Introduction
We present a case of a 24-year-old female with variable clinical characteristics and multiple underlying anomalies.
Case Presentation
A 24-year-old female presented with a two-month history of intermittent fever, loss of appetite, and generalized weakness. On evaluation, patient had no mental retardation. She had an average built and was afebrile on physical examination, with vital signs within normal limits. No clubbing, cyanosis, or desaturation was noted. The patient's height was 153 cm, weight was 53 kg with body mass index of 22.6 kg/m2.
Chest examination revealed bronchial breath sounds and fine crackles in the left infraclavicular area, with no murmurs on cardiovascular examination, and other systemic examination unremarkable. There was no venous hum or orthodeoxia and jugular venous pulse was not raised. Laboratory tests, including routine blood tests, urine analysis and malaria, dengue, and Widal tests, were unremarkable.
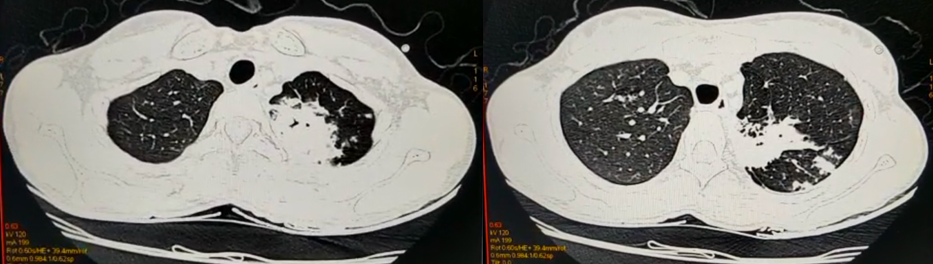
The chest radiograph revealed a cavity in the left upper lobe with surrounding consolidation.. A high-resolution computed tomography (HRCT) scan of the chest was performed to evaluate the pulmonary findings further (Figure 1).
The HRCT scan confirmed the presence of a left upper lobe cavity with surrounding consolidation and micronodular opacities arranged in a tree-in bud (V-Y) pattern with centrilobular distribution in the superior segment of the left lower lobe (Figure 2).
In addition to the pulmonary abnormalities, the HRCT scan incidentally revealed well-defined fat-density lesions in the D4, D6, and D8 vertebral bodies with a thin rim of peripheral sclerosis, suggestive of intraosseous lipomas (Figure 3). Moreover, it identified a partial anomalous pulmonary venous connection (PAPVC), with the right upper lobe pulmonary vein draining into the superior vena cava. Sputum smear for acid -fast bacilli and cartridge- based nucleic acid amplification test (CBNAAT) were negative (Figure 4).
Based on the clinical and radiographic findings, a diagnosis of pulmonary tuberculosis with PAPVC with ASD with intraosseous lipomas was suspected, and the patient was counselled for bronchoscopy with bronchoalveolar lavage to confirm the diagnosis of TB, however, she declined consent for this procedure. In the absence of definitive confirmation, the patient was offered anti-tuberculosis therapy (ATT) with a weight -adjusted fixed-dose combination of isoniazid, rifampicin, pyrazinamide and ethambutol under the National Tuberculosis Elimination Program (NTEP)which was started on May 19, 2023. The patient was also advised 2- dimensional echocardiography which revealed mild pulmonary hypertension of 34 mmHg, following which she was advised by the cardiology department advised the patient to undergo transesophageal echocardiography (TEE) to evaluate the PAPVC further, but she was unwilling to proceed with this procedure; therefore; she was categorized as Group II pulmonary hypertension and initiated on sildenafil citrate tablet 40 mg od.
She has regularly followed up in our outpatient department (OPD), and her symptoms have gradually resolved within 4 weeks.
Discussion
The case presented here describes a 24-year-old female with a two-month history of constitutional symptoms, radiographic findings consistent with tuberculosis, and incidental findings of partial anomalous pulmonary venous connection (PAPVC), ASD and intraosseous lipomas. The patient's clinical presentation, imaging results, and response to anti-tuberculosis therapy (ATT) are consistent with previously published reports on tuberculosis and associated cardiac abnormalities.
Tuberculosis remains a global health concern, and its diverse clinical manifestations often pose diagnostic challenges. Constitutional symptoms such as low-grade fever, generalized weakness, and loss of appetite are common initial presentations observed in this patient. While laboratory tests may initially yield unremarkable results, imaging studies are crucial in confirming the diagnosis.1
Partial anomalous pulmonary venous connection (PAPVC) is an congenital cardiac anomaly where the pulmonary veins connect to superior vena cava on the right side of the heart. This condition can result in excessive blood flow to the lungs and the right side of the heart, ultimately leading to the gradual development of heart failure. 2
PAPVC is a rare congenital heart defect in less than 1% of autopsies. It typically involves an abnormal connection of one or more of the right pulmonary veins to the right side of the heart, either the superior vena cava (SVC), the right atrium (RA), the inferior vena cava (IVC), the innominate (brachiocephalic) vein, or the coronary sinus.3 PAPVC is also frequently associated with other congenital heart defects, mostly atrial septal defects (ASD).4, 5
ASD is a congenital cardiac anomaly in which an opening in the septum separates the left and right atria of the heart which permits blood circulation between both chambers, ultimately leading to heart failure. In patients with the ostium secundum type of ASD, the incidence of PAPVC is approximately 15%, whereas in the sinus venosus type it approaches 90%.5 Pulmonary tuberculosis (TB) is a lung infection caused by Mycobacterium tuberculosis, which causes parenchymal inflammation, destruction and scarring leading to respiratory symptoms. Intraosseous lipomas are benign tumours that originate from the bone marrow. They are uncommon, but are usually found in the long bones of the upper and lower limbs. The combination of PAPVR, ASD, Pulmonary TB, and intraosseous lipomas is a rarely encountered condition that poses a complex diagnostic and treatment dilemma.6
In this case, the chest radiograph revealed a left upper lobe cavity with surrounding consolidation and v-y opacities in the superior segment of the left lower lobe, consistent with pulmonary tuberculosis. Moreover, the HRCT scan incidentally identified intraosseous lipomas in the vertebral bodies, which, to our knowledge, is a rare finding in tuberculosis cases. Although no specific link between tuberculosis and intraosseous lipomas has been established, their coexistence may represent a coincidental finding.1
The presence of a PAPVC in our patient is another interesting aspect of this case. PAPVC is a rare congenital cardiac anomaly characterized by anomalous drainage of pulmonary veins into the systemic venous circulation.7, 8 While its significance concerning tuberculosis is uncertain, PAPVC has been reported as a coincidental finding in several studies on tuberculosis and associated cardiac abnormalities. This could potentially be attributed to increased pulmonary circulation and plethora in PAPVC, which provides the appropriate conditions for TB bacilli to thrive in such patients. Transesophageal echocardiography (TEE) is the gold standard for diagnosing and assessing PAPVC; however, our patient declined the procedure.
Comparing our findings with similar case reports, we note several similarities regarding the clinical presentation and diagnostic approach, such as in a case series by Pendela et al., where they presented four cases. These cases highlight different presentations of anomalous pulmonary venous connections, emphasizing the importance of accurate diagnosis and appropriate management for improved patient outcomes. They demonstrate the varied clinical presentations and imaging findings associated with these conditions. Prompt medical or surgical intervention can improve patient outcomes and symptom relief.6
A case report by Tsang et al., 80 years of age presented with shortness of breath upon exertion. Further evaluation through echocardiography revealed the presence of a secundum atrial septal defect (ASD). Subsequent imaging using contrast-enhanced computed tomography (CT) of the chest confirmed the concurrent occurrence of partial anomalous pulmonary venous return (PAPVR) alongside the atrial septal defect.9 However, the incidental identification of intraosseous lipomas and the patient's reluctance to undergo confirmatory procedures like TEE present unique aspects of this case.
Intraosseous lipomas are describes as rare lipomas seen in long bones; also calcaneum; very few cases are described occurring in vertebral bodies, like in our case. This seems to be a co-incidental finding in this patient of PAPVC and pulmonary TB. One school of thought suggests that intraosseous lipoma caused due to bone marrow infarction and development of regressive lesions due to specific vascularisation in bone. PAPVC may be considered as a pre-disposing factor for infarcts; thalami infarct is described.10
It is worth emphasizing that while our patient's symptoms resolved following ATT and treatment for pulmonary hypertension with sildenafil citrate, the comprehensive evaluation of the PAPVC is crucial for a thorough understanding of its clinical significance and potential impact on long-term outcomes. As the patient continues to follow up in the outpatient department, efforts should be made to counsel and educate her regarding the importance of further cardiac evaluation and potential treatment options.
Conclusion
This case report describes a rare and complex condition involving the combined presence of PAPVC, ASD, TB, and intraosseous lipomas. The history was subacute in presentation with a 2-month duration of intermittent fever, loss of appetite, and generalized weakness as the clinical features. The chest radiograph and HRCT scan findings were consistent with tuberculosis and PAPVC. The patient was started on isoniazid, rifampicin, pyrazinamide and ethambutol for TB and sildenafil citrate for PH, which subsequently led to clinical improvement. The combination of these different conditions at a single time-point can be challenging to diagnose and manage effectively. Furthermore it becomes difficult to provide a good standard of care to such patients, taking into consideration the myriad presentation of different disorders involving different organ systems (lung, bone, heart and vasculature). However, early diagnosis and treatment are important to prevent complications such as progression of infection and to heart failure. This particular case report highlights the importance of a multidisciplinary approach in management of these complex conditions. Efforts to raise awareness about tuberculosis, early diagnosis, and appropriate management are crucial to achieve better outcomes. Furthermore, this case emphasizes the need for thorough diagnostic evaluation and patient education regarding tuberculosis, pulmonary vascular malformation and cardiac failure to ensure comprehensive care in such a complex clinical scenario.