Introduction
Head and Neck lesions often seen in clinical practice have great implications due to the complex anatomy of the head and neck region; sometimes, these lesions may be painless. These lesions aetiology may be infectious, benign or malignant tumours. The demographic changes and location of the lesions provide information regarding the type, etiopathogenesis and prognosis. Rigorous clinical examination accompanied by radiological, Fine needle Aspiration Cytology and excision biopsy is required to achieve firm evidence regarding the type of origin of these conditions. We share our experience with these rare and interesting cases presenting to our Otorhinolaryngology and Head & Neck surgery department at our institute in 2022. This article is unique because of these lesions rare aetiology, multidisciplinarity, and transdisciplinarity approaches.
More than one speciality workup is required to resolve these unique cases. However, it requires a multidisciplinary perspective, combining several skills in diagnosing and treating a patient. These interesting pathology and patient presentations need a transdisciplinary solution that includes additive skills contributed by different specialists. We recommend that the multidisciplinary teams undergo training over time to see these patients through the eyes of a colleague from another speciality for appropriate surgical outcomes, disease staging and chemotherapy regime.
Case 1
Castleman disease
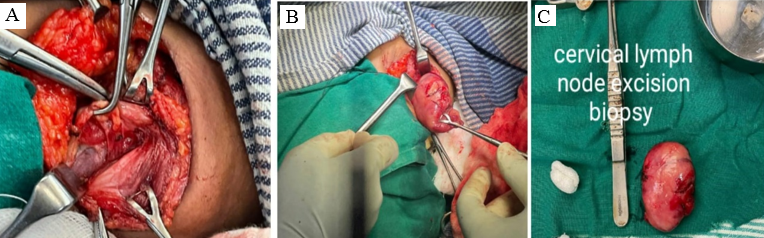
The patient is a 25-year-old lady who presented with swelling on the right side of the neck for 5 yrs. Insidious in onset and gradually progressed to size 5*4 cm with no other significant history.
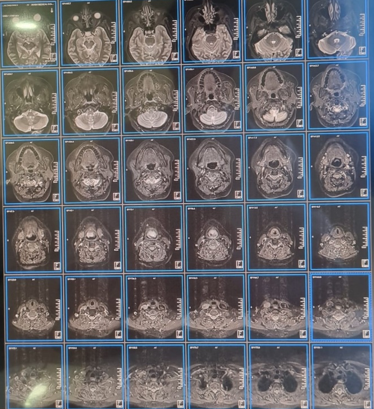
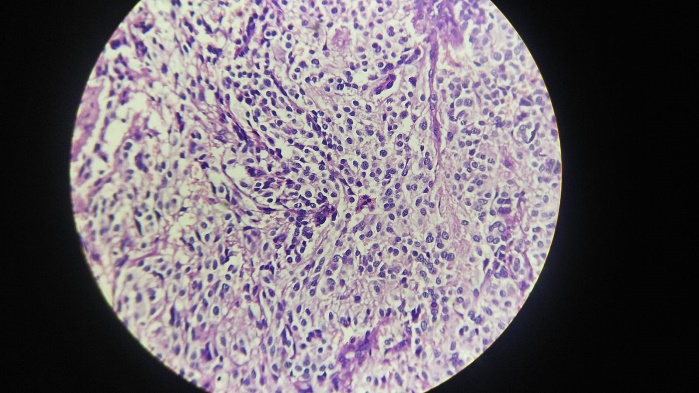
A horizontally oval swelling measuring 5*4 cm at cervical lymph node level II/III on the right side of the neck. Smooth margins and surface, firm in consistency and freely mobile on all sides. No carotid pulsations were felt. No carotid bruit heard. FNAC(09-08-2017) of the Right cervical lymph node showed features suggestive of reactive lymphadenitis. MRI neck (Plain and Contrast)(20-07-2022) showed a large, well-defined, uniformly enhancing lesion at level II/III on the right side surrounded by sub-centimetric lymph nodes. FNAC(20-07-2022)- Reactive lymph node with extensive necrotic background. USG neck and thyroid- Bilateral cervical lymphadenopathy with maintained fatty hilum, likely benign, to rule out Koch’s aetiology. The only significant haematological finding was significant raise in ESR of 45mm at the end of one hour. The diagnosis of the Tubercular cervical lymph node was made. The patient was advised to undergo an excisional level II/III biopsy.
The excised specimen was sent for various analyses. AFB/ZN staining was negative. The aerobic culture showed no growth of microorganisms. The CBNAAT study was negative. The diagnosis was Castleman disease in the histopathological study. It was a hyaline vascular variant and was suggested by IHC for confirmation. The patient was then referred to Immunologist for further management and to rule out any possibility of Pemphigus.
Case 2
Non-hodgkins lymphoma
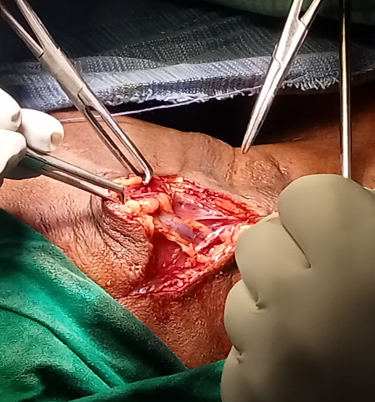
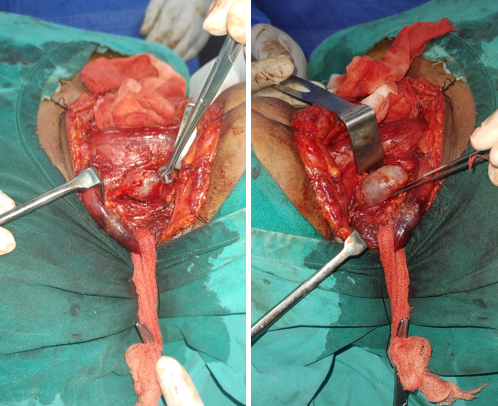
A male patient aged 70, with history of diabetes, presented a gradually progressing mass on the right side of the neck over 10 days. The mass is soft, painful, fluctuant with smooth borders, and approximately 7 x 5 cm. The transillumination test was negative. There was no erythema, ulceration or any venous prominence on the surface of the swelling. Diagnostic nasal endoscopy and Fibreoptic laryngoscopy revealed no abnormality. Ultrasound neck showed a Suppurative lymph node in the right level II. Irregular multiloculated anechoic collection in the right paramedial neck may be an abscess. The patient underwent an incision and drainage of the neck abscess (Figure 4). Culture of the pus showed Klebsiella species and sensitivity to Cefaperazone/Sulbactum, Gentamicin and Imipenem. Treated accordingly with Cefaperazone/Sulbactum for 7 days.
After about 2 months, the patient presented with swelling at the exact site, about 4*3 cm, and an enlarged lymph node on the left side, about 2*1 cm. Both the swelling was firm in consistency. The fibreoptic laryngoscopic examination also showed a cystic lesion in the left tonsil and adjacent tongue base.
CECT neck done. Abnormal enhancing irregularly shaped lesion involving the left oropharyngeal wall and advised to exclude malignancy.
Bilateral tonsillectomy and right selective neck dissection (II/III) under GA was done without injuring the underlying structures (Figure 5). Post-operative recovery was uneventful, without any complications.
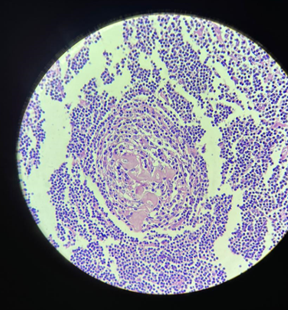
Figure 5
40X(high power) Photomicrograph exhibiting large- to Atypical medium-sized lymphocytes with nuclear atypia.
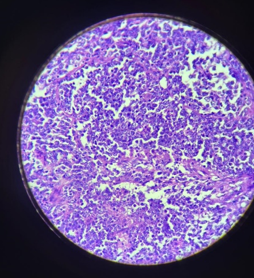
And the diagnosis was unusually rare, which showed on the histologic picture as Non-Hodgkin’s lymphoma. It was advised to confirm on IHC. Later IHC raised the possibility of 1. Burkitt’s lymphoma 2. Diffuse large B-cell lymphoma, GC type. Patient was referred to Medical oncologist for treatment.
Case 3
Epiglottic paraganglioma
A 46-year-old female patient complained of a voice change for 2 years and difficulty swallowing for 6 months. The Flexible Fibreoptic Laryngoscopic picture revealed a globular swelling on the laryngeal surface of the epiglottis (Figure 7). Additionally, MRI of the neck (Plain) showed a sizable lesion in the Supraglottis originating from the laryngeal surface of the epiglottis, which compressed the laryngeal airway. Furthermore, there was no cervical lymphadenopathy detected. (Figure 8).
Figure 6
Flexible fibreoptic laryngoscopic picture showing a globular mass in the laryngeal surface of the Epiglottis

The patient underwent Microlaryngoscopy and coblation-assisted excision biopsy of the epiglottis mass and was sent for Histopathological examination, which showed features suggestive of Paraganglioma (Figure 10). Immunohistochemistry confirmed the diagnosis.
The patient underwent Transoral Laser (CO2 laser free beam) Assisted Supraglottic Laryngectomy. Lindholm direct laryngoscope and Laryngeal ligaclips were used to clip the vascular pedicle in the pharyngoepiglottic fold. Postoperative findings were uneventful, and patient was advised to follow up regularly.
Case 4
Leprosy of larynx
A 48-year-old man who had experienced progressive hoarseness, dysphonia and difficulty in breathing for a year sought consultation. The patient had a leonine appearance, a saddle-shaped nose, madarosis, accentuated skin folds, and hyperpigmented nodules on his extremities and trunk accompanied by paresthesia. Nodules and ulcerations were noted on both ears. (Figure 11, Figure 12)
The greater auricular, ulnar, and common peroneal nerves were enlarged and during the monofilament test, demonstrating decreased sensation throughout the digits. The results of the motor test, laboratory tests, and chest X-ray were unremarkable. Lepromatous leprosy was diagnosed after a skin biopsy.
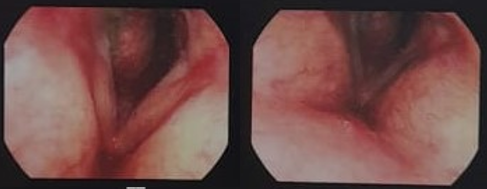
Video Laryngoscopy revealed edematous epiglottis, arytenoid, aryepiglottic folds and false vocal cords with bilateral vocal cord palsy. (Figure 13)
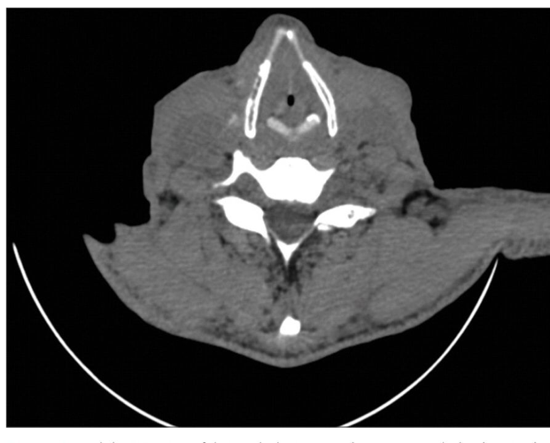
Figure 11
CT scan of the neck revealed thickened epiglottis, arytenoid, false folds, and aryepiglottic folds with 5 mm glottic chink.
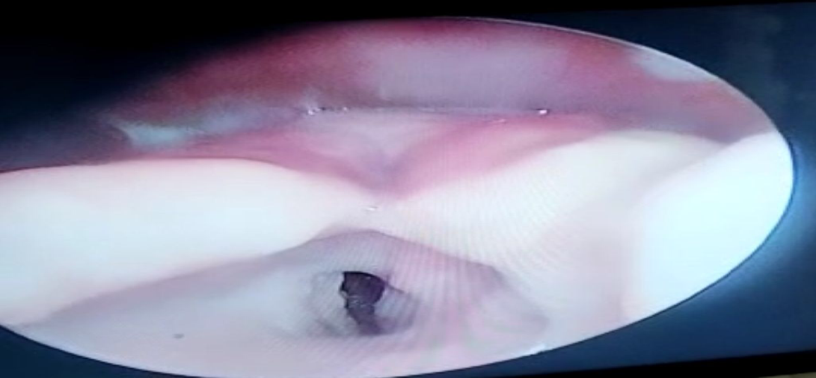
Figure 12
CT scan of the neck revealed thickened epiglottis, arytenoid, false folds, and aryepiglottic folds with 5 mm glottic chink.
Direct laryngoscopy with aryepiglottic mass tissue biopsied. Hematoxylin and eosin (H&E) stain revealed mononuclear cell infiltrates without neutrophils, which is consistent with chronic inflammation, and the stain revealed the presence of acid-fast bacilli on the arytenoid mass. Both observations point to laryngeal leprosy.
The patient was started on a multibacillary regimen containing rifampicin, clofazimine, and dapsone and advised regular follow-up.
Case 5
Subglottic pleomorphic adenoma
A 65-year-old male patient was brought to the emergency ward because of severe dyspnoea and cyanosis. Bystander gave a history of the patient’s breathlessness for 2 months, first in the exertional form and then even during rest with tachypnoea. The patient gave an account of subglottic pleomorphic adenoma undergoing Laser excision 2 years back. The patient was given symptomatic treatment and stabilised. When lying down, his dyspnoea became more severe. He did not complain of dysphagia or weight loss. He was a non-smoker and non-alcoholic, with no history of infectious disease or positive family history.
Figure 13
Flexible fibreoptic laryngoscopic examination showed a large and firm tumour, filling more than 50% of the subglottis site. It was pink with a distinct and marked vascular pattern over its capsule.
The patient underwent Enmasse tumour excision after opening the trachea vertically in the midline. Routine horizontal Kocher’s skin incision and retracting of the strap muscles laterally. The trachea opened vertically in the midline, and the tumour was excised completely and converted to permanent tracheostomy. The mass was sent for histopathological examination. It was Pleomorphic adenoma recurrence indeed.
Follow up after 3 months; patient doing well on permanent tracheostomy and flexible fibreoptic laryngoscopic examination through the stoma showed no signs of recurrence.
Discussion
Case 1- Castleman disease
Castleman disease is named after Benjamin Castleman, who described the condition in 1956. The Castleman Disease Collaborative Network is the largest organisation dedicated to accelerating research and treatment for Castleman Disease and improving patient care. 1
Castleman disease (CD) is an infrequent nonclonal lymphoproliferative disorder that presents unique subtypes among Indian patients. The subtypes of CD vary based on their aetiology, pathology, and clinical presentation. This condition can manifest in any body’s lymph node region, mimicking benign and malignant abnormalities in the neck, chest, abdomen, and pelvis. The CD has several pathological classifications, including hyaline vascular type (HV-CD), plasma cell type, mixed type, and human herpesvirus (HHV)-8 associated Castleman disease. 2
Unicentric (or unifocal) Castleman disease (UCD) is the most common clinical manifestation, whereas multicentric (or generalised) Castleman disease (MCD) is uncommon (MCD).
The reason may be the lymphoid organs excessive production of B lymphocytes and plasma cells. 3, 4
Our example, a 25-year-old female, stands in sharp contrast to the 61% of male patients with MCD and the 53-year-old mean age seen in a comparable US study.4 Its frequency among certain ethnic or sexual groups is unreported. Our patient, who is 25 years old, is on the younger end of the spectrum for the beginning of Castleman disease; nevertheless, the age at which symptoms occur might vary. The hyaline-vascular type accounts for 91% of cases, whereas the plasma-cell form accounts for just 9%. 5
Due to the expanded lymphoid follicles, broad mantle zone, and hypoplastic germinal centre, the hyaline vascular type appears as "onion skin." These follicles are perforated by hyalinised capillaries resembling "lollipops" (the lollipop sign). Interfollicular zones are characterised by significant endothelial vascular proliferation and hyalinisation. 6
Castleman disease could be challenging to identify since it shares no symptoms with other lymphadenopathy-causing diseases. When both major criteria, at least two secondary criteria and one laboratory test abnormality, are fulfilled, a diagnosis may often be made. Principal criteria include the appearance of enlarged lymph nodes and a histopathological examination of the nodes to assess the presence or absence of unicentric or multicentric disease features. Secondary criteria include symptoms of clinical B cells analogous to lymphomas, such as anaemia, thrombocytopenia or thrombocytosis, hypoalbuminemia, and elevated CRP or ESR. The most successful treatment for unicentric lesions of Castleman disease is thorough surgical excision. Similarly, it was given to the patient. 7
Non-Hodgkin’s Lymphoma presenting as cervical lymph node abscess
Non-Hodgkin lymphoma (NHL) is an umbrella term for lymphoproliferative tumours. NHLs are far less foreseeable and have a higher propensity to spread to extranodal regions than Hodgkin's lymphomas. NHL is a prevalent type of haematological malignancy known as NHL. The infiltration of atypical lymphocytes, such as small to medium-sized lymphocytes with copious cytoplasm, plasma cells, and monocytoid B-cells, is a hallmark feature of NHL. 8 Age-adjusted incidence rates for non-small cell lung cancer in India are 2.9 cases per 100,000 men and 1.5 cases per 100,000 women. 9
NHL primarily involves lymph nodes, with their enlargement generally being the first sign of disease leading to a diagnosis. 10 Occasionally, NHL may affect extranodal lymph nodes, including the spleen, brain, nose, paranasal sinuses, lungs, intestines, liver, and testes. 11 But in contrast to our study, where the patient presented with Lymph node abscess as the first symptom and developed into NHL after 2 months, it is not seen as and very rare occurrence. Follicular lymphoma, Burkitt lymphoma, diffuse large B cell lymphoma, Mantle cell lymphoma, marginal zone lymphoma, and primary CNS lymphoma are the most prominent adult B cell neoplasms. Adult T-cell lymphoma and mycosis fungoides are the most frequent of mature T-cell lymphomas. 12 Even in our situation, the pathologist recommended ruling out the likelihood of these common types.
A lymph node biopsy should be considered if significant enlargement persists for more than four to six weeks, progressive increase in growth. Excisional lymph node biopsy is regarded as the gold standard diagnostic method, but fine needle aspiration is not recommended. Excisional biopsies of intact lymph nodes give adequate samples for hematopathologists to undertake histological, immunological, and molecular biology examinations and specimen classification. 13
Case 3- Epiglottic Paragangliomas
Paragangliomas are rare neuroendocrine tumours that arise in the extra-adrenal paraganglia of the autonomic nervous system. When these tumours are identified in the head and neck, the carotid body, the jugular body, the glossopharyngeal nerve, the tympanic branch, and the vagus nerve are usually situated nearby. They account for less than 0.6% of all head and neck tumours, and there have been less than 130 recorded cases since they were originally characterised in 1955.14, 15 Laryngeal paragangliomas seem uncommon and, according to a 3:1 female-to-male ratio, are three times more likely to affect women than men. Individuals about 44 years old, like the patient mentioned in this article. Depending on their location and size, laryngeal paragangliomas may cause various symptoms. These symptoms include breathlessness, dysphagia, hoarseness, stridor, or the feeling of a foreign body in the airway. The patient, in this case, exhibited hoarseness but had no signs of dyspnoea or stridor. The larynx contains two pairs of paraganglia divided into superior and inferior groups. The physiological role of laryngeal paraganglia is unknown. They may serve as extracarotid chemoreceptors or have some effect on respiration via the larynx. 16
The vast majority (82%) occur in the supraglottic larynx; only 15% occur in the subglottis and 3% in the glottis. The right side of the larynx is more often involved than the left by a ratio of 2.3:1. 17, 18 Microscopically, laryngeal paragangliomas have the same appearance as paragangliomas of other sites. The tumour is highly vascular and comprises two types of cells: chief cells and sustentacular cells, arranged in a characteristic alveolar or Zellballen pattern. 16
Immunohistochemistry helps establish the correct diagnosis as the distinction between paraganglioma, and atypical carcinoid/neuroendocrine carcinoma may prove difficult on light microscopy. 19 In the present case, only a provisional diagnosis of paraganglioma could be made on histopathologic examination. However, with the help of immunohistochemistry (Chromogranin positive and Cytokeratin negative), a definitive diagnosis of paraganglioma was possible before surgical excision was performed.
Paragangliomas are generally benign tumours. While vascular, capsular, or perineural invasion may suggest aggressive behaviour, it is not a definitive indicator. A paraganglioma is only classified as malignant if metastasis is evident, and the absence of metastasis indicates a benign tumour. Nevertheless, the patient is closely monitored for any signs of recurrence or metastasis. 20
Case 4- Leprosy of the larynx
Leprosy (Hansen’s disease) is a chronic infectious disease caused by M. Leprae. It mainly affects peripheral nerves. It can also affect the skin, muscles, eyes, bones, testes and internal organs, but affecting the larynx is very rare.
According to WHO, the prevalence rate of the disease has dropped from 21.1 cases per 10,000 population in 1985 to 0.25 per 10,000 in 2017, explained by an improvement in the management of patients. 21
Like TB, laryngeal involvement in leprosy occurs only when there is a concurrent systemic disease. Invariably there will be cutaneous lesions which may have been present for several years, with the nasal cavity frequently being affected. The supraglottic is often involved in the larynx, mainly epiglottis with features of oedema, nodules and ulceration. The dysphonia is of muffled voice quality. The diagnosis is achieved by biopsy of this area with isolation of Mycobacterium leprae from the tissues.
On these lesions, anti-leprosy treatment is similarly effective. Such cases should frequently undergo a screening survey for laryngeal pathology.
The number of cases of laryngeal leprosy significantly decreased due to the development of multidrug therapy. 22
In a case series of 29 individuals with lepromatous leprosy done in 1974 by Barton, 31% of the patients showed laryngeal involvement. A case study of 10 lepromatous leprosy patients with laryngeal involvement was done in 1983 by Gupta et al. Their study's striking physical examination result was that the epiglottis was swollen in every patient. 23
The epiglottis is preferred by Mycobacterium leprae over other laryngeal locations because it is 2 °C cooler than the rest of the body. Aryepiglottic folds, arytenoids, the posterior commissure, and false vocal folds are also affected by the condition if untreated. The primary pathophysiologic mechanism, collective tissue fibrosis, subsequently causes airway impairment, vocal fold immobility, laryngeal stenosis, and may even require tracheostomy. 24
Leprosy of the larynx may be seen in fibrotic and ulcerative forms. In the fibrotic form, the larynx tissue reacts to Mycobacterium leprae by forming fibrous tissue, resulting in the immobility of the vocal cords, giving rise to hoarseness. The disease is slowly progressive and may lead to complete stenosis of the larynx, as seen in our patient, and sometimes a tracheostomy may be required to save the patient's life. 25
The primary course of treatment for multibacillary leprosy is dapsone, clofazimine, and rifampicin, according to the WHO. After two months of dapsone treatment, nasal discharge bacterial counts have reportedly decreased to almost nothing. 22
Case 5- Subglottic pleomorphic adenoma
Pleomorphic adenoma (PA) is the most common type of salivary gland tumour, accounting for 60% of all neoplasms.26 PA typically arises in the parotid gland (80% of cases), submandibular gland (10%), or minor salivary glands in the oral cavity, paranasal sinuses, and upper respiratory and alimentary tract (10%).27 Although usually slow-growing and painless, PAs can be mistaken for malignant neoplasms, especially in unusual sites like the larynx. Therefore, histopathological confirmation is necessary to distinguish PA from other tumours. A mixture of epithelial tissue and myxoid, mucoid, or chondroid appearance tissues characterises PAs.28 Occasionally, PAs can be composed almost entirely of epithelial cells, leading to misdiagnosis as carcinoma. When located in the larynx, early diagnosis is crucial since PAs can cause stridor and respiratory compromise. Complete surgical excision is the treatment of choice, but the recurrence can occur years later, and malignant transformation is possible. As a result, long-term follow-up is necessary.
Conclusion
Head and neck lesions are the primary reasons for patients to seek ENT advice. These lesions can be caused by infections, benign, malignant, or even metastatic conditions. When assessing patients, it is essential to consider common conditions and rare differentials to provide complete management for long-term disease-free survival without recurrence.
Common presenting symptoms include hoarseness of voice, ear and throat pain, dysphagia, and neck masses, which often persist for years. A detailed clinical examination and appropriate investigations are necessary for proper diagnosis. Excision biopsy, histopathological examination, and immunohistochemistry studies should be the gold standard protocol for diagnosing head and neck lesions.
A multidisciplinary approach involving pathologists, radiologists, and immunologists is favoured to arrive at a diagnosis for rare cases. The transdisciplinary approach considers mental and social factors, in addition to the symptoms of the illness, to provide holistic treatment for patients.
Abbreviations
AFB- Acid Fast Bacilli; ZN stain- Ziehl-Neelson stain; CBNAAT- Cartridge Based Nucleic Acid Amplification Test; CECT- Contrast Enhanced Computed Tomography; GA- General Anaesthesia; IHC- Immunohistochemistry; MRI- Magnetic Resonance Imaging; CRP- C-reactive Protein; ESR- Erythrocyte Sedimentation Rate.