Introduction
Shoulder disorders are the third most common musculoskeletal condition requiring surgical correction by shoulder arthroscopy.1, 2 Regional anaesthesia alone or in combination with general anaesthesia are employed for safe conduct of these surgeries. 3, 4, 5, 6 Post operative pain after surgery is severe and exacerbated by movement during rehabilitation.7 Out of the various regional anaesthesia modalities,3 Interscalene brachial plexus block (ISBPB) 7, 8 provides excellent surgical anaesthesia, post-operative analgesia, decreases postoperative opioid consumption and decreases postop PACU length of stay.9, 10 To increase patient comfort as these surgeries, require a beach chair position or lateral position and a lot of irrigation fluid, a combination of ISBPB with GA is used. 4, 5, 10, 11 Despite the benefits, concomitant paralysis of the ipsilateral diaphragm is an unavoidable consequence of ISBPB when a conventional volume of LA (10-45ml) is used with landmark or peripheral nerve stimulator technique6, 12, 13 due to the proximity of the phrenic nerve to the brachial plexus. A range of modifications and alternatives to ISBPB have been tried to minimize the respiratory impact of phrenic nerve palsy such as reducing the concentration of the local anaesthetic used,14 reducing the volume of LA used. 14, 15 changing the drug,16 and different approaches to ISBPB.17 To date there have been no thorough assessment of the clinical value offered by any of the above strategies. Ultrasound guided ISBPB is carried out by depositing the drug around the target structures and lesser volumes18, 19, 20, 15, 16, 21 can be given which have been shown to be of some significance in reducing the incidence of hemi diaphragmatic paresis (HDP).18, 19, 20, 15, 22, 23, 24
Materials and Methods
A prospective randomized interventional comparative study was conducted for a duration of eighteen months and sample size was calculated as 30 patients in USG guided ISBPB and 30 in PNS guided ISBPB study group based on data by previous studies. 22 Patients of 18–65-year age group belonging to either sex or ASA grade I/II scheduled to undergo arthroscopic shoulder surgery were included. Patients with preexisting lung disease, BMI>30kg/m2, allergy to the LA or any of its component, any known coagulopathy or local site infection were excluded from the study.
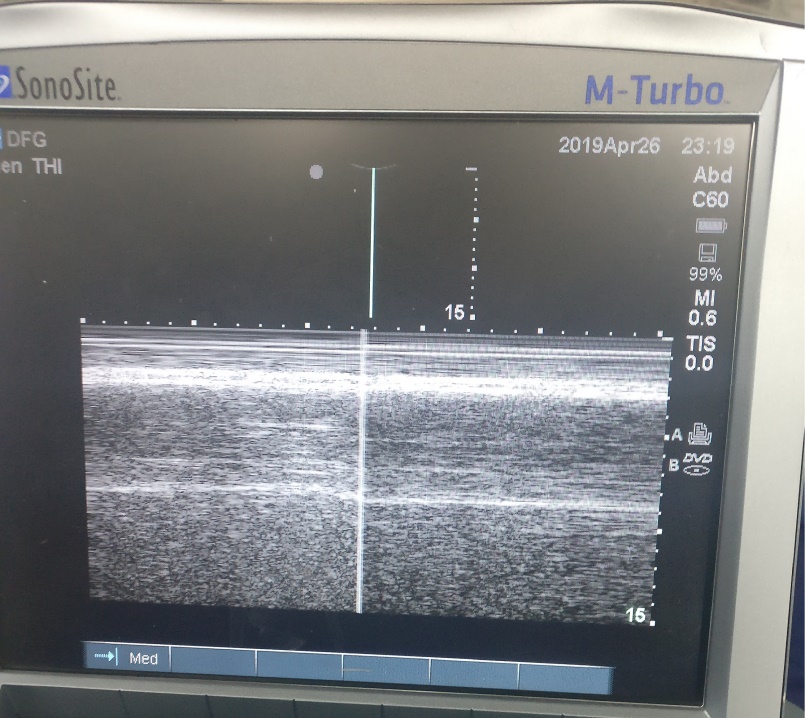
All the patients were made to be nil per oral overnight and received Tab Alprazolam 0.25mg the night before surgery. Advantages and side effect of both techniques were explained to the patients, and they were taught how to perform handheld spirometry 25 and use the Numeric Pain Rating Scale. 26 Before performing the block, a Baseline dyspnoea score was obtained according to the modified Borg scale. 27 Baseline diaphragm motion was noted using ultrasound on the side to be blocked to compare the movement after giving the block. Each patient was asked to perform the sniff manoeuvre in supine position, the diaphragm was visualized with ultrasound and a normal caudal versus paradoxical cephalad movement was noted. 28 (Figure 1)
Baseline pulmonary function tests (PFT)
Forced vital capacity (FVC), Forced expiratory volume in 1 second (FEV1) and Peak expiratory flow rate (PFR) values were obtained using the handheld spirometer in accordance with lung function testing of the American Thoracic Society (ATS). PFTs were measured 3 times in sitting position and average of 3 measurements was taken (25). (Figure 2)
Patient was shifted to preoperative holding area, standard monitors were attached, and baseline parameters were noted. An IV access was secured, IV fluids were started, and Inj. Midazolam 1-2 mg was given for sedation to all patients.
GROUP – USG: In the supine position with the head turned to the contralateral side and under all aseptic precaution a 10-15 MHz linear array ultrasound probe was used. Sternocleidomastoid and scalene muscles were identified in a short axis view. C5-C6 roots of the Brachial plexus nerve were identified and confirmed by tracing them joining to form the superior trunk. Skin infiltration was done with 1% lignocaine using 25 G needle, thereafter a 22 G, 50 mm short, bevelled nerve block needle was used from the lateral side of the probe and positioned between the anterior and middle scalene muscles. Needle tip was adjusted caudally toward the C6 trunk; 0.5% bupivacaine was injected slowly after ensuring negative aspiration for blood and excluding severe pain or resistance to injection. 10ml of the drug was given in a multi-injection technique making sure to avoid medial and rostral spread. If there was a spread appreciated in real-time, the needle tip was directed more caudally. Local anaesthetic spread was observed at the end for any collection anterior to the scalene anterior muscle.
GROUP – PNS: With the patient in a similar position and under all aseptic precautions, ISBPB was performed with 22G, 50 mm PNS insulated needle using PNS (Multistim i3640, Pujunk, Hospimedica, Germany). After skin infiltration with local anaesthetic, interscalene groove was identified by palpation followed by introduction of the PNS needle at the level of the cricoid. The needle was advanced until contractions of either deltoid or biceps (C5, 6 roots) were obtained. When these contractions persisted at the stimulation current 0.3- 0.5 mA (0.1ms and 1 Hz frequency), 0.5% bupivacaine was injected slowly in increments to a total dose of 10ml. (Figure 3) Negative aspiration for blood was confirmed and severe pain or resistance to the injection was excluded.
The sensory block was assessed (using pin prick) in dermatomes C4-C8(Table 1), 30 min after the block The block was deemed successful when complete sensory anaesthesia was achieved in dermatomes C5 and C6.
Table 1
Assessment ofsensory block using surface anatomy.
|
Dermatome Level |
Anatomical Landmark |
|
C4 |
Tip of the shoulder |
|
C5 |
Skin over the deltoid muscle |
|
C6 |
Tip pf the thumb |
|
C7 |
Tip of the middle finger |
|
C8 |
Tip of the little finger |
Full motor blockade of the upper extremity was confirmed by testing motor functions such as shoulder abduction, elbow flexion and extension, finger abduction and adduction, thumb abduction on a scale of 0 to 5 (Table 2) were measured 30 min after the block.
Table 2
Assessment ofmotor blockade
Movement of diaphragm was measured in the supine position using a real time M mode Ultrasound of hemi diaphragm with the help of a 17 mm 1-5 MHz curved array ultrasound probe on the ipsilateral side as of the block to assess HDP. HDP was positive when there was a 50% reduction in diaphragmatic movement or a paradoxical movement (the cephalad motion during inspiration). Assessment of HDP was done at 30 min post block and at 1Hr in post anaesthesia care unit.
Pulmonary Functions tests (FVC, FEV1 and PFR) were recorded at 30 minutes post block and were monitored every hourly in postoperative period till 6 hrs in the recovery.
Immediate complications, such as vascular injury, Horner's syndrome, hoarseness of voice, respiratory distress, and spinal / epidural injection were assessed during this period of block procedure as well as post-operatively.
All patients received general anaesthesia, 30 min after the completion of block. Patient was sifted to the operative room; ASA 2 monitors were attached, and baseline parameters were noted. Patients were induced according to institute protocols with Inj. Fentanyl (2mcg/kg), Inj. Propofol (2 - 2.5 mg /kg), muscle relaxation was obtained with Inj. Vecuronium bromide (0.1 mg /kg) to facilitate intubation. All patients were mechanically ventilated, and anaesthesia maintained using nitrous oxide, oxygen, and isoflurane (0.5-1%) mixture in a closed circuit with supplemental doses of Vecuronium bromide. Entropy was used to measure the depth of anaesthesia and whenever required, Inj. fentanyl (maximum 2 mcg/kg) was administered. All patients were administered Inj. Ondansetron 0.1mg/kg 20 minutes before the end of surgery.
Residual neuromuscular blockade was reversed with Inj. Neostigmine 0.05 mg/kg and Inj. Glycopyrrolate 0.01mg/kg, trachea was extubated, and patients were shifted to recovery at the end of the surgery. In the postoperative period at 1 hour, assessment of HDP was done again by ultrasound, Dyspnoea Score, PFT’s and evaluation of postoperative pain was done hourly using a Numeric Pain Rating Scale (NPRS). Rescue analgesia in the form of Inj. Paracetamol 1gm I.V. was administered on demand or if NPRS score is > 4 and its time was noted. If pain did not subside by 30 minutes after giving paracetamol, Inj. Tramadol 2mg/kg I.V was given as rescue analgesia and total amount of analgesia required were also noted. The time of rescue analgesia was recorded as the duration of postoperative analgesia.
Ethics
The study was conducted in the department of Anaesthesia and Intensive care at Vardhaman Mahavir Medical college and Safdarjung Hospital, New Delhi after obtaining approval from the institute ethics committee and registering the study with clinical trial registry of India (number CTRI/2018/05/013613).
Results
Both the groups were comparable in terms of age, weight, sex, height, BMI, ASA status. Intraoperative fentanyl requirement was not significantly different amongst the two groups and the haemodynamic were comparable. Motor and sensory effects were adequate and comparable between both the groups.
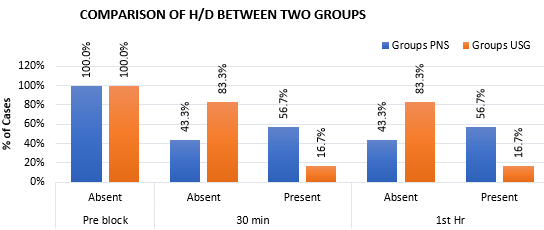
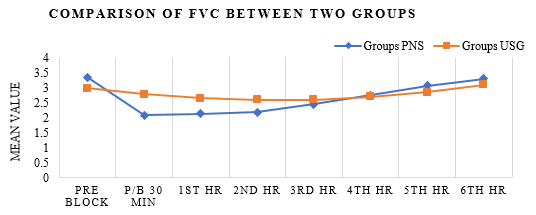
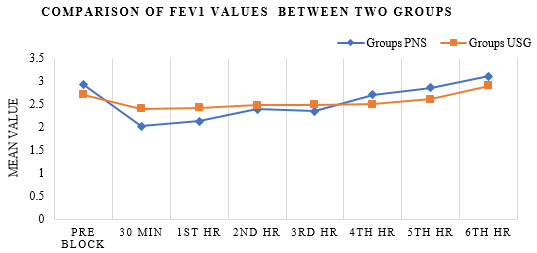
During the study only one patient complained of Dyspnoea from the PNS group at 1st and 2nd hour postoperatively, despite this the dyspnoea scores were comparable amongst the two groups. HDP was present in 17 patients belonging to PNS group and 5 patients from USG group at 30 mins and 1 hour post block. (Figure 4) Spirometry values (FVC, FEV1 and PFR) were significantly reduced at 30 mins and 1 hr post block (Figure 5, Figure 6, Figure 7).
NRS score was comparable till 6 hrs postoperatively when each patient received rescue analgesia. Complication of Horner’s syndrome was seen in 3 patients belonging to PNS group and 1 patient of USG group.
Discussion
ISBPB is one of the most common and reliable techniques for regional anaesthesia of the upper limb surgeries in combination with general anaesthesia. It is associated with several complications, the most common being the phrenic nerve palsy, which occurs in 100% of patients using conventional techniques. 12
Over the period ISBPB has evolved from its traditional landmark approach to PNS guided and USG guided techniques. Attempts were made with both the techniques to decrease the complications such as HDP either by changing the volume 14, 18, 19, 20, 15 or by changing the site of injection. 17
The incidence of HDP was compared by Renes et al among PNS and USG guided interscalene block and found a significant reduction in the incidence of HDP in the USG group. 15 They hypothesized that changing the location of the block farther away from upper cervical roots and therefore phrenic nerve may lead to decreased HDP. However, the safety of administering ISBPB at C7 level near its tubercle is to be challenged due to the close proximity of the vertebral vessels. Contrary to this, Sinha et al. compared USG guided 20 ml and 10 ml of LA injected at the same cricoid level and found that decreasing the volume did not decrease the incidence of HDP. 18
Most of the patients in our study were posted for Bankert’s repair for recurrent shoulder dislocations, a few for supraspinatus tear and very few for arthroscopic evaluation and management accordingly. The incidence of HDP was statistically significant between both groups with a p value 0.001 (Figure IV) which is consistent with the findings of Ghodki PS et al 22 in term of incidence of HDP. In their study none out of 30 patients in USG group had HDP and 12 out of 30 patients in PNS group developed HDP (p <0.0001). Similarly, Renes SH et al 15 reported incidence of HDP in 2 patients out of 15 pts in USG group and in 14 out of 15 pts in PNS group (p value <0.0001). However, Sinha SK et al 18 reported the incidence of HDP within 15 mins after performing block in 14 of 15 patients in each group (Low volume and High volume).
Pulmonary function test
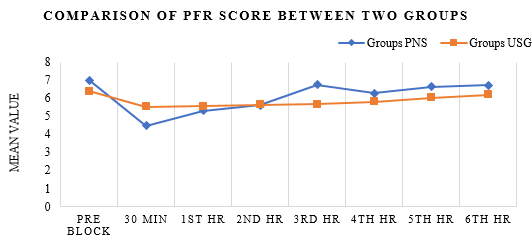
Pulmonary function test (FVC, FEV1, PFR) with spirometer were measured in both the groups at pre block (baseline), post block 30 min and from 1st hr to 6th hr post op.
FVC values were significantly reduced at post block 30 min, 2.08±0.71 for PNS group and 2.78±0.71 for USG group with p value of 0.0002 while 2.14 ± 0.57 for PNS group and 2.65± 0.57 for USG group at 1st hr with p value of 0.0004 (Figure 5).
FEV1 values were reduced for PNS group and USG group at 30 min post block 2.02±0.60 and 2.40±0.53 respectively with p value 0f 0.005 (statistically significant), at 1st hr. post op it was 2.13±0.57 for PNS group and 2.43±0.49 for USG group with p value of 0.017 which was statistically significant (Figure 6).
PFR values were 4.47 ± 1.24 for PNS and 5.52 ± 1.53 for USG group respectively with p value of 0.002, which was statistically significant at post block 30 min. PFR values were comparable at 1st hr post operatively.
Our findings were consistent with those of Ghodki PS et al 22 who reported statistically significant decrease in FVC, FEV1 and PFR value for PNS group as compared to USG group at post block 20 min and at immediate post op (p value <0.0001). Similarly, Renes et al reported significant decrease in PFT values (FVC, FEV1, PFR) at 30 minutes post block.
Dyspnoea score
Dyspnoea score was measured in both the groups at pre block, post block 30 min and 1st to 6th hour post operatively, which was comparable between both the groups with p value 0.321. Only one patient in PNS group complained about dyspnoea at 1st and 2nd hour post operatively suggesting dyspnoea is not a predictor for phrenic nerve palsy. 24
Sala blanch et al have reported no incidence of dyspnoea in their study despite of having 100% incidence of HDP. 29
Level of sensory and motor blockade was assessed at 30 min. post block in both the groups in term of block success rate, dermatomal spread, and motor power assessment which were found to be comparable. Group USG had more distal spread (C7, C8 - 30 and 22 cases respectively) and less proximal spread (C4 – 4 cases) in comparison of PNS group (C7, C8 and C4 – 19, 14 and 16 cases respectively). This finding was consistent with Kapral et al, 21 which demonstrated that ultrasound guidance is more effective than nerve stimulator guidance in blocking the distal sensory areas of the brachial plexus. Similarly, Ghodki et al 22 reported that the C5 dermatome block was achieved in all patients of both the groups (PNS and USG) and Group USG had a higher incidence of C7 and C8 level block, and a lower incidence of C4 level block compared to Group PNS (P < 0.05).
Block success rate was 100 % for both of group, similar findings were found in the study done by Renes et al 15 (block success rate of 100% for USG group and 93% for PNS group with p value of 1), Ghodki PS et al 22 (USG group 100 % and PNS group 99% p value >0.05) and Kapral et al21 (PNS group 92%, USG group 99%).
NRS, rescue analgesia and duration of post op analgesia
NRS at 1st to 6th Hr. post op was statistically not significant between both the groups with p values >0.05. All patients of either group received rescue analgesia only in the form of Inj. PCM 1 gm IV if NRS was more than 4 or on demand of patient. Average duration of post op analgesia (in term of hrs after surgery) in group N was 9.31 ± 6.09 while in group U it was 7.26 ± 4.7, with p value of 0.290 which was statistically not significant. These results were relatable to the findings of Riazi et al 20 in which pain scores 30 min post-surgery were 1.1 ± 2.8 in low volume group and 0.3 ± 1.4 in high volume group which were not significantly different.
Complications
In our study only 3 patients in PNS group and 1 Patient in USG group presented with Horner’s syndrome, which was statistically not significant with p value of 0.058. There was no case of vascular puncture, recurrent laryngeal nerve palsy and any other complications. Similarly in the study done by Ghodki et al22 Horner’s syndrome in 2/30 pts in USG group and 6/30 pts in PNS group with p value of 0.24 was observed.
Conclusion
Therefore, from the above study we conclude that incidence of hemi diaphragmatic paresis is less after USG guided interscalene block than PNS guided interscalene brachial plexus block even with the 10 ml of local anaesthetic volume. Further we observe that the HDP does not alter the respiratory mechanics in a healthy patient sufficient to lead to respiratory distress as observed by dyspnoea. However, caution must be taken while performing even USG guided ISBPB in patients with known poor respiratory function or limited pulmonary reserve as they may present with clinical symptoms and lead to respiratory distress.