Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

CRP levels and platelet count as markers of prognostic index in COVID-19 patients
Abstract
Background: Diagnostic tests like complete blood count (CBC) and C-reactive protein (CRP) are pivotal in diagnosing COVID-19 and assessing treatment outcomes. The presence of hyper coagulability and disseminated intravascular coagulation in COVID-19 patients correlates with diminished platelet counts.
Materials and Methods: A cross-sectional analytical observational study was conducted on 150 individuals diagnosed with COVID-19 between January 2022 and April 2022, utilizing data sourced from Dr. K.K.B.M. Subharti Hospital Dehradun. The study specifically targeted COVID-19 patients below 60 years old with confirmed RT-PCR test results. Medical records were scrutinized for laboratory findings regarding platelet count and CRP levels at the mentioned hospital. CRP levels were determined using the Turbidimetric method, while CBC was performed using Electrical Resistance Detection. Platelet isolation was achieved by rotating a blood sample in the Nihon Kohden Celltac alpha machine followed by microscopic examination. Data analysis was conducted using SPSS statistical software version 20.0 provided by IBM Corp.
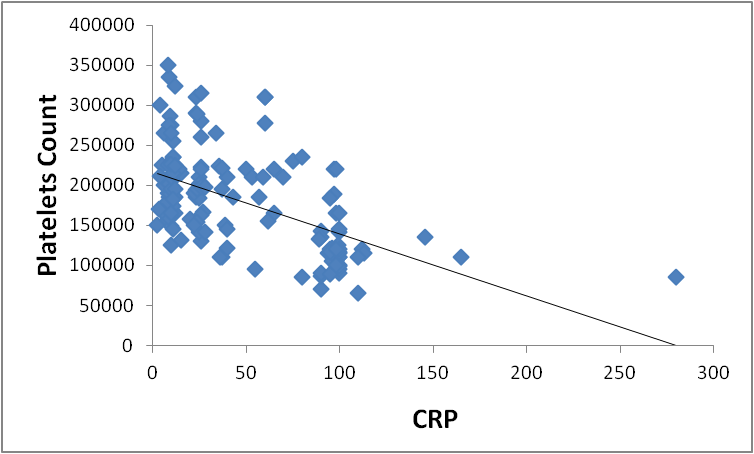
Results: A direct correlation between CRP concentrations and the COVID-19 severity was observed.(p<0.001) Platelet counts demonstrated a significant negative correlation with CRP levels (r = -0.491**, p < 0.01). This inverse relationship suggests a potential compensatory mechanism whereby platelets modulate inflammation and coagulation.
Conclusion: We concluded that Platelet count and CRP levels serve as crucial prognostic markers for determination of covid severity and for clinicians managing COVID-19 cases.
Introduction
The novel Corona virus disease (COVID-19) is a severe respiratory illness known for its high contagion and serious symptoms, often leading to significant fatality rates. It is caused by the SARS-CoV-2 virus.[1] The initial cases of the outbreak were documented in Wuhan, China, in December 2019. In COVID-19, the immune system can become overactive, causing tissue damage and potentially life-threatening outcomes. Laboratory tests such as complete blood count (CBC) and C-reactive protein (CRP) are crucial for diagnosing COVID-19 and determining prognosis, although instances of false negative results have been documented.[2] Biomarker changes in COVID-19 patients namely platelet count and CRP levels have been reported.[3], [4] The typical platelet count in blood ranges from 150 to 450×10^9 platelets per liter. Platelets are essential for hemostasis, as they help to prevent bleeding by forming blood clots during vascular injury.[5] The occurrence of hyper coagulability and disseminated intravascular coagulation in COVID-19 patients is associated with reduced platelet counts. C-reactive protein, an acute-phase inflammatory protein mainly synthesized in hepatocytes in the liver, contributes to the complement pathway activation during inflammation. Before a patients’ vital signs are affected or leukocytes are raised, elevation in CRP levels have been observed.[6] The typical CRP concentration in the bloodstream is less than 10 mg/L. However, during the early stages of the disease, CRP levels rise swiftly, peaking within 48 hours after the onset of symptoms.[7]
As the clinical spectrum of COVID-19 appears to be wide, encompassing asymptomatic infection, mild upper respiratory tract illness, severe viral pneumonia with respiratory failure, evaluation of relationship between platelet count and CRP, and severity could assist in treatment and improved prognosis. There is a need for simple tests to aid clinical management, as the behaviour of CRP levels in COVID-19 patients may help in providing important information for risk stratification related to poor outcome. Because of paucity of the data and research work on COVID-19 patients we consider this research study to be conducted in our institution.
Materials and Methods
An observational cross-sectional study was conducted among 150 COVID-19 positive patients from October 2021 to December 2021 by utilizing data obtained from Dr. K.K.B.M. Subharti Hospital Dehradun. Medical histories of COVID-19 patients with positive RT-PCR tests, under 60 years old, with laboratory findings for platelet count and CRP levels were acquired from medical records of Dr. K.K.B.M. Subharti Hospital Dehradun. Based on the guidelines of the MOHFW the patients were classified into mild, moderate and severe categories. CRP test was performed by Turbidimetric Immunoassay method. CBC was performed by Electrical resistance detection. For platelet isolation, a blood sample was run in the rotator and put in the machine (Nihon Kohden Celltac alpha), and microscopic analysis was done. Data analysis was performed using SPSS statistical software version 20.0 (IBM Corp). The Pearson Correlation test was used to elucidate the associations between CRP and platelet count. Data with a normal distribution were summarized as mean ± SD and analyzed by ANOVA test using open epi software. We used the chi-square distribution table to find the p-value associated with the calculated chi-square statistic and degrees of freedom. Data was tabulated and variables were analyzed using chi-square tests. A p-value of > 0.05 was considered non-significant.
Results
Our results highlight the importance of age as a factor in determining COVID-19 severity, with older individuals appearing to be more susceptible to severe outcomes.
|
Age Category |
Covid Severity |
Total |
||
|
Mild |
Moderate |
Severe |
||
|
<20 |
21 |
10 |
4 |
35 |
|
20-45 |
17 |
22 |
7 |
46 |
|
>45 |
18 |
19 |
32 |
69 |
|
Total |
56 |
51 |
43 |
150 |
[Table 1] Represents a detailed overview of the distribution of COVID-19 severity across various age categories. The severity levels are categorized into three groups: Mild, Moderate, and Severe. The data is segmented into three age categories: "<20" (less than 20 years old), "20-45" (between 20 and 45 years old), and ">45" (older than 45 years old). Among individuals under the age of 20, there were 35 total cases. Out of these, 21 cases were classified as Mild, 10 as Moderate, and 4 as Severe. Moving on to the 20-45 age group, there were 46 cases in total. Of these, 17 cases were identified as Mild, 22 as Moderate, and 7 as Severe. The >45 age category had the highest number of cases, with a total of 69 individuals affected. Within this group, 18 cases were classified as Mild, 19 as Moderate, and 32 as Severe.
Overall, the table provides an in-depth understanding of how COVID-19 severity is distributed across different age categories. It reveals that the >45 age group had the highest number of cases across all severity levels, whereas the <20 age group had the fewest cases overall. The data highlights the importance of age as a factor in determining COVID-19 severity, with older individuals appearing to be more susceptible to severe outcomes which may be because of the comorbidities associated with the older age groups.
In mild category, there is a positive correlation (0.097) between CRP Level and Covid severity. This suggests that individuals with higher levels of CRP, may exhibit a slightly increased severity of Covid symptoms in the mild category. In the moderate category, the positive correlation strengthens (0.301), indicating that individuals with elevated CRP levels may experience more moderate forms of the disease. In the severe category, the correlation is highest (0.740), indicating a strong association between elevated CRP levels and severe Covid cases. This suggests that severe Covid patients may have significantly higher levels of inflammation as measured by CRP.
In the mild category, there is a weak positive correlation (0.086) between Platelet Counts and Covid severity. This suggests that individuals with slightly higher platelet counts may experience slightly more severe symptoms in the mild category. In the moderate category, there is a weak positive correlation (0.117), indicating a similar trend where higher platelet counts may be associated with more moderate forms of the disease. In the severe category, there is a negative correlation (-0.223), suggesting that severe Covid cases may exhibit lower platelet counts. This abnormality in platelet counts may be indicative of the complex inter.([Table 2])
|
Variables |
Covid Severity |
||
|
Mild |
Moderate |
Severe |
|
|
CRP level |
0.097 |
0.301 |
0.74 |
|
Platelet Counts |
0.086 |
0.117 |
0.223 |
|
Variables |
Total no of Counts N = 150 |
Covid Severity |
p-value |
||
|
N = 56 |
N = 51 |
N = 43 |
|||
|
Mild |
Moderate |
Severe |
|||
|
CRP |
Mean Score |
9.67 |
40.04 |
101.68 |
<0.01 |
|
±SD |
3.46 |
20.27 |
34.35 |
||
|
Platelet counts |
Mean Score |
209732.14 |
204235.29 |
116325.58 |
<0.01 |
|
±SD |
50090.8 |
51248.956 |
26441.441 |
|
|
|
Platelet |
|
CRP level |
Pearson Correlation |
-.491** |
|
Significance value (2-tailed) |
<0.01 |
|
|
N |
150 |
CRP, a marker of inflammation, exhibited variation across different severity groups. Patients with severe conditions had the highest mean score of 101.68, indicating a heightened inflammatory response in severe conditions. In contrast, patients with moderate symptoms had a slightly lower mean score of 40.04, suggesting a relatively lower but still elevated level of inflammation. Platelet count, indicating blood clotting ability, displayed variations across variables. Patients under the mild category of COVID severity had the highest mean score of 209732.14, implying a relatively higher platelet count. In contrast, patients with moderate category and those over severe patients exhibited mean scores of 204235.29 and 116325.58, respectively, suggesting comparable platelets count between these groups. The results of the Chi-square test indicated a statistically significant relationship between the variables (Pearson Chi-Square = 171, df = 2, p < .05 for CRP and Pearson Chi-Square = 20.18, d.f = 2 and p < 0.05 for platelets count respectively).([Table 3])
Platelet counts exhibited a significant negative correlation with CRP levels (r = -0.491**, p < 0.01). This inverse relationship suggests a potential compensatory mechanism involving platelets in modulating inflammation and coagulation. ([Figure 1], [Table 4])
Discussion
Our analysis of platelet counts and CRP levels in our research underscores CRP as a robust predictor of adverse disease outcomes. Additionally, CRP serves as an independent predictor of severe or critical illness upon admission, surpassing other biological indicators. These findings align with those of a study conducted in Wuhan by Luo et al., where CRP exhibited an AUC of 0.783 in distinguishing disease severity upon admission, with a threshold of 41.3. In our study, CRP yielded similar outcomes with a sensitivity of 65%, specificity of 83.7%, positive predictive value (PPV) of 81.6%, and negative predictive value (NPV) of 68.2%.[8], [9] Findings from a separate systematic review[10] revealed that CRP levels were notably elevated in COVID-19 patients with severe illness compared to those without the disease. The objective of the meta-analysis was to furnish physicians with data aiding in the differentiation of patients exhibiting severe and mild COVID-19 symptoms. Previous studies have consistently demonstrated a direct correlation between CRP concentrations and the severity level as well as mortality rates linked with the disease.[11], [12] The similarity in findings aligns with our own research. Additionally, another study revealed a positive association between elevated CRP levels, heightened inflammation rates, and disease severity. [13], [14] Cytokine storm theory of COVID-19 which states that the innate immune system is activated releasing TNF-alpha, IL-6 and IL-1 might be responsible for the association of higher CRP with worse outcomes observed in the current study. A slight reduction in platelet count associated with severity contributes to disruptions in the coagulation process among COVID-19 patients. Evidence of clotting and vascular injury has been observed in the alveolar capillaries of COVID-19 patients. The mild decrease in platelet count in COVID-19 patients can be attributed to increased platelet consumption. [15] Possible mechanisms for decreased platelet count seen in COVID-19 patients with increasing severity in the present study might be due to platelet activation and subsequent clearance by reticuloendothelial system. Activation by increased thrombin generation and consumptive coagulopathy– Direct viral-platelet interaction activation–associated with formation of platelet-leukocyte aggregates. Furthermore, there is limited information regarding the role of platelets during the COVID-19 pandemic. Regular check-ups and consultations with a healthcare professional are crucial to monitor the patient's platelet count, as it can be influenced by factors such as age, gender, and ethnicity. When the platelet count drops too low (below 20,000 micro liters), the patient may be at risk of spontaneous bleeding. Conversely, if the platelet count increases excessively, the patient may face a heightened risk of blood clotting. However it is necessary to further investigate in order to expedite the initiation of treatment in COVID-19 patients and to optimise COVID-19 therapy in hospital care.
Conclusion
The findings of our study suggest that the variables (CRP and platelet count) and Covid severity are not independent of each other. Our findings provide valuable insights into the complex interactions among the biomarkers and contribute to our understanding of disease processes, assisting clinicians and researchers in disease monitoring and management. Disease progression, early therapeutic and palliative care can be enhanced with use of CRP as a biomarker in COVID-19 patients. A positive correlation between plasma CRP level and COVID severity was observed in our study. CRP estimation might serve as a early biomarker for detection of COVID-19 severity and help the clinicians in risk stratification and timely management. It is anticipated that raised levels of pro inflammatory marker CRP would result in the release of multimers capable of interacting with platelets, leading to platelet activation, micro thrombi, and platelet consumpttion.
Strengths Study
In Uttarakhand state of India, this is one of the first study of its kind reporting correlation between CRP and Platelet count in COVID-19 patients.
Limitation of the study
The lack of research into the mechanisms of various biomarkers that are commonly associated with the progression and prognosis of COVID-19.
The size of the sample may limit the interpretation of the results.
Source of Funding
We have not received any grant and funding for this research work.
Conflict of Interests
The author declares no conflict of interests.
References
- Sharma A, Farouk I, SL. COVID-19: A Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses. 2021;13(2). [Google Scholar] [Crossref]
- Pfoh E, Hariri EH, Misra-Hebert A, Deshpande A, Jehi L, Rothberg M. Late Diagnosis of COVID-19 in Patients Admitted to the hospital. J Gen Intern Med. 2020;35(9):2829-31. [Google Scholar]
- Ali N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J Med Virol. 2020;92(11):2409-11. [Google Scholar]
- Mei H, Luo L, Hu Y. Thrombocytopenia and thrombosis in hospitalized patients with COVID-19. J Hematol Oncol. 2020;13(1). [Google Scholar] [Crossref]
- Ziegler M, Wang X, Peter K. Platelets in cardiac ischaemia/reperfusion injury: a promising therapeutic target. Cardiovasc. Res. 2019;115(7):1178-88. [Google Scholar]
- Asakurah, Ogawa H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int J Hematol. 2021;113(1):45-57. [Google Scholar]
- Sproston N, Ashworth J. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018;9. [Google Scholar] [Crossref]
- Young B, Gleeson M, Cripps AW. C-reactive protein: a critical review. Pathology. 1991;23(2):118-24. [Google Scholar]
- Luo X, Zhou W, Yan X, Guo T, Wang B, Xia H. Prognostic Value of C-Reactive Protein in Patients With Coronavirus 2019. Clin Infect Dis. 2020;71(16):2174-9. [Google Scholar]
- Wang L. C-reactive protein levels in the early stage of COVID-19. Med Mal Infect. 2020;50(4):332-4. [Google Scholar]
- Guan W, Ni Z, Hu Y, Liang W, Ou C, He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. [Google Scholar]
- Chen W, Zheng K, Liu S, Yan Z, Xu C, Qiao Z. Plasma CRP level is positively associated with the severity of COVID-19. Ann Clin Microbiol Antimicrob. 2020;19(1). [Google Scholar] [Crossref]
- Tan C, Huang Y, Shi F, Tan K, Ma Q, Chen Y. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 2020;92(7):856-62. [Google Scholar]
- Stringer D, Braude P, Myint P, Evans L, Collins J, Verduri A. The role of C-reactive protein as a prognostic marker in COVID-19. Int J Epidemiol. 2021;50(2):420-9. [Google Scholar]
- Wool G, Miller J. The Impact of COVID-19 Disease on Platelets and Coagulation. Pathobiology. 2021;88(1):15-27. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.9-13
-
CrossMark
- Citation
- Received Date April 05, 2024
- Accepted Date August 09, 2024
- Publication Date March 12, 2025