Abstract
Introduction: Pulmonary Tuberculosis (PTB) is one of the paramount causes of morbidity and mortality in the developing and underdeveloped countries. India is the country with the highest burden of PTB. Among the electrolyte imbalance hyponatremia is observed commonly which will lead to increase in morbidity and mortality. In this study, the prevalence of hyponatremia in adult pulmonary tuberculosis patients was done.
Methodology: In this retrospective study; patients of age more than 18 years presented to our department from 2016 to 2017 were included. PTB was diagnosed as per the institutional protocol, i.e., on clinical presentation of the patient, microscopic examination suggestive of acid-fast bacilli (AFB) and an abnormal chest radiograph findings. All the case files of patients having PTB in the study period were collected and demographic parameters and relevant laboratory findings were noted and analyzed.
Results: A total of 150 patients with PTB were included in this study between 18 to 86 years of age group. Mean age of patients was 50.92 + 17.76. Among 150 patients, 114 (76%) had hyponatremia with serum sodium levels less than 135mmol/l out of which 84 (74%) were males and 30 (26%) were females. Out of 150 patients 59 (39%) had mild hyponatremia; 41 (27%) had moderate hyponatremia and 14 (9%) had severe hyponatremia. In all the groups of hyponatremia, majority were found to be males. 27 (46%) in mild hyponatremia, 34 (83%) in moderate hyponatremia and 11(79%) in severe hyponatremia were sputum AFB positive. Many patients were asymptomatic except 4 with severe hyponatremia requiring vasopressor support for hypotension.
Conclusions: Patients with PTB should be evaluated for hyponatremia; early detection and treatment of can potentially reduce morbidity and mortality.
Keywords: AFB; Hyponatremia; Mortality; Pulmonary tuberculosis.
Introduction
Pulmonary Tuberculosis (PTB) is one of the paramount causes of morbidity and mortality in the developing and underdeveloped countries. Worldwide TB is one of the top 10 causes of death and the leading cause from a single infectious agent. Globally, 10.0 million people developed TB disease in 2017: 5.8 million men, 3.2 million women and 1.0 million children. As per the previous study 23% of the world’s population, are approximately have a latent TB infection, and are thus at risk of developing active TB disease during their lifetime [1] Tuberculosis is one of the most common infection in India and is associated with high mortality. India ranks 14th out of top 22 countries who are burdened with TB infections [2]. As per the Global TB report 2017 the estimated incidence of TB in India was approximately 28,00,000 accounting major part of the world’s TB cases.
Hyponatremia, defined as serum sodium less than 135 mmol/litre, is the most common electrolyte abnormality in clinical practice [3]. Hyponatremia is important to recognize because of its potential morbidity and also it can be a marker of the underlying disease [4]. Mild, moderate and severe hyponatremia is defined as a biochemical finding of a serum sodium concentration between 130 and 135 mmol/L, between 125 and 129 mmol/L and less than 125 mmol/L respectively. Hyponatremia is observed in 15–20% of emergency patient admissions and it occurs in up to 20% of critically ill patients [5]. The syndrome of inappropriate secretion of antidiuretic hormone (SIADH) is the most common cause of hyponatremia and is characterized by hyponatremia, inappropriately elevated urine osmolality, excessive urine sodium and decreased serum osmolality in a euvolemic patient without edema [6]. SIADH results as a common complication of malignancy, pulmonary disorders, and neurosurgical conditions, cardiac, liver, and renal failure [2]. Besides other infections, PTB has been strongly associated with SIADH [7]. Various mechanism have been postulated as how TB can induce hyponatremia, like local invasion to the adrenal glands, local invasion to hypothalamus or pituitary gland, [8][9][10][11] meningitis [12][13][14] and inappropriate ADH secretion due to pulmonary infection [15][16][17], TB can affect adrenal glands directly. TB may destroy adrenals and leading to overt or subclinical adrenal insufficiency and it is one of the most common cause of Addison’s disease in India [2]. The present study was done to study and analyze the prevalence of hyponatremia in adult patients with PTB in tertiary care in India.
Materials and Methods
It was a retrospective study. The patients presented to medicine department of our tertiary care hospital over a period of one year from 2016 to 2017 with PTB were included. PTB was diagnosed as per the institutional protocol, i.e., on clinical presentation of the patient, microscopic examination suggestive of acid-fast bacilli (AFB) and abnormal chest radiograph findings. Case records of the patients having PTB were collected. Demographic characteristics and laboratory data of the patients were recorded and analyzed. An ethical committee approval was taken.
Inclusion Criteria: Adult patients aged 18 years and above, diagnosed with active PTB.
Exclusion Criteria: Patients with a H/O old TB, kidney disease, malignancies, patients on diuretics and medications related to SIADH. Serum sodium concentration less than 135mmol/L were considered as hyponatremia. Patients were divided into three groups: mild, moderate and severe hyponatremia with serum sodium concentration between 130 and 134 mmol/L, 125 and 129 mmol/L and < 125>
Statistical Analysis
In this study, the statistical methods for quantitative data and descriptive statistics were presented by N, mean, standard deviation and range. For qualitative data, frequency count, N and percentage were tabulated. All the statistical analysis has been done by using statistical software SPSS (version 20) and a p value of < 0>
Results
A total of 150 adult patients with active PTB were included in this study with age ranging from 18 to 86 years. The mean age of patients was 50.92 + 17.76 while the mean age of patients with hyponatremia was 51.42 ± 17.77 and mean age of patients with normal sodium levels were 49.31 ± 17.89 (Table 1). This was statistically not significant (P = 0.53).
Table1: The serum sodium levels and Mean age
|
Serum Sodium (mmol/l) |
Mean age (years) |
|
<135> |
51.42 ± 17.77 |
|
>135 |
49.31 ± 17.89 |
|
P |
0.53 |
The total mean serum sodium levels among the subjects was 130.91 + 4.59.The age distribution and mean serum sodium levels are shown in table 2. As shown in this table 33% of the patients were in the age group of 20-40years and 33% in 40-60years. People in the age group of more than 60 years showed lower mean serum sodium levels (130.35 + 5.19) than that of other groups.
Table 2: Age distribution and mean serum sodium levels
|
Age(years)
|
Patients (%) |
Mean Serum Sodium(mmol/l) |
|
<20> |
4(2.7) |
134 + 1.82 |
|
20-40 |
49(32.7) |
131.38 + 4.49 |
|
40-60 |
49(32.7) |
131.06 + 4.37 |
|
>60 |
48(32) |
130.35 + 5.19 |
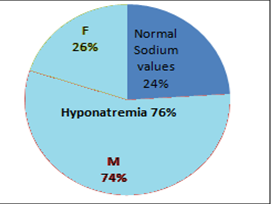
Among 150 patients, 114 (76%) patients had low sodium levels which was less than 135mmol/l out of which 84 (74%) were males and 30 (26%) were females. (Graph 1)
 |
Click here to view |
Fig. 1: Prevalence of hyponatremia
The sex distribution and mean serum sodium levels are represented in table 3, which shows that males had lower levels of mean serum sodium levels (130.84 + 4.57) than females. However this was not statistically significant (p=0.83).
Table 3: Sex distribution and mean serum sodium levels
|
Sex
|
Frequency (%) |
Mean Serum Sodium(mmol/l) |
|
Male |
110(73.3) |
130.84 + 4.57 |
|
Female |
40(26.7) |
131.13 + 4.70 |
|
P |
0.83 |
|
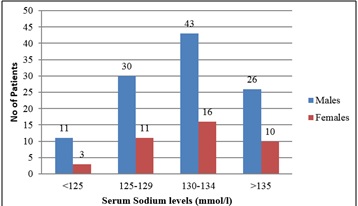
As shown in table 4 most of the patients i.e., 59 (39.3%) patients had mild hyponatremia; 41 (27.3%) had moderate hyponatremia and 14 (9.3%) had severe hyponatremia. In all the groups of hyponatremia, majority were found to be males when compared to the females in their respective groups.
Table 4: Serum sodium levels and gender wise distribution
|
Serum Sodium Levels(mmol/l) |
Males (%) |
Females (%) |
Total (%) |
|
>135 |
26 (72) |
10 (36) |
36 (24) |
|
130-134 |
43 (73) |
16 (27) |
59 (39.33) |
|
125-129 |
30 (73) |
11 (27) |
41 (27.33) |
|
<125> |
11 (79) |
3 (21) |
14 (9.33) |
|
P |
0.88 |
|
|
 |
Click here to view |
Fig. 2: Grading of serum sodium levels and gender distribution
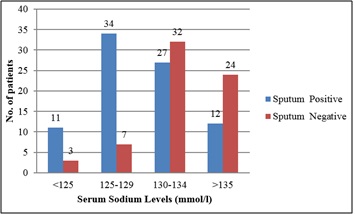
Out of 150 patients, 50 (33.33%) patients were suffering with diabetes and 20 (13.33%) with retroviral disease. Among 50 patients with diabetes and PTB, 38 (76%) had hyponatremia implying that the prevalence of hyponatremia to be more in patients with diabetes, but it was not statistically significant (p=0.88). Among 20 patients with HIV and pulmonary Kochs, 15 (75%) had hyponatremia. This was also not statistically significant (p=0.92) Out of 114 patients with hyponatremia, 72(63%) were sputum AFB positive. This finding is statistically significant (p<0>
Table 5: Serum sodium levels in relation to sputum AFB status
|
Serum Sodium Levels (mmol/l) |
Sputum Positive (%) |
Sputum Negative (%) |
|
>135 |
12(33) |
24(67) |
|
130-134 |
27(46) |
32 (54) |
|
125-129 |
34(83) |
7 (17) |
|
<125> |
11(79) |
3(21) |
|
P |
<0> |
|
 |
Click here to view |
Fig. 3: Serum sodium levels in relation to sputum AFB status
Discussion
A total of 150 patients with PTB were included in this study with an age group of 18 to 86 years and mean age being 50.92 + 17.76 and many were in the age group of 20–60 years. A previous study done showed the mean age of sodium was 44.4 ± 13.81 years ranging from 18 to 80 years [2]. Jafari et al., in their study reported the mean age as 59 ± 20 years in range of 13-102 years [18]and Khan et al., in their study showed the mean age of all the patients to be 51.57 ± 16.3[17].
Our study showed male preponderance i.e., 110(73%) out of 150 were males and 40 (27%) were females. This observation was similar to that of studies done by Bokam et al., with majority 72.2% being males [2]; Khan et al., with 65.6% males [7]; Mukherjee et al., with 69.3% males with a male female ratio of 2.25:1. The higher male prevalence was also found in the Revised National Tuberculosis Programme (RNTCP) [19]. However study by Jafari et al., has shown TB was less in males (45.5%) when compared to females [18]. TB notification rates have been found to be similar in both sexes till puberty, followed by a continuing widening of the gap between male and female cases. In males, the TB prevalence was found to be higher with increase in age. This difference is most marked in the age group beyond 60 years [20].
Out of 150 patients 114 (76%) had hyponatremia i.e., with serum sodium levels <135> [2]. Majority of the patients in our study had mild hyponatremia (39%) and very few with severe hyponatremia (9%). During clinical practice various electrolyte imbalances cases are encountered but among them hyponatremia is the most common with a prevalence up to 15% in a general hospital population. Syndrome of inappropriate anti diuretic hormone secretion (SIADH) is the most commonly encountered form of hyponatremia [21].
The total mean serum sodium levels among the subjects in our study were 130.91 + 4.59. Patients in the age group of more than 60 years had lower mean serum sodium levels than the other age groups. The hyponatremia is more commonly seen in the elderly patients and this is mainly because of degenerate physiology, co-morbid illness and involvement of poly-pharmacy. The elderly patients are highly susceptible to hyponatremia due to poor intake dehydration, inappropriate fluid therapy [21].
The mean serum sodium levels in males in our study was 130.84 + 4.57 and 131.13 + 4.70 in females implying that males had lower sodium levels than that of females. Borkam et al., in their study also showed that mean serum sodium levels were lower in males (132.9 ± 5.8 mmol/L) when compared to females (133.3 ± 5.6 mmol/L) which was similar to our results [2]. Unlike our study Khan et al., observed higher levels of mean serum sodium in males 136.03 ± 6.5 than in females 135.00 ± 6.5 [7].
Most of the patients i.e., 39.33% in our study had mild hyponatremia (serum sodium 130-134mmol/l), 27.33% had moderate hyponatremia (serum sodium 125-129mmol/l) and nearly 9.33% had severe hyponatremia (serum sodium <125>
Out of 114 patients with hyponatremia 72(63%) were sputum AFB positive. This was statistically significant (p<0>[22]. In this study there were no patients with serum sodium values less than 118 mmol/l.
Out of 150 patients, 50 had diabetes as a co-morbidity (33.33%). Among 50 patients with diabetes and pulmonary tuberculosis, 38 (76%) had hyponatremia. This shows prevalence of hyponatremia to be more in patients with diabetes. However this was not statistically significant (p=0.88). There are studies showing that diabetes mellitus is an important risk factor for tuberculosis. Furthermore, tuberculosis might induce glucose intolerance and worsen glycemic control in people with diabetes [23]. Diabetic patients frequently develop a various electrolyte disturbances of which hyponatremia is one. In case of hyperglycemia, there is an increase in movement of water out of the cells and subsequently in a reduction of serum sodium levels by dilution this is mainly because glucose is an osmotically active substance [24].
Out of 150 patients, 20 (13.33%) had retroviral disease. Among 20 patients with HIV and PTB, 15 (75%) had hyponatremia. The previous study have shown that, prevalence of HIV is high in north Karnataka and TB is the most common opportunistic infection among them. Nearly 12 to 20 times the HIV infected people have the risk to develop active TB from the latent form of TB [25].
The limitation of this study was that the cause of hyponatremia was not evaluated further.
Conclusions
Hyponatremia is important to recognize because of its potential morbidity and also it can be a marker of the underlying disease. Hence patients with PTB have to be evaluated for hyponatremia as early detection and treatment of underlying electrolyte abnormality can potentially reduce mortality and morbidity associated with tuberculosis and also can shorten the duration of hospitalization.
Conflicts of Interests: None declared
Acknowledgements: Nil
References
- ^ Global Tuberculosis Report 2018. Available from URL- https://www.who.int/tb/publications/global_report/en. Last accessed 2019 on March 1.
- a, b, c, d, e, f Bokam BR, Badikillaya VU. Prevalence of hyponatremia in pulmonary tuberculosis - A pilot study from a tertiary care center in south India. Int J Med Sci Public Health 2017;6(1):75-79.
- ^ Saeed BO, Beaumont D, Handley GH, Weaver JU. Severe hyponatraemia: Investigation and management in a district general hospital. J Clin Pathol 2002;55(12):893–896.
- ^ Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. Engl J Med 2007;356(20):2064–2072.
- ^ Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D, et al. Clinical practice guideline on diagnosis and treatment of hyponatremia. Intensive Care Med 2014;40:320–331.
- ^ Huda MSB, Boyd A, Skagen K, Wile D, Van Heyningen C, Watson I, et al. Investigation and management of severe hyponatraemia in a hospital setting. Postgrad Med J 2006;82(965):216–219.
- a, b Khan K, Rasool N, Mustafa F, Tariq R. Hyponatremia Due to Pulmonary Tuberculosis in Indian Population. Int J Sci Study 2017;5(5):98–101.
- ^ Jacobi J, Schnellhardt S, Kulschewski A, Amann KU, Kuefner MA, Eckardt KU, et al. An unusual case of hyponatremia. Nephrol Dial Transplant 2010;25(3):998–1001.
- ^ Kinjo T, Higuchi D, Oshiro Y, Nakamatsu Y, Fujita K, Nakamoto A, et al. Addison’s disease due to Tuberculosis that required differentiation from SIADH. J Infect Chemother 2009;15(4):239–242.
- ^ Lam KS, Sham MM, Tam SC, Ng MM, Ma HT. Hypopituitarism after tuberculous meningitis in childhood. Ann Intern Med 1993;118(9):701–706.
- ^ Berger SA, Edberg SC, David G. Infectious disease in the sellaturcica. Rev Infect Dis 1986;8(5):747–755.
- ^ Nagotkar L, Shanbag P, Dasarwar N. Cerebral salt wasting syndrome following neurosurgical intervention in tuberculous meningitis. Indian Pediatr 2008;45(7):598–601.
- ^ Dass R, Nagaraj R, Murlidharan J, Singhi S. hyponatremia and hypovolemic shock with tuberculous meningitis. Indian J Pediatr 2003;70(12):995–997.
- ^ Anderson NE, Somaratne J, Mason DF, Holland D, Thomas MG. Neurological and systemic complications of tuberculous meningitis and its treatment at Auckland City hospital, New Zealand. J Clin Neurosci 2010;17(9):1114–1118.
- ^ Lee P, Ho KK. Hyponatremia in pulmonary TB: evidence of ectopic antidiuretic hormone production. Chest 2010;137(1):207–208.
- ^ Vorherr H, Massry SG, Fallet R, Kaplan l, Kleeman CR. Antidiuretic principle in tuberculous lung tissue of a patient with Pulmonary Tuberculosis and hyponatremia. Ann Intern Med 1970;72(3):383–387.
- a, b Schorn D. Inappropriate antidiuretic hormone secretion. Two cases presenting with Pulmonary Tuberculosis. S Afr Med J 1974;48(27):1161–1162.
- a, b Jonaidi Jafari N, Izadi M, Sarrafzadeh F, Heidari A, Ranjbar R, Saburi A. Hyponatremia Due to Pulmonary Tuberculosis: Review of 200 Cases. Nephrourol Mon 2012;5(1):687–691.
- ^ Directorate General of Health Services. Ministry of Health and Family Welfare. New Delhi, India. Revised National Tuberculosis Control Programme.Technical Guidelines for Tuberculosis Control, 2005.
- ^ Mukherjee A, Sarkar A, Saha I, Chowdhury R. Gender differences in notification rates, clinical forms and treatment outcome of tuberculosis patients under the RNTCP. Lung India 2012;29(2):120-122.
- a, b Mukherjee A, Sarkar A, Saha I, Chowdhury R. Gender differences in notification rates, clinical forms and treatment outcome of tuberculosis patients under the RNTCP. Lung India 2012;29(2):120-122.
- ^ Biswas M, Davies JS. Hyponatraemia in clinical practice. Postgrad Med J 2007;83(980):373–378.
- ^ Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: convergence of two epidemics. Lancet Infectious Disease. 2009;9(12):737-46.
- ^ Liamis G. Diabetes mellitus and electrolyte disorders. World J Clin Cases 2014;2(10):488-496.
- ^ Banandur P, Rajaram SP, Mahagaonkar SB, Bradley J, Ramesh BM, Washington RG, et al. Heterogeneity of the HIV epidemic in the general population of Karnataka state, south India. BMC Public Health 2011;11(Suppl 6):S13





