Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Assessment of hearing in preterm babies of gestational age less than 35 weeks in a neonatal care unit in India
Abstract
Introduction: With advancing science and technology there is increased survival of preterms all over the world, along with various types of morbidity in survivors. We aimed to evaluate the burden of one such morbidity- loss of hearing, in those babies less than 35 weeks of gestational age by early initiation of screening tests and review at 3 and 6 months in a Neonatal Care Unit in India.
Materials and Methods: An observational study was undertaken in preterm babies born at gestational age <35 weeks from March 1st, 2020 to July 31st ,2021 in Neonatal Care Unit, High risk follow-up clinic and Audiological department of same hospital. After stabilization of the baby otoacoustic emission test (OAE) was done by ERO.SCAN OAE test system and also repeated at 3 months and Brainstem evoked response audiometry test (BERA) was done at 3 and 6 months after taking proper parental consent.
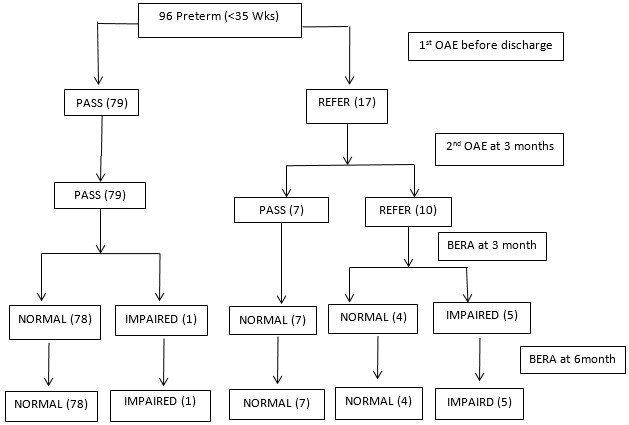
Results: Incidence of hearing impairment was 6.25% at 6month follow-up, with more incidence in extremely preterm (4.17%) and early preterm (2.08%). Exposure to various treatments showed statistically significant (p<0.05) association with hearing impairment. OAE before discharge and at 3months showed sensitivity of 85.71% but specificity of 87.64% and 95.51%, respectively. BERA at both 3months and 6 months shows 100% sensitivity and specificity.
Conclusion: Early initiation of screening test and follow up hearing assessment is crucial to detect hearing impairment in preterms.
Introduction
The introduction of new technologies and equipments in Neonatal Care Units has increased the life expectancy of preterms over the past few decades. Unfortunately, the prevalence of developmental disabilities among preterm survivors is still high[1] and among those disabilities mild motor, cognitive and behavioural problems are currently the most predominant ones.[2] Preterm birth is defined as delivery before 37 weeks of gestational age irrespective of birth weight and can be further subdivided into Extremely preterm, Very preterm, Moderate preterm and Late preterm, defined as infants born before 28, 28 to <32, 32 to <34 and 34 to <37 weeks of gestation respectively. Extremely preterms and Very preterms are more likely to have poor outcome than Moderately preterms and Late preterms.[3]
Pre-term infants and their immature organs encounter various stressors like infection, medications, many intensive modes of ventilatory support, oxygen therapy, surfactant, phototherapy, exchange blood transfusion etc which can adversely affect nervous system structure and function and it is more pronounced in more premature babies.[4] In the general population, hearing loss is relatively uncommon, with hearing loss being a significant disability in only 0.1% to 0.3% of infants,[5] while those who have been in Neonatal Care Unit for more than 5 days have a risk of 2% to 4%.[6] Etiology[6] of Hearing loss are as follows –
Genetic (50%)- 30% syndromic and 70% nonsyndromic.
Nongenetic (25%) - secondary to injury due to exposure of various risk factors[7] like infection, hypoxia, ischemia, hyperbilirubinemia, metabolic disease or ototoxic medication prolonged stay in neonatal intensive care unit, use of ECMO, ventilation etc.
Others (25%) – exact cause unknown.
Since there are very few number of studies evaluating the hearing assessment of preterms in our country, there is a necessity for research in this field to understand the degree of hearing loss by early screening tests in them so that early detection and early interventions can take full advantage of the plasticity of the child’s developing nervous system and optimize their linguistic, social, emotional, psychological and academic development.[8]
Materials and Methods
It was an observational study conducted from March 1, 2020 to July 31,2021 that is sixteen months at Neonatal Care Unit ,High Risk follow-up Clinic, Audiology unit of ENT department of a teaching hospital in India.
Sample Size calculation –
The following formula was used to calculate the appropriate sample size
N = {Z 2 p(1-p)}/d2; where-
N = Sample size,
Z = the standard normal variate. At 5% type 1 error (P<0.05), Z is 1.96,
p = Expected proportion in population,
Due to lack of proper existing data on the number of preterm infants less than 35 weeks of gestational age getting admitted to Neonatal Care Unit of a teaching hospital, a pilot study was conducted at the institution and the expected proportion of cases was found to be 20%.
d = Absolute error or precision kept at 8%;
N = {1.962 X 0.2(1-0.2)}/0.082 = 96.04 or 96
Therefore, the study was conducted with sample size of 96.
Inclusion Criteria
Preterm babies born at gestational age less than 35 weeks from March 1st, 2020 to July 31st, 2021 in a Teaching hospital in India.
Exclusion criteria
Newborns with of 35 weeks or more gestational age, babies having major/lethal congenital anomalies, hemodynamic instability, inborn errors of metabolism and who were lost on follow-up visit were excluded.
Methodology
After obtaining clearance from institutional ethics committee, the study was undertaken. After obtaining detailed informed consent from parents, infants were included in the study.
Study tools
A pre-designed semi-structured proforma- detailed history of antenatal, intrapartum and post-natal factors, systemic examinations and investigations. Gestational age was calculated from LMP or USG dating scan.
Screening tests- OAE and BERA- The currently acceptable methods in newborns for physiological hearing screening are otoacoustic emissions (OAE) and brainstem evoked response audiometry (BERA), recommended by American Academy of Pediatrics.
After hemodynamic stabilization, OAE was done by audiologist before discharge. The OAE test uses a probe placed in the baby’s ear to measure the inner-ear’s response to sound and normal results were interpreted as ‘PASS’, and abnormal results were interpreted as ‘REFER’. The test takes 1-5 minutes to be performed. Plan for repeat OAE and BERA at 3 months of age was advised. Repeat screening BERA was done at 6m of corrected gestational age. BERA uses electrodes that is placed on the baby’s head to record the brain-wave responses to ear clicks, which are then reported as NORMAL or Impaired. For mentioning ages for follow-up screening tests we have used corrected gestational age in all cases. A diagnostic BERA was done at 1year of corrected gestational age and it was considered as confirmatory.
Statistical analysis
Collected data were entered into a Microsoft excel enterprise 2010 spreadsheet. Analysis of the available data was performed by IBM SPSS Statistics for Windows, version 22.0. Armonk, NY:IBM Corp.2013. We have used percentage, sensitivity and specificity calculation and chi-square tests for our analysis. Statistical significance was accepted at the level of P value <0.05(95% confidence interval).
|
Screening tests |
Test negative |
Test positive |
|
OAE before discharge |
79(82.29%) Pass |
17(17.71%) Refer |
|
OAE at 3 months |
86(89.58%) Pass |
10(10.42%) Refer |
|
BERA(at 3 months) |
90(93.75%) Normal |
6(6.25%) Impaired |
|
BERA(at 6 months) |
90(93.75%) Normal |
6(6.25%) Impaired |
|
BERA at 6 months |
Normal N=90 |
Impaired N=6 |
p-value |
|
Gestational Age (weeks) |
|
|
|
|
Extremely preterm <28 weeks |
12 |
4(4.17%) |
0.004 |
|
Early pre-term 28-<32 weeks |
36 |
2(2.08%) |
0.0001 |
|
Moderate preterm 32-<34 weeks |
28 |
0 |
---- |
|
Late preterm 34-<35 weeks |
14 |
0 |
----- |
|
BERA At 6 months |
Normal |
Impaired |
p-value |
|
Treatment Received if any |
|
|
|
|
Respiratory support |
34 |
6 |
<0.001 |
|
Surfactant |
17 |
6 |
0.001 |
|
Inotropes |
27 |
6 |
<0.001 |
|
Phototherapy |
56 |
6 |
<0.001 |
|
Antibiotics |
35 |
6 |
<0.001 |
|
Anticonvulsants |
18 |
4 |
<0.001 |
|
Others |
31 |
5 |
0.01 |
|
Observation Only |
22 |
0 |
--- |
|
Preterm babies(n=96) |
OAE before discharge positive |
OAE before discharge negative |
OAE 3m positive |
OAE 3m negative |
BERA 3m positive |
BERA 3m negative |
BERA 6m positive |
BERA 6m Negative |
|
Hearing loss found (n=6) |
6(TP) |
1(FN) |
6(TP) |
1(FN) |
6(TP) |
0(FN) |
6(TP) |
0(FN) |
|
No hearing loss found (n=90) |
11(FP) |
78(TN) |
4(FP) |
85(TN) |
0(FP) |
90(TN) |
0(FP) |
90(TN) |
Results
Total 96 preterm babies were taken for the study, 47 (48.96%) were male and 49(51.04%) were female and 16 (16.67%) were extremely preterm (< 28 weeks), 38(39.58%) were very preterm (28-<32 weeks), 28 (29.17%) were moderate preterm (32-<34 weeks) and the remaining 14 (15%) were late preterm but less than 35 weeks of gestation (34-<35 weeks).
[Table 1] shows in OAE test done before discharge 79 (82.29%) had pass report and at 3 months 86(89.58%) had pass reports. A screening BERA was done at 3 m and 6m age , out of which , 6 (6.25%) tested impaired BERA and 90 (93.75%) tested normal BERA in both 3 months and 6 months of corrected gestational age. At 1yr confirmatory BERA test was done and it revealed same result as 6months BERA report means total 6 preterm babies had hearing impairment and 90 babies had normal hearing
[Table 2] shows out of 6pre-term subjects testing abnormal for BERA at 3 months, 6.17% were extremely preterm(<28wks) and 2.08% were in the gestational age range of early preterm (28-<32) weeks and none were in moderate and late preterm group. There is statistically significant association between impaired BERA at 6 months with lower gestational age since p-value in both extremely preterm (<28wks) and early preterm (28-<32weeks) is p<0.05, means more preterm babies are more prone to hearing impairment.
[Table 3] shows among the different types of treatment received by the normal reported BERA (n=90) and impaired BERA (n=6) there is statistically significant association between exposures of various therapy with impaired BERA reports (p<.0.05).
[Table 4] shows.OAE before discharge shows sensitivity of 85.71% and specificity of 87.64%, whereas OAE at 3months of age shows sensitivity of 85.71%and specificity of 95.51%, means OAE as screening test has more specificity when done at 3 months. BERA at both 3 months and 6 months shows 100% sensitivity and specificity proving it as a very good tool for screening test for hearing assessment below 6 months.
Discussion
Wroblewska-Seniuk k et al.[9] assessed the Polish Universal Newborns Hearing Screening Program (PUNHSP) database from 2010 - 2013 revealed, in infants born between 26 -28 weeks hearing deficit was 4.2%, in 29 -32 weeks it was 2.3% and in control group that is >=33 weeks hearing deficit was 0.2%., Another study by Hirvonen M et al.[10] in Finland (1991- 2008) revealed incidence of hearing loss in very preterm group was seven fold greater, two fold greater in mid preterm group and in late preterm group 1.5 fold greater than in the term group. A study by Jaideep Bhatt et al[11] displayed the incidence rate of permanent hearing impairment in NICU graduates were 5%. In our study the incidence rate of hearing impairment is 6.25% in preterm<35wks babies and among these 4.17% were extremely preterm (<28wks) and 2.08% early preterm(28-<32weeks) with statistical significant association (p<0.05) showing more preterm babies are more prone to hearing impairment. So hearing impairments decreased with advancing gestational age, similar to the findings of other authors.[9], [10], [11]
A study by Kumar et al[12] revealed hearing impairment was highly related with NICU admissions (72.7%) followed by hypoxia and low birth weight i.e.54.5% each. In another study by Wroblewska-Seniuk K et al [9] major risk factors were craniofacial abnormalities, very low birth weight, low scoring Apgar and ventilatory support.[9] Robertson et al. [13] displayed that mechanical ventilation and supplementation of prolonged oxygen were connected with high prevalence of hearing impairment in extremely preterm babies. In our study, pre-term babies who received respiratory support, surfactant, ionotropic support, phototherapy, antibiotics, anticonvulsants and other treatment(furosemide, dexamethasone, electrolyte correction, treatment for ROP) showed significant statistical value (p>0.05) and increased incidence of hearing impairment corroborates with the above mentioned studies.[12], [13]
A study by Yang HC et al [14] found that the majority of early refer OAE screening tests (91.3%) showed normal hearing and speech development by age 5 years and concluded that the hearing ability has improved in preterm infants over time. A study by Jaideep Bhatt et al [11] showed OAE was 70% sensitive and 61% specific at 0 month and 70% sensitive and 99% specific at 3 month. The sensitivity and specificity of BERA were 90% and 99% at 3 month and 100% and 99% at 6 month, respectively. Yousefi, Jaleh et al.[15] found in their study that OAE has a sensitivity 66.7% and a specificity of 98.8% in diagnosing hearing loss in newborns. Our study also corroborates with the above results according to sensitivity and specificity patterns of OAE and BERA emphasizing that rescreening decreases false positive rates. [16], [17], [18]
Conclusion
Every preterm babies should be periodically screened for hearing impairment and first screening must be completed before discharge with good screening tools as per availability of resources. Re-screening must be considered at 3 and 6 months to pick up the lost cases and also to decrease false positive rates so that with early diagnosis, early intervention could be done for better benefit for babies and proper counselling of parents and management plan could be implemented in our resource limited scenario.
Both OAE and BERA test need a calm baby and peaceful surroundings and Central hearing loss (where there is hearing impairment due to defective pathways from brainstem to auditory cortex) is not detected by these screening tests so these are limitations of our study.
Source of Funding
None.
Conflict of Interest
None.
References
- Saigal S, Doyle L. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261-9. [Google Scholar]
- Johnson S. Cognitive and behavioural outcomes following very preterm birth. Semin Fetal Neonatal Med. 2007;12(5):363-73. [Google Scholar]
- Do C, Kruse A, Wills B, Sabanathan S, Clapham H, Pedersen F. Neurodevelopment at 2 years corrected age among Vietnamese preterm infants. Arch Dis Child. 2020;105(2):134-40. [Google Scholar]
- Wallois F, Routier L, Bourel-Ponchel E. Impact of prematurity on neurodevelopment. Handb Clin Neurol. 2020;173:341-75. [Google Scholar] [Crossref]
- . American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898-921. [Google Scholar]
- Jane E, Jennifer B, Knorr A. Hearing Loss in Neonatal Intensive Care Unit Graduates. Cloherty and Starks Manual of Neonatal Care. . [Google Scholar]
- . Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J Early Hearing Detect Interv. 2019;4(2):1-44. [Google Scholar]
- Kumudha J. Follow up of high risk neonates. Indian J Pract Pediatr. 2009;11(4):329-36. [Google Scholar]
- -Seniuk KW, Greczka G, Dabrowski P, Szyfter-Harris J, Mazela J. Hearing impairment in premature newborns- Analysis based on the national hearing screening database in Poland. PLoS One. 2017;12(9). [Google Scholar] [Crossref]
- Hirvonen M, Ojala R, Korhonen P, PH, Eriksson K, Gissler M. Visual and Hearing Impairments After Preterm Birth. Pediatrics. 2018;142(2):1-10. [Google Scholar]
- Bhatt J, Kuchhal V, Saklani K, Kumar V. Accuracy of OAE and BERA to Detect the Incidence of Hearing Loss in Newborn”. J Evol Med Dent Sci. 2015;4(49):8466-74. [Google Scholar]
- Kumar A, Shah N, Patel KB, Vishwakarma R. Hearing screening in a tertiary care hospital in India. J Clin Diagn Res. 2015;9(3):1-4. [Google Scholar]
- Robertson C, Howarth T, Bork D, Dinu I. Permanent bilateral sensory and neural hearing loss of children after neonatal intensive care because of extreme prematurity: a thirty year study. Pediatrics. 2009;123(5):797-807. [Google Scholar]
- Yang H, Sung C, Shin D, Cho Y, Jang C, Cho H. Newborn hearing screening in prematurity: fate of screening failures and auditory maturation. Clin Otolaryngol. 2016;42(3):661-7. [Google Scholar]
- Yousefi J, Ajallouyean M, Mohammad,, Mahdieh H. The Specificity and Sensitivity of Transient Otoacustic Emission in Neonatal Hearing Screening Compared with Diagnostic Test of Auditory Brain Stem Response in Tehran Hospitals . Iran J Pediatr. 2013;23(2):199-204. [Google Scholar]
- Bansal S, Gupta A, Nagarkar A. Transient evoked otoacoustic emissions in hearing screening programs: protocol for developing countries. Int J Pediatr Otorhinolaryngol. 2008;72(7):1059-63. [Google Scholar]
- Bohnert M, Bohnert A. Hearing screening in newborn infant. Comparative studies and cost analysis with different instruments. Laryngorhinootologie. 2000;79(8):453-8. [Google Scholar]
- Coates H, Gifkins K. Newborn hearing screening. Aust Prescr. 2003;26:82-4. [Google Scholar]
Article Metrics
- Visibility 10 Views
- Downloads 4 Views
- DOI 10.18231/pjms.v.15.i.1.36-41
-
CrossMark
- Citation
- Received Date December 26, 2022
- Accepted Date August 02, 2023
- Publication Date March 12, 2025