Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Study of absent/unossified or hypoplastic nasal bone on ultrasound and its association with aneuploidies
Abstract
Introduction: Down syndrome is the most common chromosomal abnormality in neonates. Nasal bones are easily identifiable markers on genetic sonograms. AHNB in children with Aneuploidy has been detected by first and second trimester ultrasonography. Evaluation of nasal bone may constitute an additional marker to increase the efficacy of screening for trisomy 21 and can result in major reduction in the need for invasive testing.
Aim & Objectives: To study pregnancy outcome wherein fetuses are diagnosed with absent/unossified or hypoplastic nasal bone (AHNB) on ultrasound in first or second trimester of pregnancy and its association with aneuploidies.
Material and Methods: The retrospective study mainly aimed to evaluate the clinical value of AHNB alone or in combination with other soft markers or structural abnormalities for detection of aneuploidy. Total number of 92 patients with AHNB diagnosed on ultrasound over a period of 9 years were included and their outcome studied.
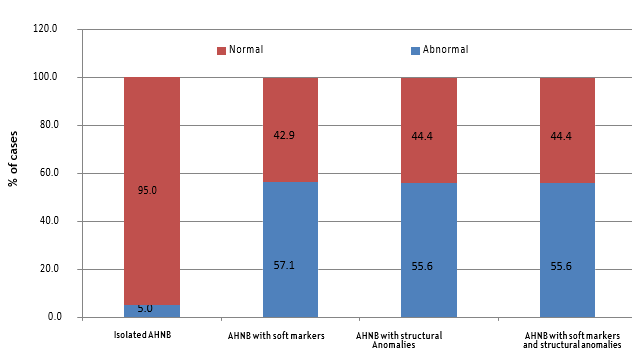
Results: Of 92 cases studied with AHNB 66.3% had normal pregnancy outcome. Isolated absent nasal bone was associated with abnormal karyotype in only 5% cases and those with soft markers or structural abnormalities were associated with abnormal karyotype in 56.25% cases. So, use of isolated AHNB in ultrasonography may not be an effective screening tool for Aneuploidy.
Conclusion: In case of finding of isolated absent nasal bone, counseling needs to be done, to assure the couple against pregnancy termination and if termination desired, not before karyotyping.
Introduction
Prenatal diagnosis is the science of discovering structural or functional anomalies and birth defects in the developing fetus. It is the testing for a disease or a condition in the fetus prior to birth.
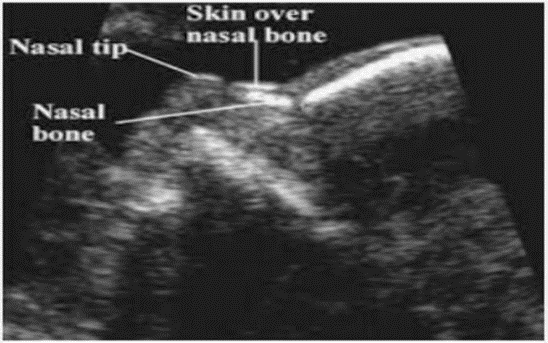
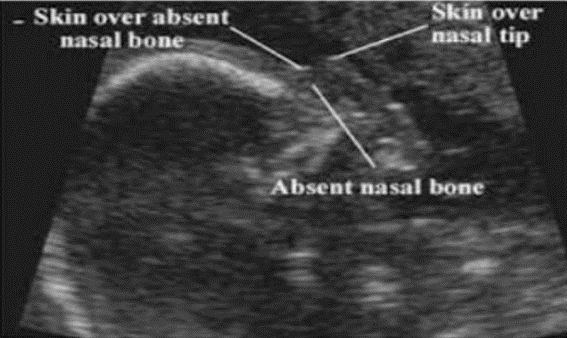
In a publication authored by Langdon Down: Observation of an ethnic classification of the idiots, he described a small nasal bone as one of the several phenotypic characteristics of Trisomy 21.[1] Flattened facial profile and small nose are common in newborns with Trisomy 21. [2] I studied the second instance of Langdon Down nasal hypoplasia in prenatal screening for trisomy 21.
Down syndrome is the prevailing chromosomal anomaly among newborns. Approximately 6000 infants are born with Down syndrome in a year, with a prevalence of approximately 1 in every 700 births. Nasal bone hypoplasia is characterized by a nasal bone length that falls below the 2.5th percentile for the duration of gestation. Nasal bones provide as distinct and recognizable indicators on genetic sonograms. Incidence of AHNB is 6.8% in Asian population. [3]
Absent/unossified or hypoplastic fetal nasal bone (AHNB) in foetuses with Down syndrome can be seen using sonography during the first and second trimesters. This has become a recognised indicator in prenatal ultrasonography. The assessment of the nasal bone can serve as an additional indicator to enhance the effectiveness of screening for trisomy 21, can lead to a significant decrease in the requirement for invasive testing and Noninvasive prenatal testing (NIPT).
Ultrasound detection of foetal structural defects is associated with an increased chance of aneuploidy such as Trisomy 21, Trisomy 13, Trisomy 18, Trisomy sex chromosomes and partial Trisomy etc. Roughly 33% of foetuses with trisomy 21 have significant abnormalities, however not all of them can be detected using sonography and only a portion of these abnormalities may be identified during the early stages of pregnancy. Soft markers are ultrasound findings that are not classified as malformations but signal an increased chance of foetal aneuploidy. [4] Some of the soft markers observed include nasal bone hypoplasia, thickening of the nuchal fold, presence of an echogenic intracardiac focus, choroid plexus cyst, minimal ventriculomegaly, presence of a single umbilical artery, mild pyelectasis, echogenic kidneys, echogenic bowel, short long bones and bilateral sandal gap.
Trisomy 21 (Down syndrome) is frequently identified chromosomal abnormality during prenatal diagnosis. Aneuploidy is the primary factor behind prenatal or neonatal illness and mortality, resulting in significant financial burden on pregnant women, their families and society at large. [5]
There have been different studies conducted all over world on the pregnancy outcome of AHNB and its correlation with aneuploidies, still there is limited data available in Indian literature. Using criteria based on Indian women may result in a higher incidence of chromosomal abnormalities. Research suggests that the length of the nasal bone is shorter in Indian fetuses as compared with other ethnicity. [6]
Studies have shown that between 0.5% and 2.8% of fetuses with a normal number of chromosomes exhibit a delay in the formation of the nasal bone during ultrasound examinations conducted in either the first or second trimester of pregnancy. Limited information is available on the significance of this after aneuploidy has been ruled out. A counseling challenge arises due to the lack of formal research addressing the results in these circumstances. Prevalence of this condition is higher in specific ethnic groups. However, further evidence is required to establish appropriate guidance for advising women of the potential risk of foetal anomalies when an AHNB is detected and invasive testing reveals a normal karyotype. [7]
The aim of this study is to analyze the results of pregnancies with ultrasonography showing an AHNB in the first or second trimester and to determine its association with aneuploidies. In this study, we examined the potential enhancement in trisomy 21 screening using the ultrasonography to assess the foetal nasal bone. The primary objective of the study was to assess the clinical significance of foetal absent nasal bone, alone or in combination with other soft markers or structural abnormalities, biochemical screening for identifying fetal chromosomal abnormalities.
Materials and Methods
A retrospective study was conducted. Ethical committee approval was obtained for the study. Total number of 92 patients with absent/unossified or hypoplastic fetal nasal bone (AHNB) diagnosed on ultrasound were included at Deenanath Mangeshkar Hospital and Research centre, Pune. Patients were identified through a computer search of the database maintained by the foetal medicine unit (sonocare software). All scans were performed by specialist accredited by Fetal Medicine Foundation (FMF), London for evaluating nasal bone, nuchal translucency and any other sonographic anomaly.
Inclusion Criteria
Patients who attended antenatal opd and genetics opd, which includes all women who had come diagnosed AHNB or diagnosis done in first or second trimester ultrasound showing fetus with AHNB over a period of 9 years.
Exclusion criteria
Patients with absent/unossified or hypoplastic fetal nasal bone with incomplete records, Patients who are lost to follow up.
Proformas were completed, all the gathered data was entered into SPSS and analyzed with descriptive statistics. Whether AHNB is an isolated finding or associated with other structural abnormalities on ultrasonography NT scan or anomaly scan were studied. Maternal medical records were examined to assess for fetal karyotype results and pregnancy outcomes like spontaneous abortion, termination, intrauterine death (IUD), preterm delivery and term pregnancy. For those who did not undergo prenatal invasive diagnostic procedures or in fetuses in whom any anomalies were present on ultrasound, newborn medical records were examined for physical examination results at birth and neonatal complications.
Results
During the study period, there were total 92 cases of absent/unossified or hypoplastic fetal nasal bone (AHNB) that were diagnosed in the hospital.([Table 1])
|
Age Group (years) |
No. of cases |
% of cases |
|
<35 |
82 |
89.1 |
|
≥35 |
10 |
10.9 |
|
Total |
92 |
100.0 |
|
Diagnosis of AHNB |
No. of cases |
% of cases |
|
Isolated AHNB |
52 |
56.5 |
|
AHNB with soft markers |
17 |
18.5 |
|
AHNB with structural anomalies |
9 |
9.8 |
|
AHNB with both soft markers and structural anomalies |
14 |
15.2 |
|
Total |
92 |
100.0 |
Of 92 cases studied, 56.5% had isolated AHNB, 18.5% had AHNB with associated soft markers, 9.8% had AHNB with associated structural anomalies and 15.2% had AHNB with associated both soft markers and structural anomalies in the study group.([Table 2])
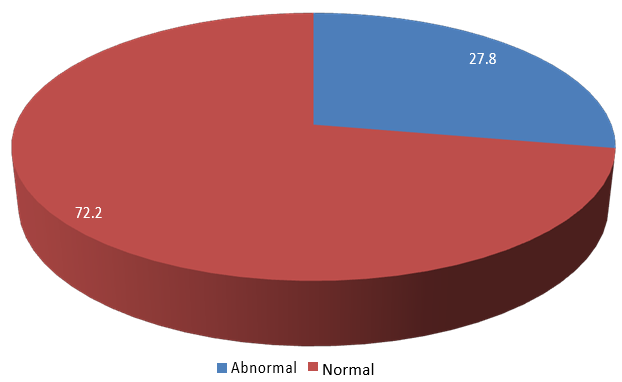
Of the 92 cases, 20 did not undergo karyotyping, leaving 72 cases for further analysis. Of 72 cases studied (on whom karyotying was done), 20 (27.8%) had abnormal karyotype and 52 (72.2%) had normal karyotype in the study group.([Figure 3])
|
Pregnancy outco |
Karyotype |
Total |
% of cases |
|
|
|
Done |
Not done |
|
|
|
Term / Preterm Delivery |
46 |
15 |
61 |
66.3 |
|
Termination of Pregnancy |
24 |
2 |
26 |
28.3 |
|
IUD |
2 |
1 |
3 |
3.2 |
|
Still Birth |
0 |
1 |
1 |
1.1 |
|
Spontaneous Birth |
0 |
1 |
1 |
1.1 |
|
Total |
72 |
20 |
92 |
100 |
Of 92 cases studied, 61 had normal pregnancy outcome i.e., term / preterm delivery and remaining 31 had abnormal pregnancy outcome i.e., Termination of pregnancy, IUD, still birth and spontaneous abortion.
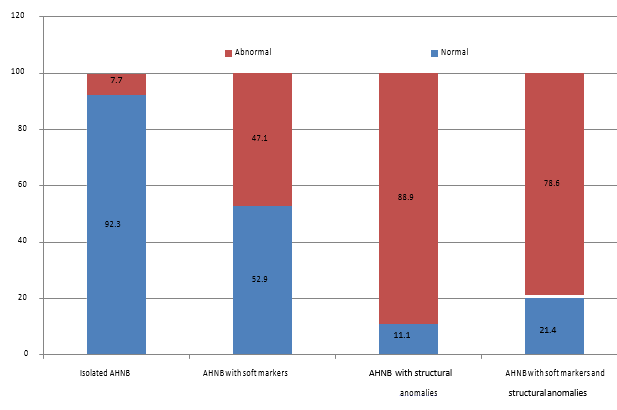
Of 52 cases with isolated AHNB, 48 had normal pregnancy outcome, 4 had abnormal pregnancy outcome.
Amniocentesis was done on 59 cases, out of which 45 had normal karyotype and 14 had abnormal karyotype. Post-delivery karyotype performed on one baby, it was normal karyotype. Abortus karyotyping was done in 12 cases.
P-value by Chi-Square test <0.05 is considered to be statistically significant. The distribution of incidence of abnormal karyotype is significantly higher among the group of cases with AHNB associated soft markers or structural abnormality compared to group of cases with isolated AHNB in the study group (P-value<0.001).
|
Screening |
No. of cases |
% of cases |
|
Not done |
12 |
13.1 |
|
Screen Negative or low risk |
48 |
52.2 |
|
Screen Positive or high risk |
32 |
34.7 |
|
Total |
92 |
100.0 |
Out of 32 with screen positive, 28 patients underwent karyotyping and 36 out of 48 patients with screen negative underwent karyotyping. Out of those, 15/28 (53.6) and 4/36 (11.1%) had abnormal karyotype.
Discussion
Of 92 cases studied with AHNB, 61 (66.3%) had normal pregnancy outcome. Of the 92 cases, 20 did not undergo karyotyping, leaving 72 cases for further analysis.
The mean of age in the group was 29.1 ± 4.4 years and the minimum – maximum age range was 19 – 43 years. Of 92 cases studied, 89.1% were of age less than 35 years and 10.9% were of age more than or equal to 35 years. Of the 10 cases of more than or equal to 35 years age, 6 had abnormal karyotype. That means 30% patients with abnormal karyotype were more than or equal to 35 years age. This is comparable to studies of Hirak D et al. [8] 23.68 % and with Zournatzi V et al. [9] 30% of trisomy 21 occurred in mothers over the age of 35. Advanced maternal age is associated with an increased chance of aneuploidies, by non-disjunction of the chromosomes at the time of maternal oogenesis. This makes it a significant factor in the likelihood of foetuses having chromosomal abnormalities. [10]
Among those who underwent karyotyping, 27.8% had abnormal karyotype which is comparable to Li H et al. [11] 27.8% and Yan du et al.[12] 22.54%.
Isolated AHNB was associated with abnormal karyotype in only 5 % cases. Our study rate is comparable with Lin R et al i.e, 4.5%,[5] Yan du et al i.e,7.14%[12] and Desai P et al i.e,8.4%. [13]
Isolated AHNB was associated with 92.3% had normal pregnancy outcome. This was comparable to Prasad CS et al. (86.7%). [14]
So, use of isolated AHNB in ultrasonography may not be a reliable method for screening Down's syndrome. When seen along with soft markers or structural abnormalities were associated with abnormal karyotype in 56.25% cases is comparable with Dash et al. [15] 41.4% and Yan du et al. [12] 44.83%. The distribution of incidence of abnormal karyotype is significantly higher among the group of cases with AHNB associated soft markers or structural abnormality compared to group of cases with isolated AHNB in the study group (P-value=0.001). This can be used for appropriate counseling of couples.
Amniocentesis is recommended for fetuses that have a structural abnormality or additional soft marker, which should be thoroughly examined by a skilled sonologist.
Of the patients with positive biochemical screening, 53.6% had abnormal karyotype. We found significant difference in abnormal karyotype status between group of cases with positive and negative biochemical screening. My study had sensitivity of 79% and specificity of 71%.
Out of 20 abnormal karyotype, 15 were Trisomy 21(most common aneuploidy), one Trisomy 13, one Trisomy 18, one Trisomy sex chromosomes, one partial trisomy 18q21 and one partial trisomy 5p+.
Limitations of this study is that the nasal bone assessment is an observer dependent variable. So specialist with appropriate training is necessary to use this parameter for aneuploidy screening.
Incidence calculation of AHNB limited as the study population was selected on the bias of AHNB.
All 92 patients did not undergo karyotyping, so karyotype status of all patients was not known.
Conclusion
All pregnant women irrespective of maternal age should undergo prenatal screening.
Isolated nasal bone was associated with abnormal karyotype in only 5 % cases and in majority of cases this is a normal variation. In case of finding of isolated AHNB, counseling needs to be done, to assure the couple against pregnancy termination and if termination desired, not before karyotyping. Positive biochemical screening is strongly associated with abnormal karyotype. So, these cases should always be offered karyotyping/ noninvasive Prenatal Testing. The first-trimester anomaly scan does not serve as a substitute for the second-trimester anatomic survey, which continues to be the most complete fetal structural evaluation. But the first trimester screening offers the option for earlier diagnosis of major anomalies.
Clinical interpretation of various soft markers should be done judiciously prior to opting for invasive test and termination of pregnancy.
Abbreviation
AHNB- Absent/unossified or hypoplastic nasal bone, NIPT- Non-invasive prenatal testing.
Source of Funding
None
Conflict of Interest
None
Acknowledgments
I sincerely thank all the doctors, fetal medicine department, medical record department and other hospital staff who participated in management of the patients. I am thankful to the ethics committee of hospital for permitting me to conduct this study.
References
- Down J. Observations on an ethnic classification of idiots. Lond Hosp. 1866;3:259-62. [Google Scholar]
- Jones K. . Smith‘s Recognizable Patterns of Human Malformation. 1997. [Google Scholar]
- Cicero S, Longo D, Rembouskos G, Sacchini C, Nicolaides K. Absent nasal bone at 11-14 weeks of gestation and chromosomal defects. Ultrasound Obstet Gynecol. 2003;22(1):31-5. [Google Scholar]
- Viora E, Errante G, Sciarrone A, Bastonero S, Masturzo B, Martiny G. Fetal nasal bone and trisomy 21 in the second trimester. Prenat Diagn. 2005;25(6):511-5. [Google Scholar]
- Lin R, Zhao F, Li J, Yan Y, Ren Y. Absence of nasal bone in fetuses with trisomy 21 at second trimester of pregnancy. Int J Clin Exp Med. 2017;10(6):9358-63. [Google Scholar]
- Sharma A, Tayal T, Narayani B, Radhakrishnan P, Kaul A. Nasal bone length: the long and short of it. Evaluation of the reference values for the fetal nasal bone length at 16 to 25 weeks of gestational age in an Indian population. Prenat Diagn. 2013;33(8):800-3. [Google Scholar]
- Dukhovny S, Wilkins-Haug L, Shipp T, Benson C, Kaimal A, Reiss R. Absent fetal nasal bone: what does it mean for the euploid fetus?. J Ultrasound Med. 2013;32(12):2113-4. [Google Scholar]
- Hirak D, Giriraj K, Rita P, Arpita G, Priyanka S, Tulika N. Study of the Relation of Maternal Age with Down Syndrome. Int J Health Inf Med Res. ;2(2):9-12. [Google Scholar]
- Zournatzi V, Daniilidis A, Karidas C, Tantanasis T, Loufopoulos AA, Tzafettas J. A prospective two years study of first trimester screening for Down Syndrome. Hippokratia. 2008;12(1):28-32. [Google Scholar]
- Ryu H. Should advanced maternal age be a reasonable indication for invasive diagnostic testing?. Obstet Gynecol Sci. 2013;56(3):135-6. [Google Scholar]
- Li H, Yao Y, Zhang C, Qin Y, Zeng L, Song J. Prenatal diagnosis and outcomes in 320 fetuses with nasal bone anomalies. Front Genet. 2023;14. [Google Scholar] [Crossref]
- Du Y, Ren Y, Yan Y, Cao L. Absent fetal nasal bone in the second trimester and risk of abnormal karyotype in a prescreened population of Chinese women. Acta Obstet Gynecol Scand. 2018;97(2):180-6. [Google Scholar]
- Desai P, Chauhan B, Jhawar M. Outcome of Pregnancies with Isolated Absent Fetal Nasal Bone in the Second Trimester. J Fetal Med. 2019;6(1):31-4. [Google Scholar]
- Prasad C, Kunjukutty R, Krishnan V. Fetal absent/hypoplastic nasal bone: a single center follow up study from a tertiary referral hospital in India. Int J Reprod Contracept Obstet Gynecol. 2020;9(11):4606-11. [Google Scholar]
- Dash P, Puri R, Goyal M, Bijarnia S, Lall M, Kotecha U. Absent/Hypoplastic Fetal Nasal Bone and Its Association with Aneuploidies. J Fetal Med. 2015;2(2):75-8. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.99-103
-
CrossMark
- Citation
- Received Date February 28, 2024
- Accepted Date May 29, 2024
- Publication Date March 12, 2025