We present an interesting case of an elderly male presenting with pyrexia of unknown origin in whom the imaging findings had a peculiar and characteristic rare appearance simulating a classic pathological diagnosis. On clinical examination patient had hepatomegaly. Biochemical evaluation showed raised bilirubin and alkaline phosphatase (ALP). On ultrasound (USG) imaging the provisional diagnosis was metastasis as evidenced by hepatomegaly with diffuse inhomogeneous echotexture of liver. The lesions were hypoechoic with no posterior acoustic enhancement [Figure 1A]. Computed Tomography (CT) showed hepatomegaly with diffuse heterogeneous attenuation and multiple small hypodense areas. The lesions in arterial and portal phase appeared hypoattenuating with no early contrast enhancement. Delayed contrast enhanced sections of liver showed persistent hypoattenuating nodules. [Figure 1B,C]
Figure 1
USG shows diffuse inhomogeneous echotexture of liver and tiny hypoechoic lesions with no posterior acoustic enhancement [A]: CT shows lesions in arterial and portal phase appeared hypoattenuating with no early contrast enhancement. Delayed contrast enhanced sections of liver showed persistent hypoattenuating nodules; [B,C]: MRI shows multiple ill-defined T2 iso to hyperintense nodules scattered diffusely in both lobes of liver; [D]: The nodules showed significant diffusion restriction; [E] and appeared T1 hypointense; [F]: The MRI appearance in the DWI and ADC sequence was similar to the ‘starry sky pattern’ [G]
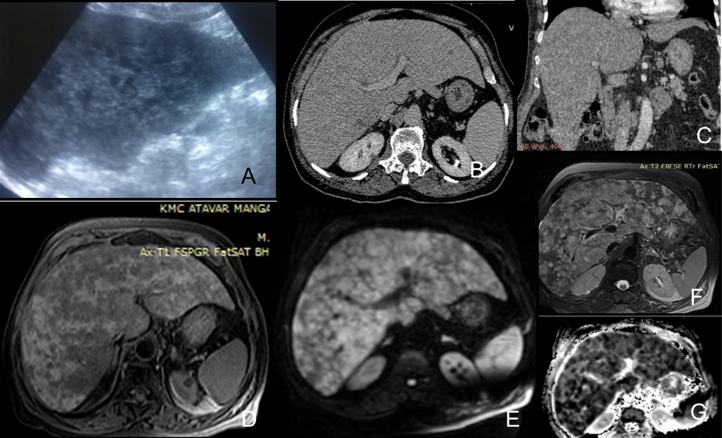
Figure 2
(H&E, 100x)Histopathological evaluation shows the core of liver tissue showing infiltrating sheets of neoplastic cells; (A): (H&E, 200x) Neoplastic cells have moderate amount of cytoplasm, pleomorphic hyperchromatic nuclei with high N/C ratio; (B): (LCA, 100x) Immunohistochemistry (IHC) studies showing neoplastic cells positive for LCA (C). (CD20, 200x) Neoplastic cells positive for CD20 (D).
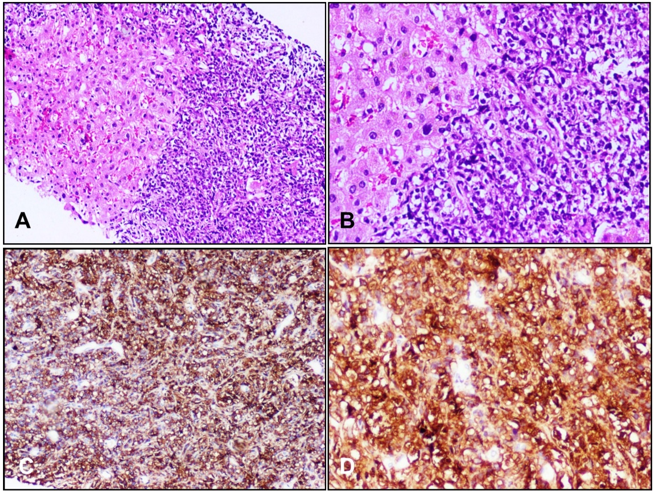
Magnetic Resonance Imaging (MRI) showed diffuse hepatomegaly with multiple ill-defined T2 iso to hyperintense nodules scattered diffusely in both lobes of liver [Figure 1D]. The nodules showed significant diffusion restriction [Figure 1E] and appeared T1 hypointense [Figure 1F]. The MRI appearance in the Diffusion weighted imaging (DWI) and Apparent Diffusion coefficient (ADC) sequence was similar to the ‘starry sky pattern’ [Figure 1G] previously described on USG in acute and chronic hepatitis, right heart failure 1 and lymphoma2 and on MRI in biliary hamartomas.3 Both CT and MRI showed borderline splenomegaly, however no significant intra-abdominal lymphadenopathy. We proceeded with USG guided target biopsy of the liver lesions. On histopathological evaluation the core of liver tissue showed infiltrating sheets of neoplastic cells (Figure 2A). The neoplastic cells had moderate amount of cytoplasm, pleomorphic hyperchromatic nuclei with high N/C ratio (Figure 2B). Based on morphology the differential diagnoses were poorly differentiated carcinoma and lymphoma. On immunohistochemistry (IHC) studies, the neoplastic cells were positive for LCA (lymphoid marker) (Figure 2C), CD20 (B cell marker) (Figure 2D) and BCL-6 (40-50% of cells), confirming the diagnosis of diffuse large B cell Lymphoma. Since there was no evidence of lymph node/ solid organ involvement, the final diagnosis in this case was primary hepatic non-hodgkins B cell lymphoma – diffuse large b cell lymphoma (DLBCL). The patient was followed up on treatment and the lesions regressed with no new development of lymphadenopathy on the 6 months and 1-year follow up.
This is a rare primary presentation of lymphoma accounting for less than 1% of all extranodal lymphomas in general.4 Secondary hepatic involvement with lymphoma is a well-known entity. The classical features described in primary hepatic lymphoma is a large poorly enhancing solitary mass lesion. 5 Few cases show multiple nodules on CT and MRI and often one of the lesions is dominant. There are multiple etiological factors and no definitive association.5 The non enhancing nodules showing diffusion restriction is one clinching point in this case. On DWI and T2 sequences, multiple hyperintense lesions of varying sizes showing diffusion restriction simulate the “Starry sky appearance” pattern. The starry sky pattern has been described earlier in USG of chronic hepatitis liver and in pathological specimens of hepatic lymphoma, however this is the first time it has been extrapolated to DWI of the liver. It is a point of interest!






