Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Role of perfusion index in analysing post-operative analgesia in patients undergoing laparoscopic cholecystectomy under general anaesthesia
Abstract
Background: Vasoconstriction and a drop in the perfusion index (PI) are brought on by an unpleasant stimulus. The visual analog scale (VAS) is a subjective instrument for measuring pain. To employ PI as an objective measure for postoperative pain assessment, our study will correlate PI with VAS.
Materials and Methods: A study including 72 patients (18-50 years old) undergoing laparoscopic cholecystectomy was carried out prospectively through observation. The first timepoint (T1) in the postoperative phase, during which heart rate (HR), mean arterial blood pressure (MAP), peripheral oxygen saturation (SPO2), VAS, and PI were collected, was regarded as the initial request for analgesia. 1 mcg/kg of inj. fentanyl was utilized as a rescue analgesic. After thirty minutes of rescue analgesia, all previously listed parameters were recorded at the second timepoint (T2). The second request for rescue analgesia was taken as the third timepoint (T3) and thirty minutes later as the fourth timepoint (T4) and all the above-said parameters were recorded.
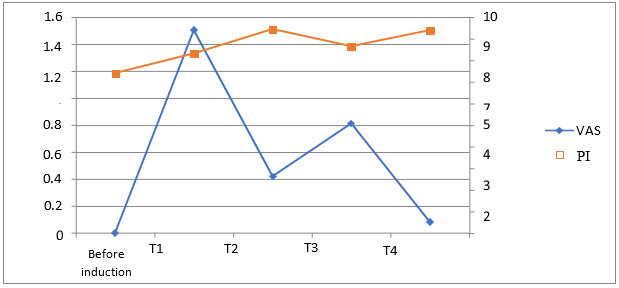
Results: PI increased after rescue analgesia from T1 (8.29±2.50) & T3 (8.63±2.49) to T2 (9.42±2.41) & T4 (9.38±2.54) respectively. This increase in PI between the time points were statistically significant with p-value <0.05. With respect to other parameters, PI shows a significant negative correlation between HR, MAP, SPO2 and VAS score at T2 and T4 with p-value <0.05. However, there was no significant correlation between SBP and PI at any time point.
Conclusion: Perfusion Index values can be utilized as a reference when choosing the right analgesic to treat postoperative pain as well as an objective instrument for assessing postoperative pain.
Introduction
The International Association for the Study of Pain (ISAP) defines pain as ' An unpleasant sensory and emotional experience associated with actual or potential tissue damage'.[1] In most cases, pain stems from a multifactorial physical origin. The subject perceives it through peripheral and central feedback mechanisms.[2] As pain represents the most unpleasant sensation, it should be the primary focus of management during treatment. It triggers the sympathetic nervous system, leading to the release of stress hormones that result in increased oxygen uptake.[3]
Pain is a complex subjective experience that poses challenges in quantification. The visual analogue scale stands as the predominant tool for pain evaluation.[4] The primary goal of pain assessment revolves around grading the severity of pain, which, in turn, aids in mitigating post-operative complications and in selecting suitable analgesics for the intensive care unit and post-operative ward.[5] PI and VAS score has been used as an objective and subjective measurement for the assessment of pain and analgesia. The perfusion index values range from 0.02% to 20% which indicates higher the PI better is the tissue perfusion.[6], [7]
The perfusion index can be used to measure peripheral perfusion when under general anesthesia. The index denotes the proportion of pulsatile to non-pulsatile blood flow inside peripheral vascular tissue, and it is ascertained through the measurement of infrared light absorption using a pulse oximeter.[8]
The perfusion index functions as an indirect, non-invasive, and continuous parameter for evaluating peripheral perfusion.[9] Sensations of pain during surgical procedures fluctuate over time due to their direct impact on the sympathetic nervous system. Consequently, alterations in the sympathetic nervous system influence smooth muscle tone and the perfusion index/peripheral perfusion.[10]
In laproscopic surgeries, various factors affect the PI such as patient's position, pneumoperitoneum and hemodynamic instability. Pneumoperitonium is created and patient is placed in reverse trendelenberg position during laparoscopic surgery. All these factors decrease the PI and this decrease in PI may cause tissue damage and other side effects due to a decrease in perfusion to the tissue organs.[11] Therefore, monitoring of PI during laparoscopic surgery is vital.[12] Given the known association between laparoscopic surgeries and significant post-operative pain, it is crucial to address the potential consequences such as hemodynamic and respiratory changes as well as delayed return to normal activity [13]. The study help to facilitate the administration of appropriate analgesia for patients, thereby reducing post-operative complications and enhancing the well-being of patients in post-operative care units and ICUs. This study's main goals were to determine the relationship between the visual analogue score (VAS) and the pulse oximetry perfusion index (PI) and to evaluate the tool's suitability for use as an objective means of measuring post-operative pain.
Materials and Methods
This prospective observational study was carried out at a government hospital following Enrolment in the Clinical Trial Registry of India under registration number (CTRI/2023/05/052476).
Inclusion criteria
The study included seventy-two patients aged 18 to 50 years, belonging to ASA (American Society of Anaesthesiology) I/II, scheduled for elective cholecystectomy under general anesthesia, and who were deemed conscious and able to cooperate during the immediate postoperative period.
Exclusion criteria
In this study patients with unstable hemodynamic parameters, a history of neurological, psychiatric, or chronic pain disorders, and pre-existing cardiovascular, pulmonary, or metabolic diseases were excluded.
Procedure
Three sections of a semi-structured questionnaire were used to collect data. Names, ages, sexes, and other sociodemographic details were gathered in the first section. The peripheral oxygen saturation (SPO2), mean arterial pressure, systolic and diastolic blood pressure, and baseline pulse rate were all recorded in the second section. Postoperative data such as pulse rate (HR), systolic and diastolic blood pressure, mean arterial pressure (MAP), spO2, PI, and visual analogue score (VAS) were recorded in the third section.
The visual analog scale (VAS) is a subjective instrument that depends on the patient's self-expression of pain level. Patients rate their level of pain on a range from 0 to 10. One hand was used to measure blood pressure while the other held the oximeter probe on its middle fingertip. If the SpO2 was less than 90%, an oxygen mask was put on. Every patient was watched until they asked to be given rescue medication. Pre-medication was given to each of the 72 study participants to guarantee their safety and comfort. This involved injecting intravenously with Inj. Glycopyrrolate (0.01 mg kg-1), Inj. Midazolam (0.01 mg kg-1), and Inj. Fentanyl (2 mg kg-1). Subsequently, intravenous induction was carried out using Inj. Propofol 2 mg kg-1 and Inj. Vecuronium 0.1 to produce muscular relaxation.
Immediately following induction, we meticulously observed their heart rate, blood pressure, mean arterial pressure, oxygen saturation, and perfusion index.
Clinical confirmation of endotracheal intubation was obtained, as well as by analyzing the capnographic waveform. End-tidal carbon dioxide (EtCO2) was maintained between 35 and 40 mmHg by adjusting the ventilatory rate while the patients were ventilated with a tidal volume of 6–8 mg kg-1. O2:N2O 40:60, isoflurane 1-1.5 vol%, and injectable vecuronium (0.01 mg kg–1) were used to maintain anesthesia. We made sure the patients' hemodynamic stability maintained steady during the entire surgical process. Following surgery, patients received cautious attention and were given injections of glycopyrrolate (0.01 mg kg-1) and neostigmine (0.05 mg kg-1) to aid in their recovery.
During the postoperative period, heart rate (HR), mean arterial blood pressure (MAP), peripheral oxygen saturation (SPO2), visual analog scale (VAS), and perfusion index (PI) were measured. The first timepoint (T1) was the initial request for pain treatment. The rescue analgesia was achieved by injection of 1 mcg/kg of fentanyl. The second timepoint (T2) was the half-hour following the rescue analgesia, during which all of the previously listed parameters were again measured.
The request for rescue analgesia that followed was labeled as the third timepoint (T3). The next timepoint (T4) was the 30-minute period that followed, during which time each of the previously mentioned parameters was recorded. The principal objective was to establish a correlation between the visual analog scale (VAS) and the pulse oximetry perfusion index (PI). Evaluating the pulse oximetry perfusion index as an objective means of assessing post-operative discomfort and its association with alterations in hemodynamic parameters was the secondary goal.
Statistical analysis
Statistical analysis of the data was performed using SPSS23.0 (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp). Descriptive statistics of HR, SBP, MAP, SPO2, VAS and PI were expressed using mean and SD. Categorical variables were expressed using frequency and percentage. The correlation of HR, SBP, MAP, SPO2, and VAS with PI was analysed using Karl –Pearson’s coefficient of correlation. A p-value <0.05 was considered statistically significant.
Results
A total of 72 patients (18-50 years) undergoing laparoscopic cholecystectomy were evaluated in this study. The mean age of the participants was 38.2+ 2.3 years. And majority of the patients were females (45) than males (27). Perfusion Index increased after rescue analgesia from T1 (8.29±2.50) & T3 (8.63±2.49) to T2 (9.42±2.41) & T4 (9.38±2.54) respectively. This increase in PI between the time points was statistically significant with p p-value <0.05.
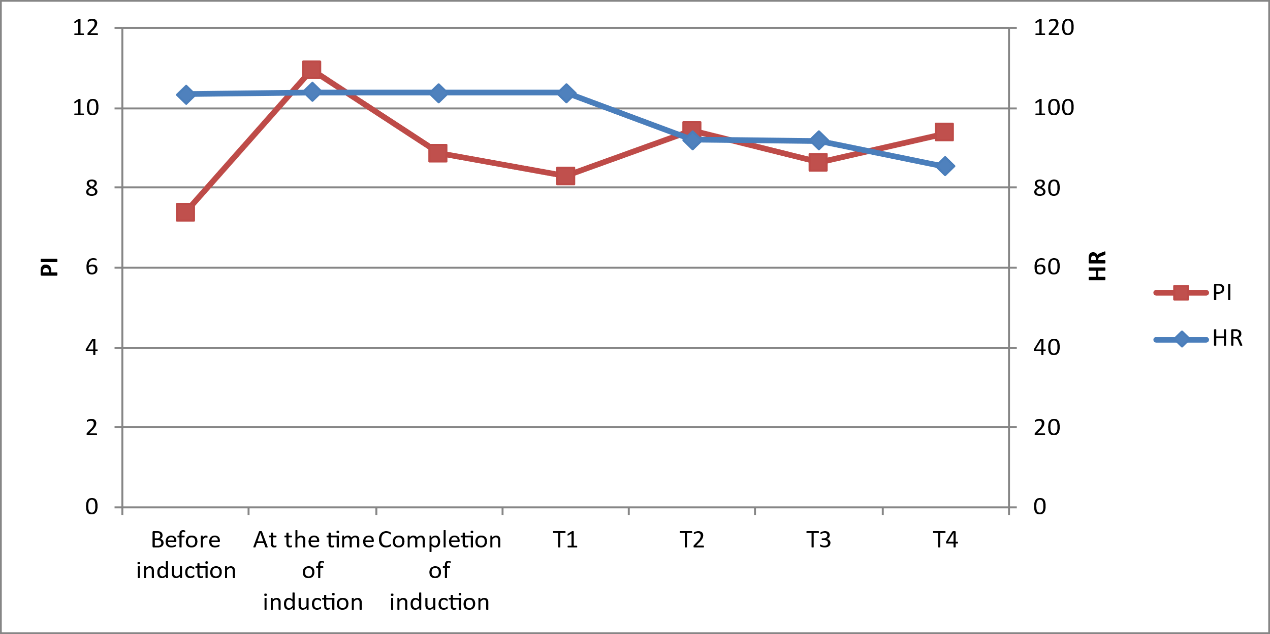
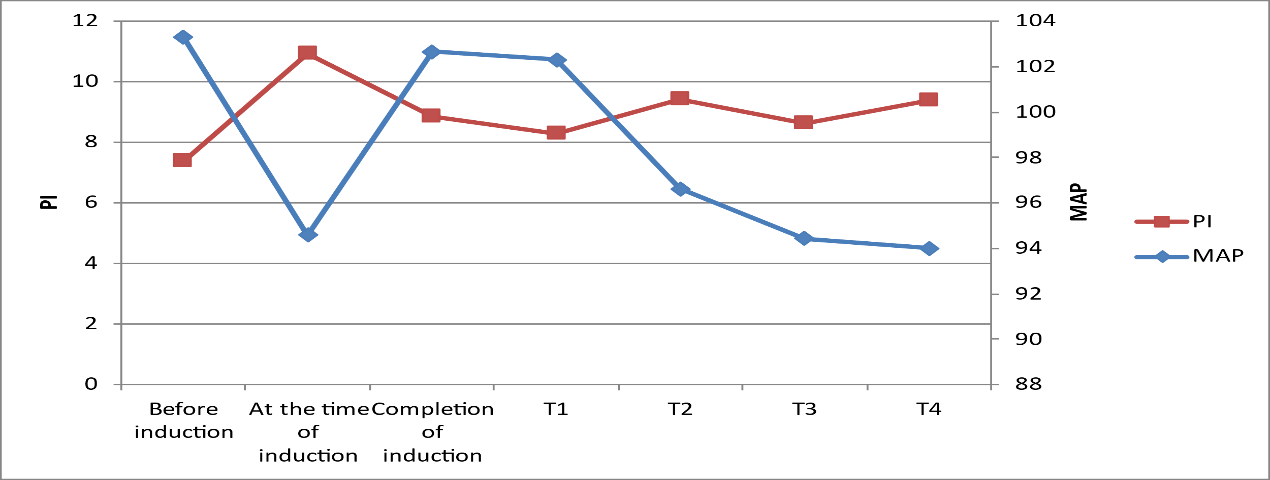
As shown in [Figure 1], after fentanyl administration, the Heart rate decreased from 103.78+/- 11.64 at T1 to 92+/-13.18 at T2. Mean arterial pressure readings decreased from 102.29+/-11.56mmHg at T1 to 96.61+/-9.91mmHg at T2 ([Figure 2]).
Systolic blood pressure readings decreased from 136.47+/-16.63 mmHg at T1 to 131.31+/-12.51 mmHg at T2 Perfusion Index shows a significant negative correlation between HR, MAP at T2 and T4 with p-value <0.05.
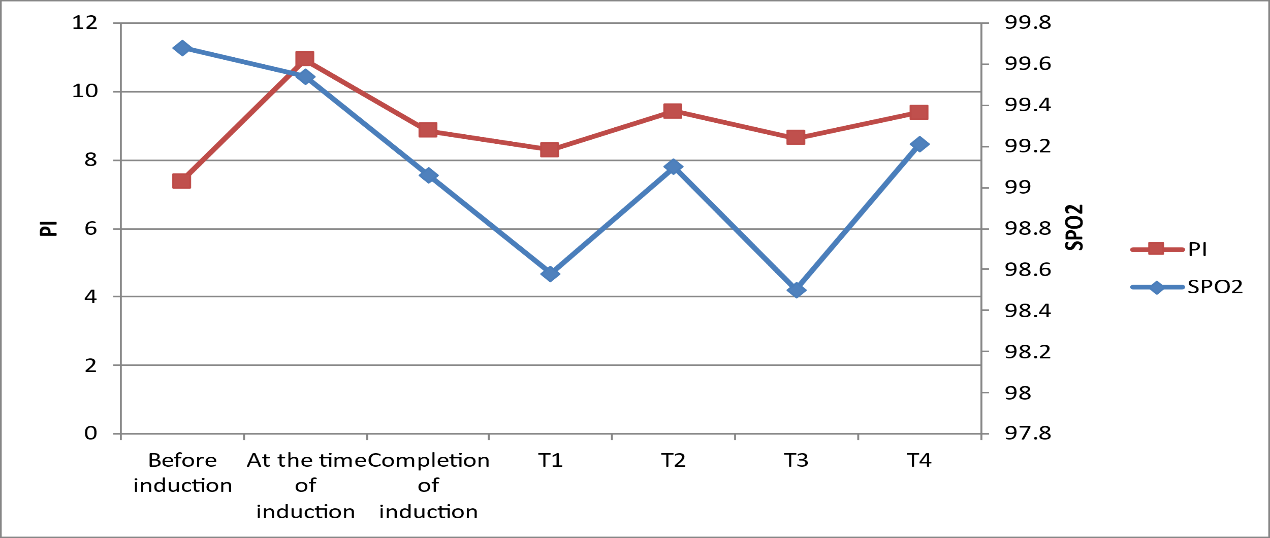
There was no significant correlation between Systolic blood pressure and perfusion index at any time point. Again, the Perfusion Index shows a significant negative correlation between SPO2 and VAS score at T2 and T4 with p-value <0.05 ([Figure 3], [Figure 4]).
Discussion
In the present study, we observed that after the administration of fentanyl, HR readings decreased from 103.78+/- 11.64 at T1 to 92+/-13.18 at T2. SBP and MAP readings decreased from (136.47+/-16.63) mmHg and (102.29+/-11.56) mmHg at T1 to (131.31+/-12.51) mmHg and (96.61+/-9.91) mmHg at T2 respectively.
Our study was similar to a study conducted by Dhanger S et al, in which, PI was significantly higher at T2 than at T1 (mean increase % = 92.2 ± 80.9%). The rise in PI was inversely proportional to VAS, HR and MAP with statistically significant p values. Hence, they concluded that PI can be added to other indicators of pain assessment in the post-operative care unit. [14]
As per study done by Sanjeev et al, the PI was significantly higher at T2 than at T1 (mean increase % = 94.3 ± 82.7%). PI was found to be inversely proportional to HR, VAS and MAP. The mean decrease % was 70.5±19.88%, 11.1±7.2% and 3.96 ± 5.01% in VAS, HR and MAP respectively.[15] This indicates PI increases with adequate pain relief as indicated by a decrease in VAS, HR and MAP. A decrease in VAS was associated with an increase in PI but the correlation was not statistically significant as the degree of the increase in PI in relation to the decrease in VAS was variable among patients and depends upon the subjective feeling of pain in patients. Our study showed a significant decrease in HR, MAP and VAS with an increase in PI with P < 0.05 after administration of intravenous fentanyl.
Next study done by Surekha et al, showed that PI values after fentanyl increased from 5.33 ± 2.67 (P1) to 5.99 ± 2.8 (P2) (P < 0.001) and to 6.3 ± 2.88 (P3) (P < 0.001).[16] This increase correlated with a decrease in HR (P <0.001). They concluded that PI can be a tool to monitor the nociception in anaesthetised patients during administration of analgesia. Similarly, our study also showed an increase in PI from 8.29 ± 2.50 (T1) to 9.42 ± 2.49 (T2) after giving intravenous Fentanyl with (P < 0.05) henceforth giving the conclusion that PI can be used as an objective tool to assess pain.
This study’s use of multiple exclusion criteria limits the usefulness of utilizing ASA grade I or II cases with non-fluid shift surgeries because it introduces a confounding variable. The study's small sample size is another drawback. An increased sample size could yield additional proof to bolster the initial findings presented here.
Conclusion
Perfusion Index values can be used as an objective tool for assessment of Post-operative pain and also to guide the selection of appropriate analgesics to relieve postoperative pain.
Ethical approval
This study was done after taking approval from the institutional ethical committee (MIMS/IEC/2023/697).
Source of Funding
None.
Conflict of Interest
None.
References
- Saleh A, Mostafa R, Hamdy A, Hafez A. Pulse-oximetry Derived Perfusion Index as a Predictor of the Efficacy of Rescue Analgesia After Major Abdominal Surgeries. Open Anesthesiol J. 2020;14:101-7. [Google Scholar] [Crossref]
- Lee J, Choi B, Jung Y, Lee Y, Bang J, Noh G. Evaluation of Surgical Pleth Index and Analgesia Nociception Index as surrogate pain measures in conscious postoperative patients: an observational study. J Clin Monit Comput. 2020;34(5):1087-93. [Google Scholar]
- Lal J, Bhardwaj M, Malik A, Bansal T. A study to evaluate the change in perfusion index as an indicator of successful ultrasound-guided supraclavicular block. Indian J Anaesth. 2021;65(10):738-43. [Google Scholar]
- Chung K, Kim K, Kim E. Perfusion index as a reliable parameter of vasomotor disturbance in complex regional pain syndrome. Br J Anaesth. 2018;121(5):1133-7. [Google Scholar]
- Sriganesh K, Theerth K, Reddy M, Chakrabarti D, Rao G. Analgesia nociception index and systemic haemodynamics during anaesthetic induction and tracheal intubation: A secondary analysis of a randomised controlled trial. Indian J Anaesth. 2019;63(2):100-5. [Google Scholar]
- Gibler R, Mano K. Systematic review of autonomic nervous system functioning in pediatric chronic pain. Clin J Pain. 2021;37(4):281-94. [Google Scholar]
- Vaghela A, Patel U, Saiyad J. Role of perfusion index as a tool for acute postoperative pain assessment in laparoscopic surgery. Natl J Med Res. 2021;11(4):131-3. [Google Scholar]
- Chu C, Huang Y, Chen Y, Lai L, Yeh H. An observational study: The utility of perfusion index as a discharge criterion for pain assessment in the postanesthesia care unit. PLoS One. 2018;13(5). [Google Scholar] [Crossref]
- Toyama S, Kakumoto M, Morioka M, Matsuoka K, Omatsu H, Tagaito Y. Perfusion index derived from a pulse oximeter can predict the incidence of hypotension during spinal anaesthesia for Caesarean delivery. Br J Anaesth. 2013;111(2):235-41. [Google Scholar]
- Bihani P, Pandey A, Jha M, Paliwal N, Jaju R, Solanki R. Comparing Perfusion Index and Visual Analogue Scores for Postoperative Pain Assessment Following Upper Limb Surgeries Under Supraclavicular Brachial Plexus Block: An Observational Study. Cureus. 2024;16(3). [Google Scholar] [Crossref]
- Kwon J, Park H, Sim W, Park J, Jung K, Oh M. Evaluation of the Intraoperative Perfusion Index for Correlation with Acute Postoperative Pain in Patients Undergoing Laparoscopic Colorectal Cancer Surgery. J Clin Med. 2019;8(9). [Google Scholar] [Crossref]
- Kupeli I, Kulhan N. Can Perfusion Index be used as an Objective Tool for Pain Assessment in Labor Analgesia?. Pak J Med Sci. 2018;34(5):1262-6. [Google Scholar]
- Chung K, Kim K, Kim E. Perfusion index as a reliable parameter of vasomotor disturbance in complex regional pain syndrome. Br J Anaesth. 2018;121(5):1133-7. [Google Scholar]
- GC, Singh A, Mohta M, Saxena A. Perioperative "stress dose" of corticosteroid: Pharmacological and clinical perspective. J Anaesthesiol Clin Pharmacol. 2019;35(2):147-52. [Google Scholar]
- Kumar S, Hussain M, Prakash J, Raghawendra K. Role of Perfusion Index as a Tool for Acute Post-operative Pain Assessment: An Observational Study. Indian J Anaesth Analg. 2019;6(5):1623-6. [Google Scholar]
- Surekha C, Eadara V, Kumar M. Evaluation of perfusion index as an objective tool to assess analgesia during laparoscopic surgeries under general anaesthesia. Indian J Anaesth. 2022;66(4):260-5. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.25-29
-
CrossMark
- Citation
- Received Date April 05, 2024
- Accepted Date August 09, 2024
- Publication Date March 12, 2025