Abstract
Abstract
Introduction: Meningomyelocele is congenital defect in backbone of children and most common neural tube closure defect and malformations affecting brain and spine of children. It have high rate of morbidity and disability in survived children. This is the second most common caused for morbidity and mortality in children. global prevalence of Meningomyelocele has been reported to be 0.8–1 per 1,000 live births. The Hydrocephalus may affect as many as 80% of children with Meningomyelocele. use of periconceptional folic acid supplements, prevents ~50–75% of cases of neural tube defects the. This study aims to evaluate and clinical profile and use of folic acid in pericoceptual period by mother in rural area of western U.P., and outcome of children with Meningomyelocele.
Methods and Materials: 226 patients with Meningomyelocele admitted to SVBP hospital, Meerut and private in private hospitals of near by area between august2015 to dec’18, were analyzed prospectively. The data regarding clinical profile with associated congenital anomalies and supplementation of folic acid by mother in conceptuals period and post surgical disabilities were obtained by questionnaire- interview with the parents,drug history pertaining to drugs causing folic acid deficiency was unavailable as most of the patients belonged to low socio economic strata and were less literate. MRI was the essential investigation in all patients. The data was analyzed by SPSS 21.0 version.
Results: Mean age of presentation is 9.1 months. M:F ratio is 1.1:1. Lumbosacral region is involved in 73.5% patients. Hydrocephalus was the most common (63.71%, n=144) associated anomaly. In 92% cases there is no history of folic acid supplementation & all patients were from low socioeconomic status. Excision & repair of Meningomyelocele is the most commonly (80% n=180) performed surgery, dural patch was used to close the larger defect in 8.35%(n=15).and 20% patients were not operate due to various regions. In our study out of180 operated patients 80%(n=144) patients improved & discharged, and 6.6%(n=12) patients expired, 13.35%(n=24) patients left against medical advice (LAMA).
Conclusion: Low socioeconomic status & no maternal supplementation of folic acid in conceptual period are the important risk factors for the development of Meningomyelocele. Timely intervention with excision and repair gives good result. The use of Dural patch to closed the neural tube dural defect was good alternative, modified z-plasty can be use to cover large defects.
Keywords: Meningomyelocele, Hydrocephalus, Folic acid supplementation, Dural patch.
Introduction
Meningomyelocele is a birth defect in which the backbone and spinal canal do not close before birth. At four weeks of gestation, the lateral edge of the neural plates elevate towards each other and fuse to form a tube known as the neural tube. Failure of this process results in a neural tube defect.[1] The condition is a type of spina bifida,which may be open and occulta type. Neural tube defects are one of the most common congenital malformations affecting the brain and spinal cord & Meningomyelocele is one of the commonest neural tube closure defects due to dietary and folic acid deficiency. The global prevalence of Meningomyelocele has been reported to be 0.8–1 per 1,000 live births.[2],[3] Hydrocephalus may affect as many as 80% of children with meningomyelocele.[4],[5] The exact causes of neural tube defects are not known. Low intake of folic acid and poor dietary intake before getting pregnant and in early pregnancy increases the risk of having a foetus affected by NTDs, including Meningomyelocele.[6] The use of periconceptional folic acid supplements prevents ~50–75% of cases of neural tube defects. Proper management of affected children can lead to a meaningful & productive life and poorly managed cases of MMC can be a devasting obstacle not only for patients but also for the patient’s family. This study aims to evaluate clinical profile and use of folic acid in pericoceptual period by mother in rural area of western U.P and associated anomalies & outcome of children with Meningomyelocele.
Material and Methods
226 patients with Meningomyelocele admitted to SVBP hospital, Meerut in the department of surgery & department of paediatric medicine and operated in private hospital between August’15 to dec-18, were analysed prospectively. The data regarding clinical profile with associated congenital anomalies and supplementation of folic acid by mother in conceptuals period and post surgical disabilities were obtained by questionnaire- interview with the parents and patients themselves,drug history pertaining to drugs causing folic acid deficiency could not be available as most of the patients belonged to low socio economic strata and were less litrate. Follow up was done to note for complications. MRI was the essential investigation in all patients.TheDural patch, artificial dural substitute was used in some large dural defects and having poor dural membrane.The z-pasty and s- shaped flap rotation and modified rhomboid flap technique were used to cover the defect. The data was analysed by SPSS 21.0 version.
Results
In our series of 226 patients most patients (70.8%, n=80) presented at the age of less than 6 month. (Mean =9.0months.) One patient presented at the age of > 6 year (table: 1)
Table1: The sex ratio is M:F 1.1:1(table: 2)
|
Age group |
n |
% |
|
0-6 months |
160 |
70.8 |
|
6-12 months |
38 |
16.8 |
|
1-5 year |
26 |
11.5 |
|
>5 year |
2 |
0.9 |
|
Total |
226 |
100 |
Table 2: Most of the patients (51.3%, n=116) came from villages near by to Meerut district region. (table : 3)
|
Sex |
n |
% |
|
Male |
116 |
51.3 |
|
Female |
110 |
48.7 |
|
Total |
226 |
100 |
Table 3: Most commonly involved site was Lumbosacral region (n=166, 73.5%). while occipital region was the least commonly (2.7%, n=6) involved. (table: 4)
|
Region |
N |
% |
|
Meerut |
116 |
51.3 |
|
Out side the meerut |
110 |
48.7 |
|
Total |
226 |
10 |
Table 4: In most patients (57.52%, n=130) defect was large i.e > 5 X 5 cm[2]. (table: 5)
|
Site |
N |
% |
|
Cervical |
16 |
7.1 |
|
Dorsal |
18 |
8.0 |
|
Dorsolumbar |
4 |
1.8 |
|
Lumbosacral |
166 |
73.5 |
|
Occipital |
6 |
2.7 |
|
Sacral |
16 |
7.1 |
|
Total |
226 |
100 |
Table 5: Most common associated anomaly was Hydrocephalus (63.71%, n=144) followed by Arnold chiari malformation II (20.35%, n=46). (table: 6).
|
Size in cm2 |
n |
% |
|
Large (> 5 x 5 cm2) |
130 |
57.52 |
|
Small (< 5>2) |
96 |
42.48 |
|
Total |
226 |
100 |
Table 6: LSCS was the most common mode of delivery (n=69.9%, n=158), while 8.8%(n=20) patients were born by episiotomy. Normal vaginal delivery recorded in 21.23% (n=48) patients (table: 7)
|
Associated anomalies |
N |
% |
|
Hydrocephalus |
144 |
63.71 |
|
Acyanotic heart disease |
14 |
6.19 |
|
Adenoid hypertrophy |
2 |
0.88 |
|
Aqueductal stenosis |
1 |
0.44 |
|
Arnold chiari mal. Ii |
46 |
20.35 |
|
Cleft palate |
2 |
0.88 |
|
Ctev |
8 |
3.5 |
|
Distematomyelia |
3 |
1.3 |
|
Syrinx |
3 |
1.3 |
|
Tonsillar herniation |
3 |
1.3 |
Table 7: Periconceptional folic acid intake was absent in 92% (n=208) patients (table:8) & all 226 patients were from low socio-economic status and from rural area of western U.P. table no.8
|
Mode of delivery |
n |
% |
|
Episiotomy |
20 |
8.8 |
|
Lscs |
158 |
69.9 |
|
Nvd |
48 |
21.23 |
|
Total |
226 |
100 |
Table 8: Mean of total no. of births in a month in SVBP Hospital is 270.Mean of Neural tube defect found in unbooked patients means was not taking antenatal care is 9.7 while mean of Neural tube defect found in booked patients in a month is 1.2.
|
Folic acid intake in periconception period |
N |
% |
|
No |
208 |
92.0 |
|
Yes |
18 |
8.0 |
|
Total |
226 |
100 |
Most commonly performed operation was excision & repair of Meningomyelocele,and patients developed hydrocephalous are managed by Ventriculo-peritoneal shunt and some patients developed flap necrosis which was managed secondary closure of defect by modified rhomboid rotation of flap. Operation exision and repair was done in 80% (n=181). Patients who developed hydrocephalous in initial follow period were by V P shunt surgery. About 20% patients could not be operated due to various regions (n=46). (table: 9)
Table 9: Surgical site infection was the most common complication 30%(n=54) followed by CSF leak and flap necrosis.They were managed by appropriate antibiotic, acetazolamide and dressings and Ventriculoperitoneal shunt.
|
Operation |
N |
% |
|
Excision of mmc |
180 |
8o |
|
Not operated |
46 |
20 |
|
Total |
226 |
100 |
In our study out of180 operated patients 80%,(n=144) patients improved & discharged, and 6.6%(n=12) patients expired, 13.35%(n=24) patients left against medical advice (LAMA).(table:10).
Table 10:
|
Out come |
No. |
Percentage |
|
Improved and discharged |
N=144 |
80% |
|
Expired |
N=12 |
6.6% |
|
Lama |
N=24 |
13.4% |
|
Total operated |
N=180 |
100% |
 |
Click here to view |
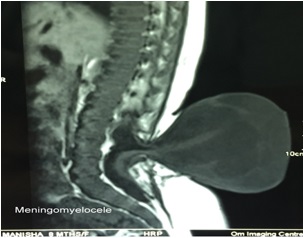
Fig. 1: showing lumber meningomyelocoele
 |
Click here to view |
Fig. 2: MRI of lumber meningocoele.
Discussion
Myelomeningocele (MMC), one of the most common congenital malformation of the central nervous system, has been described as “the most complex treatable congenital anomaly compatible with life”.[7] Failure of neural tube closure may occur anywhere along the neural axis. MMC occurs in 0.8-1 per 1000 live birth and incidence varies with environmental and genetic factors.[7],[8],[9]
In our series most patients (70.8%, n=160) presented to us before the age of 6 months (mean=9.1 months) & we found an inverse relation between the age & the incidence of MMC (table: 1). In our series the M:F ratio is almost equal i.e 1.1:1 while in a other study by Chand MB et al[10] M:F ratio is 3:2. In our series most common site of MMC is Lumbosacral () & in a series of 190 patients, Mirzai et al[11] also reported Lumbosacral region as a most common site for MMC. In comparison to other site Cervical MMC seems to have a better long-term neurological prognosis than low spinal MMC.[12],[13] Most common associated anomaly was Hydrocephalus (63.71% n=144) followed by Arnold chiari malformation II (20.35%,n=46)(table:6). Chand MB et al[10] reported association of hydrocephalus in 67.56% cases. The cause of hydrocephalus is related to Arnold chiari malformation. Caudal displacement of 4th ventricle with compression and thinning of upper medulla and cerebellum through foramen magnum into upper cervical spinal cavity, this defect permits CSF to exit caudally displaced 4th ventricle but prevents its ascension into cerebral cavity to be absorbed because the CSF flow is impeded by herniated tonsils of cerebellum. Studies related to MMC suggests that 37% MMC are associated with congenital heart disease however in our study 21.2%(n=48) patients were found to have congenital heart disease.[14] Out of 226 patients of our series 69.9% (n=158) patients were born by LSCS (table: 7). As it is the well known fact that maternal folic acid intake prevents development of neural tube defect. In our series mother of 92% (n=208) patients were not supplemented by folic acid. Mean of total no. of births in a month in our hospital is 270. Mean of neural tube defect found in unbooked patients is 9.7 while mean of neural tube defect found in booked patients in a month is 1.2. it clearly states that antenatal screening and folic acid supplementation is the crucial risk factor in the development of MMC. In this study drug history was unavailable because most of the attendants belonged to low socio economic status and were less litrate. In developed countries incidence in decreasing thanks to antenatal screening procedures, as well as dietary supplementation with folic acid to the women at risk prior to and during pregnancy. The prevalence of myelomeningocele has declined in developed countries of the world owing to both prenatal folate supplementation and to pregnancy termination following prenatal diagnosis. In United States before 1980 prevalence of myelomeningocele was 1-2/1000 live births, but more recently prevalence has declined to 0.44 per 1000 live births.[15],[16],[17],[18] Unfortunately, in third world countries prevalence is much higher, and acceptable prevalence data not available, nor has the issue been addressed with the goal of eradication, or reduction of incidence. The cause of MMC is multifactorial and includes genetic predisposition, nutritional deficiencies, particularly folate and zinc, use of anti-epileptic drugs like carbamazepine or valproic acid, diabetes mellitus (type-1), pre-pregnancy obesity and other non medical factors such as agricultural pesticides, radiation, hyperthermia and use of tobacco or drugs. Most commonly performed operation was excision & repair of MMC, (80%, n=180). 20%(n=46) patients not operated due to various reasons.(table:9). because, either patient referred to higher centre or left against medical advice due to various reasons including social stigma, financial issues, deficiencies related to manpower required for expertise in neonatal anesthesia & paediatric nursing care, deficiencies related to infrastructure like unavailability of paediatric ventilator, unavailability of neonatal warmer etc. In 57.52%(n=130) patients defect was large (5X5cm[2]). In 180 total operated patients, 80%(n=144) patients defect was closed by primary repair while 20%(n=36) patients required Z-plasty and rotation of flap and modified rombhoid technique. Dural patch were use to close the dural defects in 15 patients, which is good alternative to dural membrane. Closure of a large MMC defect is challenging for the reconstructive surgeon. The goals of closure are to preserve the function of the neural tissue and to prevent secondary infection.[19] If the MMC defect is small, direct repair can be performed; however, if the defect is large, various other reconstructive options are available[20] including modified rhomboid flap rotation. Surgical site infection was the most common complication followed by VP shunt malfunctioning’ CSF leak was seen in many patients. Hydrocephalus affects neurocognitive outcome and result in morbidity and mortality caused by shunt malfunction and infection.[21] Significant hydrocephalus may complicate the management of airway, reduced response to hypoxia and hence susceptible to post-operative apnoeic episodes.23 In our study out of180 operated patients 80% (n=144) patients improved & discharged, and 6.6%(n=12) patients expired, 13.35%(n=24) patients left against medical advice. Overall results in our series were encouraging.
Conclusion
The folic acid and dietary deficiencyin low socioecnomic status is the major cause and risk factor for meningomyelocoele there is need of strong recommendation of antenatal screening of the mother specially in low socioeconomic area, as low socioeconomic status and lack of folic acid supplementation are the important risk factors for the development of MMC.
Funding: Self.
Conflict of interest: None.
Ethical approval: The study was approved by the institutional ethics committee.
References
- ^ Wallingford JB. Neural tube closure and neural tube defects: studies in animal models reveal known knowns and known unknowns. Am J Med Genet C Semin Med Genet 2005;135C:59–68.
- a, b, c Greenberg F, James LM, Oakley GP., Jr Estimates of birth prevalence rates of spina bifida in the United States from computer-generated maps. Am J Obstet Gynecol 1983;145:570–573.
- ^ Lapid O, Rosenberg L, Cohen A. Meningomyelocele reconstruction with bilobed flaps. Br J Plast Surg 2001;54:570–572
- ^ De la Cruz R, Millan JM, Miralles M, Munoz MJ (1989) Cranial sonographic evaluation in children with myelomeningocele. Childs Nerve Syst 5:94–98.
- ^ Bowman RM, McLone DG, Grant JA. (2001) Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg 34:114–120
- ^ Botto LD, Moore CA, Khoury MJ. Neural-tube defects. N Engl J Med 1999;341:1509–1519.
- a, b Bunch WH,WH green, St. Louis PP. Modern management of mylomeningocele 1972; 168-174.
- ^ AM Adzick NS Fetal myelomeningocele. Naturalhistory, pathophysiology, and in-utero intervention. SeminFetal Neonatal Med 2010;15:9–14.
- ^ McLone DG, Knepper PA. The cause of ChiariII malformation: a unified theory. J PediatrNeurosci 1989;
- a, b http://www.pmjn.org.np/index.php/pmjn/article/download/78/76
- ^ Mirzai, H., Erşahin, Y., Mutluer, S. Child's Nerv Syst 1998;14:120.https://doi.org/10.1007/s003810050192
- ^ McLone DG Dias MS Complications of myelo meningocele closure. PediatrNeurosurg1991; 17:267-273
- ^ Ansari S, Nejat F, Yazdani S, Dadmehr M. Split cord malformation associated with myelomeningocele. J Neurosurg 2007;107:281-285.
- ^ Perez LM, Wilbanks JT, Joseph DB, Urological outcome ofpatients with cervical and upper thoracic myelomeningoceles. J Urol 2000;164:962–964
- ^ Cohen AR Myelomeningocele & Myelocystocele Pediatric Neurosurgery Robinson’s (ed) 4th Edition ch 203;3215-27.
- ^ Logan WJ. Neurological examination in infancy & childhood chapter 200 sections VII. Pediatrics;3169-3186.
- ^ MC Neely PD, Howe WJ. infectiveness of dietary folic acid supplementation on the incidence of lipomyelomeningocele: pathogenic implications. J Neurosurg 2004;100:98-100.
- ^ Mowatt DJ, Thomson DNP, Dunaway DJ. Tissue extension for the delayed closure of large myelomeningocele. J Neurosurg 2005;103:544-548.
- ^ El-khatib HA. Large thoracolumbar meningomyelocele defects: incidence and clinical experiences with different modalities of latissimus dorsi musculocutaneous flap. Br J Plast Surg 2004;57:411–417.
- ^ Campobasso P, Pesce C, Costa L, The use of the Limberg skin flap for closure of large lumbosacral myelomeningoceles. Pediatr Surg Int 2004;20:144–147.
- ^ Perez LM, Wilbanks JT, Joseph DB, Urological outcome ofpatients with cervical and upper thoracicmyelomeningoceles. J Urol 2000;164:962–964.





