Background
Lung Carcinoma is considered one of the most common cancers globally, excluding those originating from the skin, with approximately 1.8 million cases being diagnosed annually and is the leading cause of death in both men and women.1 In the Indian population, the annual incidence of new lung cancer cases is approximately 63,000, with roughly one-third of cases presenting as the locally advanced stage. 2 The estimated total mortality attributed to lung cancer in India in 2020 was reported at 66,279, according to GLOBOCAN 2020. Significantly, lung cancer constituted the foremost cause of mortality among males, with 48,697 reported deaths. In females, the estimated mortality attributed to lung cancer was 15,062. 3 NSCLC is the most common histology (85%), while small cell lung cancer (SCLC) accounts for a minority, constituting only 15% of the total cases of lung cancer. 4 The therapeutic approach for NSCLC is contingent upon the disease stage. Surgical resection is the primary modality for achieving curative outcomes in patients presenting with early-stage disease. Conversely, individuals with more extensive intrathoracic disease benefit from concurrent chemoradiotherapy. 5, 6 In cases of advanced disease, the emphasis shifts to palliative management, incorporating systemic therapy and/or local palliative interventions. In contrast, SCLC demands a distinct therapeutic strategy, with systemic chemotherapy playing a pivotal role due to its widely disseminated nature at the time of presentation in nearly all cases.
Although the treatments in lung cancer have made great progress, more effective treatment strategies must consider patient selection and evaluate the prognosis of patients with lung cancer. For locally advanced and metastatic lung cancer cases, five-year survival rates are not promising. Prognostic determinants influencing survival outcomes have been previously established, encompassing factors such as age, gender, disease stage, performance status, weight loss, histopathological features, and serum levels of lactate dehydrogenase (LDH) and carcinoembryonic antigen (CEA) 7, 8, 9, 10, 11 While recent advancements have introduced new immunological and histological biomarkers like intercellular adhesion molecule-1 (IDM-1) and epidermal growth factor receptor (EGFR), 12, 13 these markers often involve considerable cost and time for measurement. Hence, the quest for a readily detectable and clinically pertinent prognostic factor persistently eludes researchers for lung cancer patients. 14 Hematological assessment, specifically the hemogram, represents a cost-effective and readily accessible diagnostic modality routinely administered to nearly all patients. Parameters such as leukocyte count, neutrophil count, lymphocyte count, and the Neutrophil to Lymphocyte ratio (NLR) serve as indicators of systemic inflammation and play pivotal roles in the mechanisms underlying cell-mediated destruction of cancer cells.15 Previous investigations have underscored the significance of cancer-related inflammation as a recognized marker in cancer, playing a crucial role in shaping the tumor microenvironment. The tumor immune microenvironment plays a pivotal role in the progression of tumors, orchestrating processes such as tumor angiogenesis, metastasis promotion, augmentation of cancer cell proliferation, and exerting influence on the efficacy of systemic treatments.16 Integral to tumor-associated inflammation are T lymphocytes and B lymphocytes, each significantly contributing to this intricate milieu.17, 18 The observed dysregulation in the balance between neutrophils and lymphocytes is hypothesized to emanate from tumor-induced hypoxia or necrosis coupled with anti-apoptotic effects.19 The NLR, a composite metric derived from circulating neutrophil and lymphocyte counts, serves as a quantitative indicator of this imbalance in individuals with neoplastic conditions, providing a reflective measure of systemic inflammation.
In recent examination, an elevated preoperative NLR derived from peripheral blood test, has surfaced as an independent and readily accessible prognostic biomarker linked to adverse survival outcomes across diverse malignancies. This includes but is not limited to colorectal cancer, breast cancer, gastric cancer, and esophageal cancer.20, 21, 22, 23 Moreover, a series of studies has methodically investigated the association between NLR and its prognostic implications, particularly within the framework of lung cancer. Within the spectrum of NSCLC, individuals presenting with elevated systemic inflammation at the time of diagnosis may manifest a more aggressive disease phenotype, warranting prompt and robust therapeutic intervention. Moreover, a rising NLR during the course of treatment may serve as an early indicator of impending disease progression and a heightened risk of treatment failure.24 The prognostic significance of inflammatory markers, such as NLR and Platelet-to-Lymphocyte Ratio (PLR), remains insufficiently elucidated within the context of SCLC.25 In a study conducted by Deng et al., elevated peripheral NLR before treatment emerged as an independent prognostic factor for unfavorable outcomes, including poor progression-free survival and overall survival, in patients diagnosed with SCLC.26, 27, 28 This present study aims to evaluate the prognostic implications associated with the NLR in individuals diagnosed with locally advanced and metastatic lung cancer.
Materials and Methods
Study design
The study aims to assess the prognostic value of the baseline neutrophil to lymphocyte ratio in patients with locally advanced and metastatic lung cancer. Conducted as a retrospective observational study in a hospital setting, it includes patients registered at the Dr. Bhubaneswar Borooah Cancer Institute, Assam from January 2017 to December 2017, who were diagnosed with histopathologically verified lung cancer that had locally progressed and metastasized. The inclusion criteria are patients aged 18 years and older, those with biopsy-proven carcinoma of the lung (both Non-Small Cell Lung Cancer and Small Cell Lung Cancer included), lung cancer that has spread locally and metastasized (Stages III–IV), patients with baseline complete blood count parameters, and those with available data on clinical outcomes and demographics.
Patients with Stage I – II lung cancer, those lacking baseline hematological parameters or information on demographic characteristics and clinical outcomes, and individuals aged less than 18 years were excluded from the study.
Data collection
Demographic data, such as age, gender, occupation, travel time to the hospital, Eastern Co-operative Oncology Group (ECOG) performance status, and clinicopathological data, such as Neutrophil count, Leukocyte count, Haemoglobin value, Platelet count, Red blood cell distribution width (RDW), Haematocrit, and Lymphocyte count were collected. Other clinical parameters like pathological diagnosis, tumor histology, tumor stage, course of stage, date of last visit, and date of the patient’s leave were extracted from patient files, charts, and medical records.
Study procedure
Hematology analysis
The fluorescence and impedance methods for WBC and sub-parameters measurement were done by the Sysmex XS-800i (5-part differential hematology analyzer).
NLR analysis
NLR was derived from absolute counts of neutrophils and lymphocytes. An NLR greater than 3 was considered a prospective prognostic indicator. Subsequently, the NLR values were dichotomized into two distinct groups: those with an NLR of 3 or less and those with an NLR exceeding 3. Survival outcomes were systematically analyzed and compared between these delineated groups.
Table 1
Outcome analysis of patients
Statistical analysis
Statistical analysis was performed utilizing SPSS® for Windows®, version 18.0, developed by SPSS Inc., Chicago, IL. Descriptive statistics, including percentages, means, standard deviations, ranges, and median values with quartiles, were employed to characterize the dataset. The presentation of data involved frequency distribution and percentages. Group comparisons were executed using Chi-squared statistics or Fisher’s exact test, as appropriate.
The Cox proportional hazards model was employed to evaluate variables that independently predicted survival outcomes. Statistical significance was defined as a two-tailed p-value of less than 0.05. Kaplan–Meier survival curves were generated to depict survival trends, with the log-rank test employed for inter-group comparisons. Survival status was determined based on each patient's registration date at the Dr. Bhubaneswar Borooah Cancer Institute.
Results
A total of 546 patients diagnosed with locally advanced and metastatic lung cancer were enrolled in the hospital-based cancer registry at Dr. B Borooah Cancer Institute. Notably, comprehensive records for 262 patients are currently unavailable. Of the remaining 282 patients, information regarding baseline CBC was not available for 57 patients, while 25 patients were misclassified as lung cancer. A total of 202 patients were included in the final analysis. [Figure 2]
Patient characteristics
The median age at the time of presentation for the cohort was 60 years. Among the 202 patients, 156 (77%) were male, establishing a male-to-female ratio of 3.3:1, with 46 (23%) being female. The median travel distance to the hospital was 145 kilometers, ranging from 10 to 700 kilometers. A predominant occupational category among the patients was agriculture, accounting for 45% of the cohort. Notably, more than half of the patients exhibited a performance status of ECOG 1, and approximately 75% had a history of smoking. [Table 2]
Disease characteristics
The prevalent clinical manifestation observed in 59% of patients was NSCLC. Within the NSCLC subtype, adenocarcinoma emerged as the predominant histological variant in 122 patients (60%), followed by squamous cell carcinoma in 59 patients (29%). Non-small cell carcinoma constituted 94% of the histological types observed. The majority of cases presented at an advanced stage, with over 90% classified as TNM stage IV (93%), while 7% were at stage III.
Mutation analysis was conducted in a subset of patients (22%, n=45) using Reverse Transcriptase–Polymerase Chain Reaction (RT-PCR) for EGFR and Immunohistochemistry (IHC) for ALK and ROS.
Baseline CBC parameters
The median total leukocyte count (TLC) count was 9475/mm3, the absolute neutrophil count (ANC) was 6800/mm3, the absolute lymphocyte count (ALC) was 1360/mm3, the platelet count (PLT) count was 259,000/mm3 and the RDW was 15.10%. The median haemoglobin (Hb) and hematocrit (HcT) values were 11.2gm/dL and 31.8% respectively. The median baseline NLR for the 202 patients was 4.6. [Table 3]
Table 3
Baseline CBC parameters
Treatment characteristics
Among the 202 patients, 13 individuals underwent treatment with curative intent, while 189 received palliative interventions. Notably, 47% (95 patients) did not initiate any form of treatment, primarily due to poor performance status or loss to follow-up before treatment initiation.
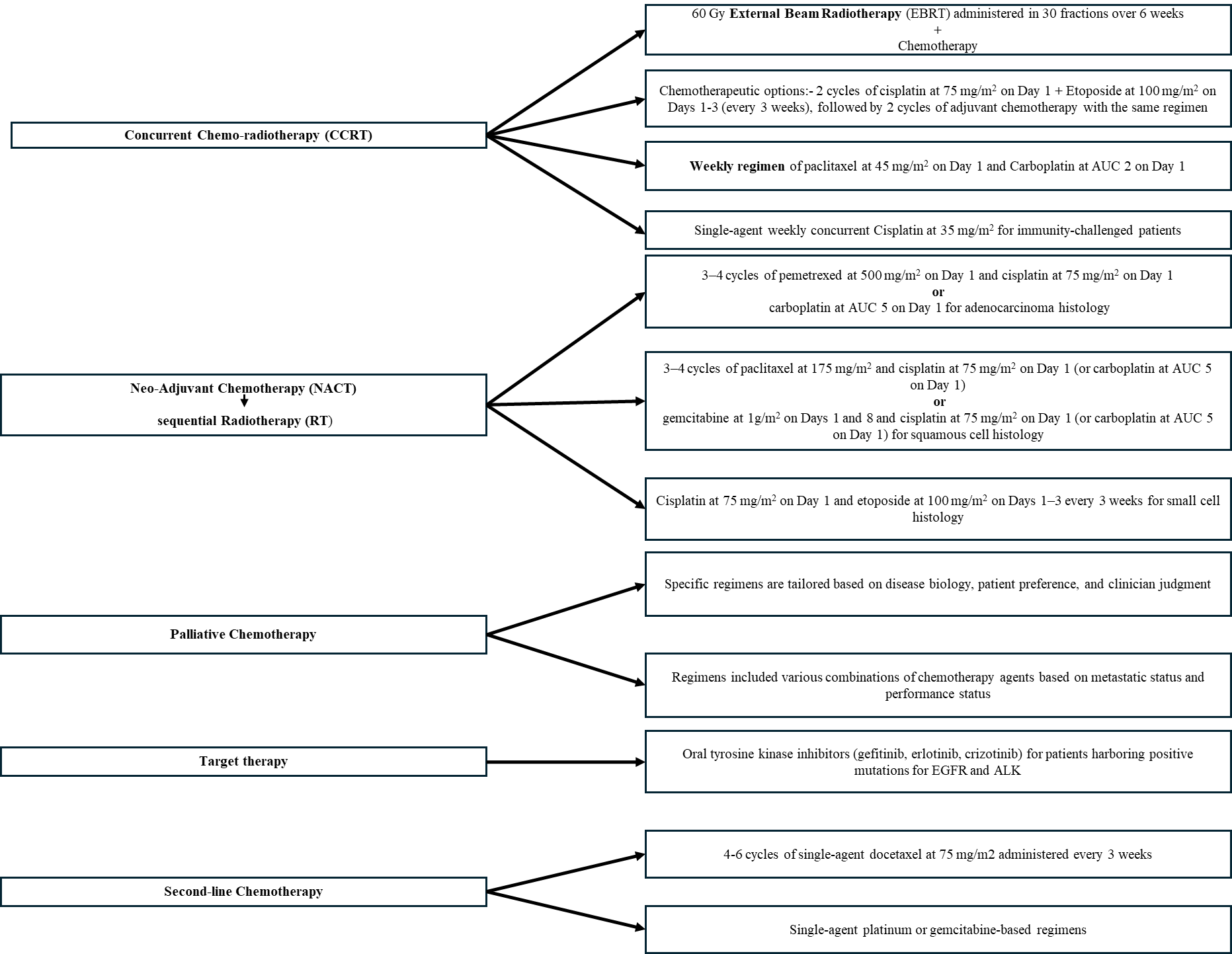
Of the remaining 107 patients, treatment modalities included concurrent chemo-radiotherapy (CCRT) in 4 patients (4%), chemotherapy (CT) alone in 57 patients (53%), radiotherapy (RT) alone (comprising both palliative and radical radiotherapy) in 7 patients (6.5%), CT followed by RT in 7 patients (6.5%), and targeted therapy in 32 patients (30%). Among the subgroup receiving chemotherapy (68/107), the predominant regimen involved platinum and taxane-based treatments in 24 patients (35%), followed by platinum and pemetrexed in 22 patients (32%). Seven patients received maintenance systemic therapy.
Response and survival parameters
For response and survival analyses, a cohort of 107 patients who underwent various forms of treatment was included. Among them, 71 patients (66%) exhibited a positive response to the initial therapy, characterized by partial response in 32% and stable disease in 34%. The median follow-up duration was 6 months (range: 0-37). The median PFS and OS were determined to be 8 months and 10 months, respectively. Notably, progressive disease was observed in 73 patients (68%) during subsequent follow-ups. As of the data analysis cutoff, 3 patients (2.8%) were still alive, 52 patients (48.6%) had succumbed to the disease, and an additional 52 patients (48.6%) were lost to follow-up.
Patients were stratified based on their NLR values into two distinct groups: those with NLR ≤ 3 and those with NLR > 3. In the subset of individuals exhibiting NLR values of 3 or less, the median survival duration reached 11 months, exceeding that of counterparts with NLR values exceeding 3, where the median survival was 8 months. It is important to underscore that this disparity did not achieve statistical significance (p=0.180). [Figure 3]
Figure 3
Log Rank showing the difference in median overall survival amongst subgroup with NLR ≤ 3 and NLR >3

The results showed that there was no significant difference in terms of the patient’s age, gender, stage of disease, performance status (ECOG) and weight loss between 2 groups of NLR >3 and low NLR ≤3. However, NLR > 3 was seen more in patients with NSCLC, than in patients with SCLC (p=0.024), and, in patients with history of smoking versus those without history of smoking (p=0.045). [Table 4]
Table 4
The associations between NLR and clinical features
Upon conducting a multivariate Cox regression analysis, clinical factors including age, gender, stage, histology, performance status, patient weight, and NLR were found to lack independent predictive significance for prolonged survival.
Discussion
Lung cancer stands prominently as a major contributor to cancer-related mortality, impacting both developed and developing nations.29 Despite notable advancements in diagnostic methodologies, molecular profiling, and therapeutic interventions, the overall prognosis for lung cancer patients remains suboptimal. 2 The patient’s demographic was characterized by a predominance of elderly males, with a median age of 60 years, and a noteworthy association with smoking history evident in three-quarters of cases. Nearly 60% of patients presented with a history of weight loss and exhibited a performance status of ECOG PS 1. Histologically, non-small cell (94%) predominated, with adenocarcinoma emerging as the predominant subtype, accounting for 60% of cases. A significant proportion of patients (90%) presented with advanced TNM stage IV disease. In terms of treatment modalities, 13 patients (6%) underwent interventions with radical intent, while the majority (189 patients, 94%) received palliative treatments. Importantly, 47% (95 out of 202) of patients did not receive any form of treatment, primarily attributed to poor performance status or loss to follow-up before the initiation of treatment. Amongst the patients who received any form of therapy, the majority of them received chemotherapy (53%) with or without maintenance. The taxanes and platinum doublet regimen was the most often utilized, accounting for 35% of cases. The median baseline NLR for the 202 patients was 4.6. In patients with NLR≤3 the median survival time (11 months) was numerically longer than that of patients with NLR>3 (8 months), but the result was not statistically significant (p=0.180). Patients with NSCLC histology and with a history of smoking have significantly high markers of inflammation (NLR > 3). At the time of data analysis, 3 (2.8%) patients were alive, 52 (48.6%) were dead, and 52 (48.6%) were lost to follow-up. About 5 decades ago, Coussens and Werb30 reported that chronic inflammatory response has led to the formation and development of tumors. Inflammatory processes involve a spectrum of immune cells, such as lymphocytes, monocytes, and platelets, alongside various signaling molecules within the cellular immune system. The stream of circulating neutrophil and lymphocyte counts, commonly denoted as the NLR, functions as a discerning marker of systemic inflammation. A comprehensive meta-analysis, consisting of 14 trials and aggregating data from over 2700 lung cancer cases, unveiled a consistent association, wherein an elevated NLR consistently indicated unfavorable OS.
This prognostic significance persisted irrespective of whether Hazard Ratios (HRs) were derived from multivariate or univariate analyses.31 Moreover, neutrophil count elevation has been known as an independent predictor of mortality in individuals diagnosed with lung cancer. 32, 33 The applicability of NLR extends to treatment stratification, facilitating outcome estimation for patients undergoing immunotherapy and guiding alternative therapeutic decisions for those presenting elevated NLR values. 34 Also, increased NLR serves as an independent predictive factor for both the baseline presence and subsequent development of brain metastases in patients with NSCLC, particularly within the subgroup characterized by adenocarcinoma.35 The median cutoff value of NLR reported in various studies ranges from 2.5 to 5. 33, 36, 37, 38, 39 The median NLR in our study was 4.6, but we used a cut-off value of 3 based on the study by Akinei et al., to define the two groups.40 For both NLR values of 4.6 and 3, we did not find any significant difference in median survival, although numerically, there was a 3-month benefit in the low NLR group. This is in contrast to other studies, where they found a significant benefit between two groups (NLR low vs NLR high).40, 31, 41 The possible explanations for this difference could be inadequate sample size and high loss to follow-up rate. A study from Turkey42 that included only stage III patients also showed no difference between NLR ≤ 3.21 vs. NLR >3.21. High NLR in the NSCLC group, as seen in our study, was also shown by a study from Turkey.41 Also, more patients with high NLR were found in patients with a history of smoking, which is expected as smoking is associated with high systemic inflammatory markers. 43 Our study is subject to several limitations that warrant thoughtful consideration. Primarily, it is imperative to acknowledge that this investigation constitutes a retrospective study conducted within a singular institutional setting. The retrospective nature of this study posed inherent limitations, as certain confounding factors, including medical comorbidities, drug usage, or the presence of inflammatory disorders that may impact our outcomes, were beyond the scope of control. Secondly, our study is marked by a notable loss to follow-up rate, and a substantial number of patients were excluded due to missing records. Furthermore, there were disparities in sample sizes across various subgroups, including variations in stage, histology, performance status, and weight loss. Despite these limitations, our study also boasts several strengths. Notably, in the absence of extensive data on lung cancer patients from Northeast India, our investigation contributes valuable database insights. To the best of our knowledge, this study stands as a singular endeavor from Northeastern India. An additional strength lies in our efforts to assess the prognostic relevance of baseline NLR in patients with locally advanced and metastatic lung cancer. Although our study showed that there is no prognostic significance of baseline NLR with overall survival, the numerical difference of 3 months should not be ignored. Thus, it merits prospective studies to evaluate the utility of baseline hematological parameters like NLR, PLR, White Blood Cells, C- C-reactive protein, serum albumin, etc. These are easily available, relatively cheaper, and reproducible blood tests that can be used for prognostication of patients with lung cancer.
Conclusion
Despite observing higher NLR values among smokers and within the non-small cell histology subgroup, the study findings do not substantiate the prognostic significance of pre-treatment NLR for overall survival in patients with metastatic and locally advanced lung cancer. To establish the predictive utility of NLR for overall survival in this patient population, further validation is essential through prospective multicenter studies with larger sample sizes.
List of Abbreviations
NLR- Neutrophil to Lymphocyte Ratio, BBCI- Bhubaneswar Borooah Cancer Institute, NSCLC- Non-Small Cell Lung Carcinoma, SCLC- Small Cell Lung cancer, LDH- Lactate Dehydrogenase, CEA- Carcinoembryonic Antigen, IDM-1- Intercellular Adhesion Molecule- 1, EGFR- Epidermal Growth Factor Receptor, PLR- Platelet to Lymphocyte Ratio, CBC- Complete Blood Count, ECOG- Eastern Cooperative Oncology Group, Hb- Haemoglobin, RDW- Red Blood Cell Distribution Width, HcT- Hematocrit, CCRT- Concurrent Chemo-radiotherapy, NACT- Neo-Aduvant Chemotherapy, HBCR - Hospital Based Cancer Registry, RT PCR- Reverse transcriptase – Polymerase Chain Reaction, IHC- Immunohistochemistry, ANC- Absolute neutrophil count, ALC- Absolute lymphocyte count, PLT - Platelet count, PFS- Progression free survival, OS- Overall survival.