Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Microbiological profile and risk factors of catheter associated urinary tract Infections (CAUTI) in adult intensive care unit in a tertiary care hospital, Maharashtra
Abstract
Background: Indwelling urethral catheter use is responsible for 70–80% of UTIs and is a major cause of sepsis. The research aims to investigate the prevalence, risk factors, and causative agents linked to urinary tract infections (UTIs) related to catheter use, along with understanding the antibiotic susceptibility patterns.
Aim & Objective: To determine the microbiological profile and risk factors associated with Catheter Associated Urinary Tract Infections (CAUTI).
Materials and Methods: A hospital-based cross-sectional study was conducted in the Department of Microbiology at a Tertiary care Hospital from August to December 2023, on 200 patients with indwelling catheters admitted in Intensive Care Unit. Urine samples were collected in an aseptic procedure and processed within a 2-hour timeframe. Uropathogen identification and Antibiotic Susceptibility Testing were done following CLSI guidelines 2023.
Results: A total of 200 patients with indwelling urinary catheter with an aggregate of 1457 catheter days over a period of 5 months. 32 were culture positive in clinically suspected cases of CAUTI. The CAUTI rate was 21.96 per 1000 catheter days with predominant etiological agents as Non albicans Candida 14 (43.75%) followed by E.coli 8 (25%) and Candida albicans 5 (15.63%).
Conclusion: This research offers foundational information on the rate of catheter-associated urinary tract infections (CAUTI), the predominant uropathogens, and associated risk factors within our institution.
Introduction
Urinary tract infections (UTIs) account for up to 40% of all Healthcare Associated Infections (HAI). Catheter Associated Urinary Tract Infection (CAUTI) is defined as a Urinary Tract Infection in a patient who was catheterized for more than 2 days with at least one of the following signs or symptoms: Fever (>38°C); urgency; frequency; dysuria; suprapubic tenderness; costovertebral angle pain or tenderness and a positive urine culture of ≥105 colony-forming units (CFU)/ml with no more than 2 species of microorganisms. Urinary catheterization in itself is a risk factor for Catheter associated urinary tract infection (CAUTI).[1]
The risk of a patient developing CAUTI increases by 3–7% each day the catheter remains in the patient. Approximately 12% - 16% of adult hospital inpatients will have an indwelling urinary catheter (IUC) at some time during their hospitalization.[2] This information will contribute to enhancing hospital infection control measures, shaping institutional antibiotic policies, and reducing the impact of infections acquired in healthcare settings.
Aim and Objectives
To determine the prevalence of Catheter Associated Urinary Tract Infection in Adult Intensive Care Unit (ICU) patients.
To assess the microbiological profile of isolates causing CAUTI and to determine the antibiotic susceptibility pattern of bacterial isolates.
Materials and Methods
The current cross-sectional study took place at a Tertiary care Hospital in Maharashtra over a span of five months (from August to December 2023). Our study obtained approval from the Institute’s Ethical Committee (IEC). The sample size was calculated using the formula:
Sample size = 4pqd2, with p (prevalence) = 14.67%, [3] d (allowable error) = 5%, Confidence interval = 95%. The sample size came as 200.
We included 200 patients [136 (68%) patients from MICU and 64 (32%) patients from SICU] admitted to the Medical Intensive Care Unit (MICU) and Surgical Intensive Care Unit (SICU) who underwent catheterization with indwelling urinary catheters (Foley's catheter) during this research period were included in this study.
Inclusion criteria
In this study all patients admitted to the Adult Intensive Care Units, including both Medical and Surgical ICU and who were catheterized with an indwelling urinary catheter for at least 48 hours will be included in this study and patients (or their caregivers) who gave consent are included.
Exclusion criteria
In this Patients whose sample taken at time of initial catheterization shows culture positivity, Patients catheterized prior to admission in ICU, Patients with renal anomalies, Patients or their caregivers who were not willing to give consent and Patients with history of antimicrobial therapy in last 7 days were exclued.
Study procedure
The study was started after obtaining the approval of the IEC. All the study participants were included in the study after we thoroughly explained the details of the study and the procedures involved, and informed consent was taken. For the patients who were on mechanical ventilation, informed consent was taken from Legally Authorized Representative (LAR). We assured the patients and their LARs that confidentiality will be maintained.
Urinary catheter care bundle, in accordance with the guidelines of the Healthcare Infection Control Practices Advisory Committee (HICPAC) from the Centers for Disease Control and Prevention, was implemented for all catheterized patients. Continuous monitoring of catheterized patients occurred daily, meticulously checking for local and systemic signs of Urinary Tract Infection (UTI). [4] In cases where UTI was clinically suspected in catheterized patients, a urine sample was promptly sent to the microbiology laboratory, and the details were documented.
Urinary catheter care bundle was implemented among all catheterized patients as per Standard guidelines. [5]
Specimen collection
Aseptic approach was employed during the retrieval of urine samples from patients with indwelling catheters. The preferred method involved obtaining urine directly from the sampling port. In cases where a sampling port was absent, the catheter tubing was securely clamped above the port, and the tubing surface was cleansed with 70% ethanol. Subsequently, urine was extracted using a needle and syringe. A minimum of 3 ml of urine sample was collected from Foley's catheter, ensuring the integrity of closed drainage system was maintained throughout the process. [6]
Transport of specimen
Urine samples were immediately transported to the Microbiology laboratory within 2 hours of collection and processed as soon as possible. When there is a delay in the transport of urine sample for more than 2 hours, boric acid (0.1g/10 ml of urine) was used as a preservative.
Processing of specimen
The urine samples were subjected to wet mount for evaluating the presence of pus cells, epithelial cells, RBCs and microorganisms.
Semi-quantitative culture was done by calibrated loop method on 5% sheep Blood agar and Cystine Lactose Electrolyte Deficient medium (CLED) agar and incubated in aerobic conditions at 370C for 16-18 hours. The urine cultures of colony count >105 Colony Forming Units (CFU)/ml with no more than two species of microorganisms were considered positive for CAUTI. Further biochemical tests were performed for species identification. Antibiotic susceptibility testing was performed by Kirby-Bauers disk diffusion method on Mueller Hinton agar as per the 2023 CLSI (Clinical Laboratory Standard Institute) guidelines. [7]
For fungal isolates, subculture was done in Sabouraud Dextrose Agar and LPCB mount was prepared from the colonies to examine yeast cells and pseudohyphae. Germ Tube Test (Reynolds Braude Phenomenon) was done. Species identification was done using Dalmou Culture in Corn Meal Agar.
Statistical tools
Data was collected using Epicollect5 software (v 5.1.7) and analyzed using Microsoft Excel (version 2019) and Jamovi software (v 2.4.11). Descriptive statistics such as Mean±Standard deviation and percentages (%) were calculated. For inferential statistics, we used Chi-square test to find associations. Statistical significance was noted at p<0.05.
Results
The CAUTI Rate was found to be 21.96 per 1000 catheter days in our study. A total of 200 ICU patients [136 (68%) patients from MICU and 64 (32%) patients from SICU] were included over 5 months with 1457 catheter days. A total of 47 (23.5%) patients were in mechanical ventilation (34 patients from MICU and 13 patients from SICU). In this study period, 32 were culture positive and 16% of patients had CAUTI.
In our study, both bacterial and fungal isolates were seen shown in [Table 1]. Non albicans Candida is the most predominant organism pertaining to 43.75%, following it Candida albicans were seen in 15.62%. Among Non-albicans Candida, C. glabrata was predominant showing 26.31% as shown in [Figure 1]. It was followed by C. tropicalis which showed 21.05%, C. parapsilosis by 15.78% and least by Candida dublinensis by 10.52% as shown in [Table 1].
Among bacterial isolates, Escherichia coli accounts to 25%, Pseudomonas aeruginosa to 6.25% and Klebsiella pneumoniae to 3.12%. Enterococcus species was the only gram positive cocci isolated in our study with 6.25%.
|
Organisms isolated |
CAUTI patients |
Percentage |
|
Enterococcus species |
2 |
6.25% |
|
Escherichia coli |
8 |
25% |
|
Klebsiella pneumoniae |
1 |
3.12% |
|
Pseudomonas aeruginosa |
2 |
6.25% |
|
Candida albicans |
5 |
15.62% |
|
Non Candida albicans |
14 |
43.75% |
|
Grand Total |
32 |
100% |
|
Candida species |
CAUTI patients |
Percentage |
|
Candida albicans |
5 |
26.31% |
|
Candida glabrata |
5 |
26.31% |
|
Candida tropicalis |
4 |
21.05% |
|
Candida parapsilosis |
3 |
15.78% |
|
Candida dublinensis |
2 |
10.52% |
|
Grand Total |
19 |
100% |

There is a slight increase in female gender of CAUTI cases (53.12%). We found that most of the cases belonged to middle age group (31-50 years) from MICU with 28.12% as shown in [Table 3].
|
Age groups |
Female |
Male |
Grand Total |
Percentage |
|
18 - 30 years |
13 |
16 |
29 |
14.5% |
|
31 - 40 years |
14 |
28 |
42 |
21% |
|
41 - 50 years |
23 |
16 |
39 |
19.5% |
|
51 - 60 years |
21 |
16 |
37 |
18.5% |
|
61 - 70 years |
16 |
20 |
36 |
18% |
|
71 - 80 years |
1 |
12 |
13 |
6.5% |
|
> 80 years |
0 |
4 |
4 |
2% |
|
Grand Total |
88 |
112 |
200 |
100% |
On comparing the months, October had highest CAUTI rate of 32.47 and November had lowest of 10.7 as shown in [Table 4].
|
Month |
CAUTI patients |
Number of Catheter days |
CAUTI Rate |
|
August |
5 |
323 |
15.48 |
|
September |
10 |
401 |
24.94 |
|
October |
5 |
154 |
32.47 |
|
November |
2 |
187 |
10.70 |
|
December |
10 |
392 |
25.51 |
|
Overall |
32 |
1457 |
21.96 |
Majority of the patients were catheterized for 5 - 10 days and the rate of CAUTI was more in this group of 81.25% with p value 0.32. Mean ± S.D = 7.29 ± 4.13. Most patients were catheterized for monitoring urine output (65%) as shown in [Table 5].
|
Indications |
No. of patients |
|
Acute urinary retention or bladder outlet obstruction |
22 (11%) |
|
In peri-operative / post-operative period |
48 (24%) |
|
Monitor urine output in critically ill patients |
130 (65%) |
|
Grand Total |
200 (100%) |
Regarding symptoms of CAUTI, 21 patients had fever, suprapubic pain and costovertebral angle tenderness each. 9 CAUTI patients had chills and rigor. Chi-square test was applied, and significant association were noted in all symptoms with CAUTI (p < 0.05), as shown in [Table 6].
|
Symptoms |
CAUTI patients |
Non CAUTI patients |
Total |
Chi-square value; p value |
|
Fever |
21 |
67 |
88 |
7.23; 0.007 |
|
Chills and rigors |
9 |
23 |
32 |
4.17; 0.041 |
|
Suprapubic pain |
21 |
69 |
90 |
6.55; 0.011 |
|
Costovertebral pain |
21 |
54 |
75 |
12.86; 0.0003 |
Routine urine examination of patients revealed that most CAUTI patients had turbid or cloudy urine (n=14; 43.75%), and it was statistically significant (𝛘2=88.6;p<0.001). In wet mount, it was noted that most CAUTI cases had presence of bacteria (n=20; 62.50%), followed by pus cells (n-14; 43.75%), yeast (n-14; 43.75%) and red blood cells (n=9; 28.13%). Statistical significance was noted in the presence of pus cells (𝛘2=3.72;p=0.045), bacteria (𝛘2=39.54;p<0.001) and yeast (𝛘2=13.4;p<0.001) as shown in [Table 7].
|
Routine urine examination |
CAUTI patients |
Percentage |
Chi-square value; p value |
|
Appearance of urine |
|||
|
Clear |
9 |
28.13% |
88.6; <0.001 |
|
Red and Cloudy |
9 |
28.13% |
|
|
Turbid / Cloudy |
14 |
43.75% |
|
|
Wet mount |
|||
|
Pus cells |
14 |
43.75% |
3.72; 0.045 |
|
Red blood cells |
9 |
28.13% |
0.201; 0.654 |
|
Bacteria |
20 |
62.50% |
39.54; <0.001 |
|
Yeast |
14 |
43.75% |
13.4; <0.001 |
[Table 8] shows theRelationship of co-morbidities with gender. Female preponderance was seen in most of the co-morbidities. Chi-square test was applied, and significant association were noted in cardiovascular disease and diabetes mellitus with gender (p < 0.05).
|
Comorbidities |
Males |
Females |
Total |
Chi-square value; p value |
|
Cardiovascular disease |
20 |
29 |
49 |
6.07; 0.014 |
|
Hypertension |
23 |
27 |
50 |
2.71; 0.1 |
|
Diabetes mellitus |
29 |
33 |
62 |
3.10; 0.048 |
|
Tuberculosis |
2 |
2 |
4 |
0.05; 0.81 |
|
Bronchial asthma |
12 |
8 |
20 |
0.144; 0.704 |
|
Chronic steroid intake |
2 |
4 |
6 |
1.29; 0.256 |
|
Chronic Kidney Disease |
25 |
26 |
51 |
1.35; 0.245 |
Among various risk factors of CAUTI, we found association with diabetes mellitus, hypertension, tuberculosis, bronchial asthma and chronic kidney disease as shown in [Table 9].
|
Risk factors |
CAUTI patients |
Percentage of CAUTI patients |
Chi-square value; p value |
|
Female gender |
17 |
53.12% |
1.29; 0.257 |
|
≥ 65 years of age |
6 |
18.75% |
0.0015; 0.969 |
|
≥ 5 days of catheterisation |
29 |
90.62% |
0.44; 0.507 |
|
Diabetes mellitus |
17 |
53.12% |
8.72; 0.003 |
|
Hypertension |
17 |
53.12% |
16.1; <0.001 |
|
Cardiovascular disease |
9 |
28.12% |
0.271; 0.603 |
|
Tuberculosis |
2 |
6.25% |
3.51; 0.046 |
|
Bronchial asthma |
6 |
18.75% |
3.24; 0.042 |
|
Chronic steroid intake |
1 |
3.12% |
0.00205; 0.964 |
|
Chronic kidney disease |
13 |
40.62% |
4.59; 0.032 |
There was a higher proportion of CAUTI patients in MICU than SICU. Chi-square test was applied, and there was no statistically significant association between CAUTI and the type of ICU (p > 0.05), as shown in [Table 10].
|
Type of ICU |
CAUTI patients |
Non-CAUTI patients |
Total |
Chi-square value; p value |
|
MICU |
24 |
112 |
136 |
0.858; 0.354 |
|
SICU |
8 |
56 |
64 |
Both the isolates of Enterococcus faecalis were sensitive to ampicillin, linezolid, teicoplanin, nitrofurantoin, tigecycline and vancomycin. Resistance was seen with penicillin and ciprofloxacin.
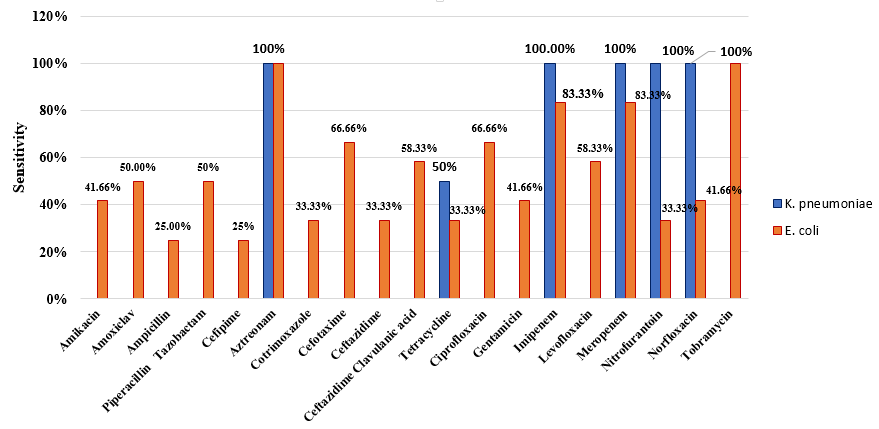
E.coli and Klebsiella pneumoniae were Enterobacteriaceae obtained in urine samples. E.coli isolates were predominantly sensitive to imipenem, meropenem, aztreonam, cefotaxime, ciprofloxacin and tobramycin. Klebsiella pneumoniae was sensitive to aztreonam, imipenem, meropenem, nitrofurantoin and norfloxacin as shown in [Figure 2].
2 isolates of Pseudomonas aeruginosa were grown and sensitive to ceftazidime, piperacillin tazobactam, tobramycin, levofloxacin, imipenem, meropenem and norfloxacin. They were resistant to cefepime and amikacin.
Discussion
Urinary pathogens can invade the body through a foreign device (such as a urinary catheter). While the bladder is usually sterile, the catheter tube provides a way for these bacteria to enter the body and potentially cause infection. [8] Catheter-Associated Urinary Tract Infection (CAUTI) is diagnosed when a patient with indwelling urinary catheter experiences one or more symptoms such as fever, suprapubic or flank pain, costovertebral angle pain or tenderness. [9]
In our study, the CAUTI rate is 21.96 per 1000 catheter days which is lower than Simaranjit Kaur et al. (26), [10] Sreedevi Hanumantha et al.(3.65), [11] Kazi et al. (4.59), [12] and Vishwajith et al.(1.74). [13]
The culture positivity rate of our study was 16% and seemed to be lower than Anggi A et al (44.4%). [14] The most common organism isolated in our study was Non albicans Candida accounting to 43.75% which is more than Khandare et al showing 35.19%. [15] They reported that Candida albicans was the predominant organism. In our study Candida albicans and Candida glabrata were grown in 26.31% cases each, which is lower compared to finding of Keten D et al showing C.albicans (52.4%). [16]
We found significant association between CAUTI cases and symptoms such as fever (10.5%), chills and rigor (4.5%), suprapubic pain (10.5%) and costovertebral angle pain (10.5%) and values were higher with Kaur et al. [10] with 18.5% having fever, 28% had rigors, 26.5% had suprapubic tenderness and 46.5% with costovertebral angle pain.
In the current research, an elevated incidence of CAUTI was observed with prolonged catheterization periods, reaching its peak when the duration exceeded 5 days (90.62%). Correspondingly, S Nivedita et al found a similar rise of 68%. [17]
Presence of pus cells, bacteria and yeast in urine showed association with CAUTI patients with p value <0.001. Comparing the study months, lowest CAUTI rate was seen in November with 10.70 and highest in October with 32.47. This change might be due to change in staff or behaviour towards infection prevention and control or change in patient characteristics (comorbidities, age distribution, duration of catheterization, and overall health status).
Risk factors associated with CAUTI include female gender, age, impaired immunity, co-morbidity, and increased duration of catheterization. [18] On analysing the risk factors, there was a positive association of CAUTI cases with diabetes mellitus (53.12%), hypertension (53.12%), tuberculosis (6.25%), bronchial asthma (18.75%) and chronic kidney disease(40.62%). Similar association of comorbidities with CAUTI cases was noted by Kaur et al., with diabetes mellitus (8.5%) and hypertension (39%). [10]
The CAUTI rate in MICU and SICU was 24.74 and 16.43 respectively. 24 patients (12%) had CAUTI in MICU and 8 patients (4%) in SICU. There was no association between type of ICU and CAUTI patients. A study conducted by Lewis et al. [19] in 2010 for a period of 2 years at North Carolina, United States showed similar higher CAUTI values in MICU (67.8%) than SICU (9.09%). This increase of CAUTI patients in MICU might be due to longer durations of catheterization in case of chronic illnesses, prolonged hospital stays and multiple comorbidities.
Bacterial isolates were sensitive to many drugs mainly urinary drugs like nitrofurantoin and norfloxacin. Resistance was seen with ciprofloxacin and penicillin in case of E.faecalis.
E.coli was the most common bacterial cause of CAUTI and was resistant to cotrimoxazole, ampicillin and cefepime. Klebsiella was sensitive only to imipenem, meropenem and aztreonam. P.aeruginosa was resistant to cefepime and amikacin.
Conclusion
Our study revealed that the prevalence of Catheter Associated Urinary Tract Infections (CAUTI) in the Adult Intensive Care Unit (ICU) of a tertiary care hospital in Maharashtra is significant. The CAUTI rate was calculated to be 21.96 per 1000 catheter days. Non-Candida albicans species (43.75%) and Escherichia coli (25%) were the most common pathogens isolated in the study. The antibiotic susceptibility patterns of the bacterial isolates demonstrated a high degree of resistance, emphasizing the need for vigilant antimicrobial stewardship.
Several risk factors were identified in association with longer catheterization duration (≥5 days), female gender, and comorbidities like diabetes mellitus and hypertension being significantly associated with an increased risk of CAUTI.
Recommendations
Strict adherence to catheter insertion and maintenance protocols is crucial. Implementing CAUTI preventive care bundles can significantly reduce infection rates. Regular training programs for healthcare professionals on the importance of aseptic techniques, early catheter removal, and recognizing early signs of infection can help in reducing CAUTI incidence.
Limitations
Our study has a limitation in that we did not conduct antifungal susceptibility testing. Given the increased difficulty in treating non-albicans Candida, there is a higher likelihood that these strains may persist.
Source of Funding
None.
Conflict of Interest
None.
References
- Werneburg G. Catheter-Associated Urinary Tract Infections: Current Challenges and Future Prospects. Res Rep Urol. 2022;14:109-33. [Google Scholar]
- Elvy J, Colville A. Catheter associated urinary tract infection: what is it, what causes it and how can we prevent it?. J Infect Prev. 2009;10(2):36-41. [Google Scholar]
- Parihar S, Sharma R, Kinimi SV, Choudhary S. An Observational Study from Northern India to Evaluate Catheter-associated Urinary Tract Infection in Medical Intensive Care Unit at a Tertiary Care Centre. Indian J Crit Care Med. 2023;27(9):642-6. [Google Scholar]
- Gould C, Umscheid C, Agarwal R, Kuntz G, Pegues D. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2009;31(4):319-26. [Google Scholar]
- Bennett J, Dolin R, Blaser M. . Mandell, Douglas, and Bennett’s Principles and Practices of Infectious Diseases. 2019. [Google Scholar]
- Procop G, Church D, Hall G, Janda W, Koneman E, Schreckenberger P. . Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. 2017. [Google Scholar]
- . CLSI (Clinical laboratory standard Institute). M100 Performance standards for Antimicrobial susceptibility Testing 33rd edition M100 ED33. CLSI. . 2023. [Google Scholar]
- Garibaldi R, Burke J, Britt M, Miller W, Smith C. Meatal Colonization and Catheter-Associated Bacteriuria. N Engl J Med. 1980;303(6):316-8. [Google Scholar]
- Parida S, Mishra S. Urinary tract infections in the critical care unit: A brief review. Indian J Crit Care Med. 2013;17(6):370-4. [Google Scholar]
- Kaur S, Dhaliwal K, Singh D, Randhawa R. A Study to Assess the Prevalence of Catheter-Associated Urinary Tract Infection among Catheterized Patients Admitted in Tertiary Care Hospital, Bathinda (Punjab). Int J Med Res Health Sci. 2021;10(7):34-42. [Google Scholar]
- Hanumantha S, Prakash H, Pilli K. Catheter associated urinary tract infection(CAUTI)-Incidence and microbiological profile in a tertiary care hospital in Andhra Pradesh. Indian J Microbiol Res. 2016;3(4):454-7. [Google Scholar]
- Kazi M, Harshe A, Sale H, Mane D, Yande M, Chabukswar S. Catheter Associated Urinary Tract Infections (CAUTI) and Antibiotic Sensitivity Pattern from Confirmed Cases of CAUTI in a Tertiary Care Hospital: A Prospective Study. Clin Microbiol: Open Access. 2015;4(2). [Google Scholar] [Crossref]
- Vishwajith, Sahkare R, Rao K, Sangeetha S. A study on catheter associated urinary tract infections (CAUTI) and antibiotic sensitivity pattern of uropathogens causing CAUTI from a tertiary care hospital. Indian J Microb Res. 2021;8(3):196-9. [Google Scholar]
- Anggi A, Wijaya D, Ramayani O. Risk factors for catheter-associated urinary tract infection and uropathogen bacterial profile in the intensive care unit in hospitals in Medan, Indonesia. Open Access Maced. Open Access Maced J Med Sci. 2019;7(20):3488-92. [Google Scholar]
- Khandare L, Barate D. Incidences of Candida Albicans and non-albicans among catheter-associated urinary tract infection patients of Akola city. Asian J Pharm Clin Res. 2017;10(11):115-7. [Google Scholar]
- Keten D, Aktas F, Tunccan O, Dizbay M, Kalkanci A, Biter G. Catheter-associated urinary tract infections in intensive care units at a university hospital in Turkey. Bosn J Basic Med Sci. 2014;14(4):227-33. [Google Scholar]
- Niveditha S, Pramodhini S, Umadevi S, Kumar S, Stephen S. The Isolation and the Biofilm Formation of Uropathogens in the Patients with Catheter Associated Urinary Tract Infections (UTIs). J Clin Diagn Res. 2012;6(9):1478-82. [Google Scholar]
- Job M, Monachan M, Scaria R, Babu M. Comparative study of Incidence rates and Antibiogram of Catheter associated Urinary Tract Infections in Intensive care unit versus Non Intensive care Unit at at Tertiary Care Teaching Hospital. Asian J Pharm Clin Res. 2021;14(6):167-72. [Google Scholar]
- Lewis S, Knelson L, Moehring R, Chen L, Sexton D, Anderson D. Comparison of Non-Intensive Care Unit (ICU) versus ICU Rates of Catheter-Associated Urinary Tract Infection in Community Hospitals. Infect Control Hosp Epidemiol. 2013;34(7):744-7. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.54-60
-
CrossMark
- Citation
- Received Date January 26, 2024
- Accepted Date August 13, 2024
- Publication Date March 12, 2025