Introduction
The skin can be affected by calcinosis cutis, an uncommon, benign disorder that is often asymptomatic.1 It is marked histologically by calcium accumulation inside the dermis and clinically by many, tiny, nodular, hard, and painless swelling of varied sizes.2 It might be idiopathic, metastatic, dystrophic, or iatrogenic in nature. 1 There are several ideas that attempt to explain the pathophysiology, but the main argument is on whether the condition is dystrophic or idiopathic.3 In the absence of metabolic diseases, idiopathic calcinosis cutis is a cutaneous calcification of unclear cause.4 The literature has only few case series with this entity.5
Aims and Objectives
The aim of the case series is to present idiopathic cutaneous calcinosis is an uncommon condition that may be properly identified using clinical, pathological, and metabolic correlation.
Materials and Methods
This descriptive study was carried out between January 2019 and December 2021 in the Department of Pathology at VIMSAR, Burla, Sambalpur. All of the information was gathered from the histology and FNA records.
Case History
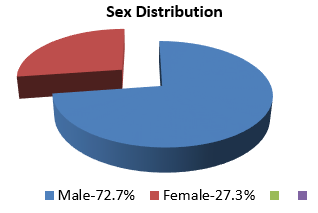
We include 11 cases of cutis calcinosis. Most of the cases, i.e.8 cases (72.7 %) were male, whereas only 3 (27.3%) female cases were found in the present study.(Figure 1)
The age ranged from 6 to 83years.However, maximum cases were between the ages of 30 and to 60 years.(Table 1)
Almost all the cases were clinically diagnosed as epidermoid or sebaceous cyst.
Most common site in this study (6 cases, 54.54%) was scrotum (Figure 2a) whereas, other sites like scalp, forearm, elbow, shoulder, inguinal are a and flanks were observed in other 5 cases.(Table 2)
Table 1
Age distribution
|
Age group (in Years) |
No. of cases |
|
0 -120 |
2 (18.18%) |
|
21 -140 |
4 (36.36%) |
|
41 -160 |
2 (18.18%) |
|
61 -180 |
2 (18.18%) |
|
>80 |
1 (9.09%) |
Table 2
Distribution based on site
|
Site |
No. of cases |
|
Scrotum |
6 (54.54%) |
|
Scalp |
1 (9.09%) |
|
Right side flank |
1 (9.09%) |
|
Forearm, shoulder |
1 (9.09%) |
|
Inguinal area |
1 (9.09%) |
|
Right side Elbow, hand and flank |
1 (9.09%) |
Figure 2
a: Skin swelling in scrotum, b: Cytology smear showing blue amorphous calcific material and anucleated squames (Diff Quik, X100)

Table 3
Details of all cases
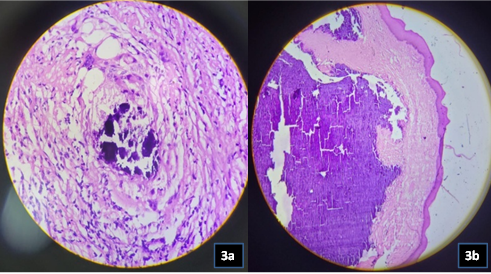
Figure 3
a: Histomorphology showing calcific deposit in centre with gaint cell reaction (H&E, X200); b: Histomorphology showing calcific deposit below stratified squamous lining (H&E, X100)
Lesions were of sizing between 0.5cm to 3cm Except for 2 cases all others were multiple in numbers. FNAC was performed in all the cases. Cytology showed plenty of basophilic amorphous granular deposits in almost all the cases (Figure 2b). There was association of few histiocytes in 4 cases i.e. in case no.2, 5, 6 and 8. Calcium crystals were seen in the background in case no. 3. Giant cell reaction with few anucleated squames were seen in case no.6 and only giant cell reaction in case 9 and 10.(Table 3)
Histopathological correlation could be performed in 7 cases only because the rest of the cases did not turn up for biopsy. Histopathological study showed variable calcium deposition together with foreign body giant cell response and epithelial lining. (Figure 3a&b)
Metabolic work up was normal in all cases except in 1 case which had raised serum urea and creatinine which was excluded from the present study. No instances have, as of yet, documented recurrence.
Discussion
H.M. Lewinsky initially identified idiopathic scrotal calcinosis in 1883. It is a benign, uncommon variant of calcinosis cutis marked by calcium deposition in the form of many hard, nodular swellings over the scrotum. 2
According to aetiology, there are four basic kinds of calcinosis cutis: Metastatic, iatrogenic, idiopathic, and dystrophic. 1, 6 There is another term called calciphylaxis which is associated with metabolic disorder.
It is very important to correctly classify and subtype these lesions, so that the correct treatment can be initiated. Almost in all the cases the Calcinosis cutis lesions gradually grow and have no symptoms. 7 Only point of concern that draws the patient attention is the swelling. Sometimes the lesions get ulcerated and may have chalky white discharge.
A few uncommon variants have been variously categorised as idiopathic or dystrophic.8 These include tumoral calcinosis, calcinosis cutis universalis, calcinosis cutis circumscripta, and transplant-related calcinosis cutis. 8 The CREST syndrome is characterised by calcinosis cutis together with Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia. 9, 10, 11
The aetiology of the calcification affects the history and development of the lesions. Patients with dystrophic calcification may disclose a history of an underlying illness, an earlier dermal nodule (which is a tumour), or an initiating traumatic incident. The majority of individuals with metastatic calcification have a background of chronic renal failure. In contrast to metastatic calcification, serum calcium and phosphate levels are aberrant in dystrophic calcification. Iatrogenic calcinosis cutis patients frequently have a recent hospitalisation history. 12
The present study is a case series of 11 cases, whereas Muddegowda et al (2011) reported 4 cases, 4 Andola et al (2014) reported 9 cases, 13 Alok et al (2017) reported 18 cases,5 out of which 5 cases were idiopathic, Kotian et al (2021) reported 6 cases 1 and few other case reports were reported.
There were 8 male and 3 female cases in the present study whereas in study by Muddegowda et al 4 there were 2 male and 2 female cases. Andola et al 13 reported all 9 cases to be male, whereas Alok et al 5reported 13 male and 5 female cases and Kotian et al 1 had 3 male and 3 female cases in their study. However, it is observed that in all the reported studies there was male preponderance.
As per size of the nodules in the present study size ranges from 0.5cm to 3cm. Similar findings were observed in the studies by Kotian et al,1 Muddegowda et al,4 Andola et al 13 and Alok et al5 where size ranges from 0.3 to 3 cm, 0.4cm to 4cm, 0.5 to 3.5 cm, 0.5 to 4.8cm respectively. In all these studies the lesion were clinically diagnosed as sebaceous cyst which is similar to the present study.
In all these above mentioned studies scrotum was the most common site involved which is at par with the present study. Evidence of epithelial lining was seen in 1 case in the present study. Study made by Muddegowda et al 4 showed evidence of epithelial lining in 1 case and study by Kotian et al 1 observed 3 cases with epithelial lining.
In all these studies serum Calcium, Phosphate, Uric acid, Vitamin D were within normal limits. No history of recurrence were present in studies by Andola et al 13 and Kotian et al. 1
In the differential diagnosis of samples with high levels of calcium on FNAC, it is important to take into account conditions such as calcified fibrous pseudotumor, calcified epidermal cyst, lymphoepithelial lesion, sarcoidosis, tuberculosis, pilomatricoma, osteitis fibrosa cystica, and extraskeletal osteosarcoma.9
A calcified fibrous pseudotumor has an abundance of hyalinized collagen, fat, and neurovascular bundles in addition to calcification.11
Frank granulomatous reaction is seen in Calcified tuberculosis and sarcoidosis, 11 whereas calcified epidermal cyst shows anucleated and nucleated squames.
Presence of basaloid cells and ghost cell along with multinucleated giant cells and calcification are seen in Pilomatricoma which comes as one of the differential diagnosis. 9
Histiocytes, calcification, and a polymorphous population of lymphoid cells are all seen in lymphoepithelial lesions.9 It is possible to rule out extraskeletal osteosarcoma if there are no tumour cells present. The clinical assessment aids in ruling out osteofibrosa cystica.
Reiter et al.'s analysis of several disorders that might cause skin calcification14 and their information on the lab procedures needed to distinguish between different forms of calcinosis cutis were both helpful.
When Shiv Kumar et al.8 examined the cytological characteristics of idiopathic scrotal calcinosis, they found that the smears lacked any signs of epithelial cells and instead had intense, basophilic, amorphous, and granular deposits.
With no prior history of trauma, hospitalisation, parenteral therapy, underlying disease, or any preceding pathological lesion at the site in the current study, along with normal serum calcium and phosphorus levels, dystrophic, iatrogenic and metastatic causes were clearly ruled out, leading to the final diagnosis of idiopathic calcinosis cutis.
Idiopathic calcinosis cutis FNA cytology case reports and case series are uncommon in the literature as of this writing. Correct cytomorphological diagnosis throws a guiding light in determining cases that requires surgical rather than medical treatment.
To conclude, this study is highlighted to alert the pathologists to consider calcinosis cutis as a differential diagnosis in any swelling yielding whitish granular material on FNAC as it is a potential mimic of a neoplastic lesion. It also reaffirms that FNAC is a straightforward, fast, and effective method, especially for soft tissue lesions like calcinosis cutis and in collaboration with serological and biochemical findings can help in effectively triaging the patient for the correct management.