presence and nature of life events preceding the onset of depressive disorders and schizophrenia, in a rural Indian setting.
Materials and Methods
This observational study was conducted in a tertiary medical college in rural south India. Institutional ethical clearance was obtained before the start of the study. A total of 92 participants, out of which 46 schizophrenia patients and 46 depressive disorder patients, fulfilling the inclusion criteria, attending psychiatry OPD during an 18-month period, were selected for the study. The patients and their family were explained about the nature of the study. Confidentiality about the identity and data gathered were assured. Written informed consent was taken before enrolling the participant into the study.
Study tools used
Semi-structured proforma to collect socio-demographic data.
Presumptive stressful life events scale (PSLES): Inventory of 51 items, each item having a weighted score.
Data collected was entered in Microsoft excel and analyzed using Epi-info. Descriptive statistics such as proportions, means and standard deviations were calculated. Z-test for difference between proportions and means were used wherever applicable.
Results
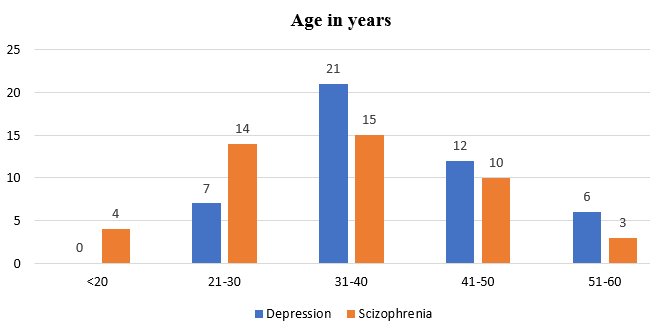
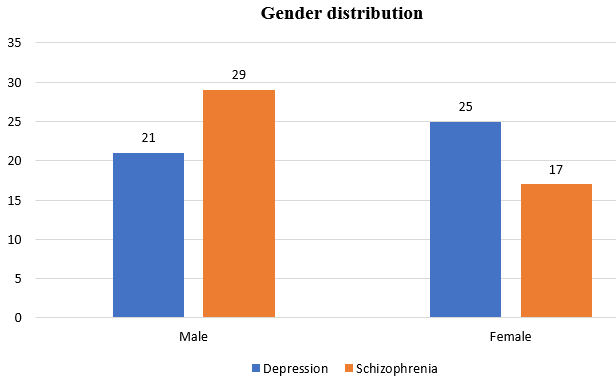
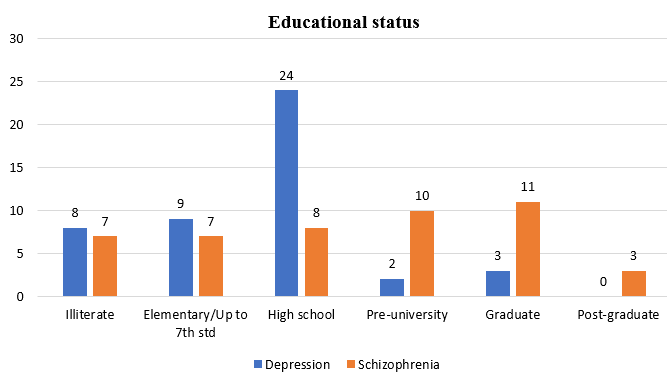
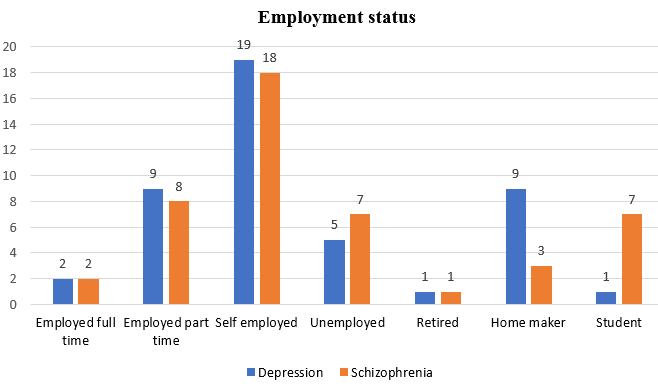
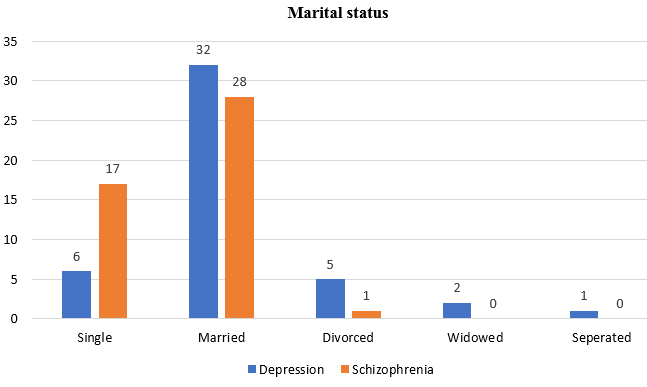
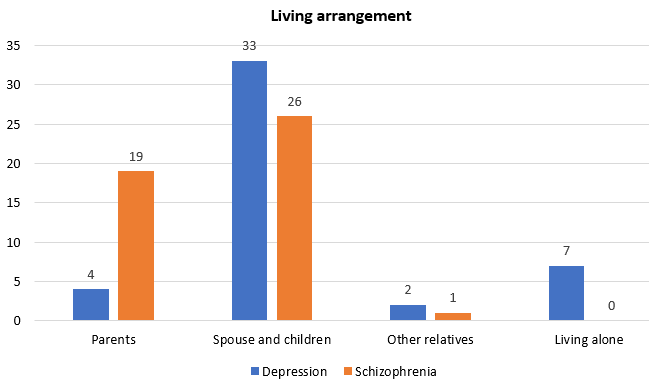
In this study, the majority of onset of schizophrenia was between 21-40 years and for depressive disorders, it was between 31-50 years as shown in Figure 1. There was no statistically significant difference between males and females in both the groups as shown in Figure 2. Majority of the subjects in both the groups were self-employed as shown in Figure 4. Majority of patients in both groups were married and living with their spouse and children as shown in Figure 5, Figure 6.
Life event score for depressive disorders was significantly higher than schizophrenia group as shown in Table 3. The mean time lag between the life event and onset of depression was around 2.7 months while for schizophrenia it was around 5.54 months, as shown in Table 2. The most commonly reported life events were family conflict, large loans, marital conflict, son or daughter leaving home and illness in family members, as shown in Table 1. All of these life events were significantly higher in depressive disorders.
Table 1
Frequency of preceding life events in depression and schizophrenia
Discussion
The age of onset of schizophrenia and depression in our study was in concordance in facts established in earlier researches. 3, 6, 13, 18, 19 Majority of the participants in this study were farmers, shepherds, daily wage workers or owners of small shops. This is a typical occupational pattern in rural south India. Majority of patients in both groups were married and living with their spouses and children. This can be explained by the dependent culture in India, which strengthens the social support system.
In this study, the life event score for depression was much higher when compared with the schizophrenia group. This is in concordance with many of the earlier studies.9, 10, 20, 21, 22 In schizophrenia, life events were related more to relapses rather than onset as shown in many studies.23, 24 Research in the past has shown that life stress merely act as final impetus towards illness in a person strongly predisposed to schizophrenia because of an underlying diathesis.23
The time lag between the life event and onset of depression in our study was shown as 2.74 months and for schizophrenia, it was 5.54 months. This was in contrast in some of the earlier studies which showed not more than a one-month time lag between life event and onset/relapse of schizophrenic symptoms.14, 25 This could be sometimes due to the lack of awareness of prodromal symptoms of schizophrenia among rural Indian population. In rural India, mentally ill people are usually taken for medical consultation only when they exhibit disruptive behaviors.
Although literature suggests that life events play an important role in precipitation and relapse of psychiatric disorders, this relationship is not straight forward. The relationship between stress and illness varies with preexisting vulnerability factors. The differences in social support system, skills, attitudes, beliefs, and personality characteristics renders some individuals relatively immune to stress induced illness and make others relatively susceptible. The protective factors against stress, in our country, include dependent family culture, and relatively low cost of living. Education from young ages should focus on stress management, healthy daily routine, emphasizing quality communication among family members, financial management, problem solving skills, decision making skills and improving coping skills. Importance of self-care should be ascertained in family and school. Future research may focus on other intervening variables in order to reduce the incidences of stress induced illnesses.