Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Evaluating suspected cases of tubercular lymphadenopathy: A comparative analysis of fine needle aspiration cytology, CBNAAT and AFB screening with Ziehl-Neelsen staining
Abstract
Introduction: Tubercular lymphadenopathy poses a diagnostic challenge due to its varied clinical presentations and overlapping features with other diseases. The incidence of tuberculosis in India has dramatically increased and contributing to it is Human Immunodeficiency Virus (HIV). Preliminary findings suggest that FNAC provides rapid cytological insights but may lack specificity. AFB screening using Ziehl-Neelsen staining demonstrates high specificity but is limited by sensitivity, especially in paucibacillary cases. CBNAAT emerges as a promising molecular diagnostic tool with superior sensitivity and specificity, potentially reducing the time to diagnosis. In December 2010, the World Health Organization (WHO) endorsed the use of GeneXpert/CBNAAT as the primary diagnostic test for suspected extrapulmonary tuberculosis (EPTB) cases.
Aims and Objective: To assess the diagnostic effectiveness of three commonly used techniques—Fine Needle Aspiration Cytology (FNAC), Acid-Fast Bacilli (AFB) screening with Ziehl-Neelsen staining, and the Cartridge-Based Nucleic Acid Amplification Test (CBNAAT)—in cases where tubercular lymphadenopathy is suspected.
Materials and Methods: This prospective study was conducted within a hospital setting over a 12-month period, spanning from October 2022 to September 2023. It encompassed all individuals presenting as presumptive cases of tubercular lymphadenopathy and those with purulent aspirates from lymph nodes at various sites. Following fine needle aspiration (FNA), smears were prepared and stained using Haematoxylin and Eosin (H&E), Papanicolaou (PAP), May-Grünwald-Giemsa (MGG), and Ziehl-Neelsen (ZN) techniques. Additionally, samples from all lymphadenopathy cases underwent processing for Cartridge-Based Nucleic Acid Amplification Test (CBNAAT). Statistical analyses were performed using SPSS software version 20.00.
Results: Total number of suspected cases were 107. Majority of aspirates were from cervical region (89.7%) i.e 96 cases from 107. Fnac diagnosis of Tubercular Lymphadenitis was given in 12 cases (11.2%). ZN Stain was positive in 12 cases (11.2%). CBNAAT detected tuberculosis in 32 cases (29.9%), among them 4 cases (3.7%) not detected by FNAC.
Conclusion: While FNA remains the most cost-effective test for diagnosing TB, CBNAAT plays a crucial role in the diagnosis of extrapulmonary tuberculosis (EPTB) in cases featuring granulomatous lymphadenitis and purulent aspirates. Furthermore, CBNAAT provides rapid detection of rifampicin-resistant M. tuberculosis strains, presenting an additional advantage in the diagnostic process.
Introduction
Tubercular lymphadenopathy, a common manifestation of extrapulmonary tuberculosis, poses a diagnostic challenge due to its diverse clinical presentation and the need for prompt identification to initiate timely treatment. Significant progress has been observed in the diagnostic field, where various modalities compete for attention. This study centers on the comparison of three crucial diagnostic methods to offer a thorough assessment in suspected cases of tubercular lymphadenopathy. These methods include Fine Needle Aspiration Cytology (FNAC), Acid-Fast Bacilli (AFB) screening utilizing Ziehl-Neelsen Staining, and the Cartridge-Based Nucleic Acid Amplification Test (CBNAAT).[1]
Fine Needle Aspiration Cytology (FNAC) has been a traditional and widely employed technique for obtaining cellular material from lymph nodes. FNAC offers a minimally invasive means of sample collection, allowing for rapid on-site evaluation and cytological examination. However, its limitations lie in the subjective interpretation of smears and the potential for false negatives, urging a comparative exploration to gauge its efficacy against newer diagnostic modalities.[2]
The utilization of Ziehl-Neelsen Staining for Acid-Fast Bacilli (AFB) screening has been a longstanding cornerstone in tuberculosis diagnosis. This method hinges on identifying acid-fast bacilli in clinical specimens, including lymph node aspirates.[3] Despite its quick results, concerns have been raised regarding the sensitivity and specificity of this method, particularly in cases with low bacillary load. The comparative analysis aims to shed light on its performance relative to contemporary diagnostic alternatives.[4]
The advent of molecular diagnostics has ushered in a new era in tuberculosis diagnosis, with CBNAAT emerging as a powerful tool.[5] The technology combines nucleic acid amplification and real-time PCR, allowing for the simultaneous detection of Mycobacterium tuberculosis and rifampicin resistance. The speed and accuracy of CBNAAT make it an attractive option, but its accessibility and cost implications warrant a critical examination in the context of resource-constrained settings.[6]
The study aimed to compare the diagnostic effectiveness of three frequently used methods: Fine Needle Aspiration Cytology (FNAC), Acid-Fast Bacilli (AFB) screening utilizing Ziehl-Neelsen staining, and the Cartridge-Based Nucleic Acid Amplification Test (CBNAAT) in cases where tubercular lymphadenopathy was suspected.
Materials and Methods
Conducted in a tertiary care hospital in India, this prospective study spanned 12 months from October 2022 to September 2023 and involved a sample size of 107 cases. Approval from the Institutional Ethics Committee was obtained prior to the commencement of the study.
Inclusion criteria
The study encompassed all cases clinically suspected of extrapulmonary tuberculosis (EPTB), including purulent aspirates obtained through fine needle aspiration cytology (FNAC) from various sites, within the age range of 1 year to 65 years.
Exclusion criteria
The study excluded cases that had previously been diagnosed with Cartridge-Based Nucleic Acid Amplification Test (CBNAAT), as well as recurrent and follow-up cases of extrapulmonary tuberculosis (EPTB).
Procedure
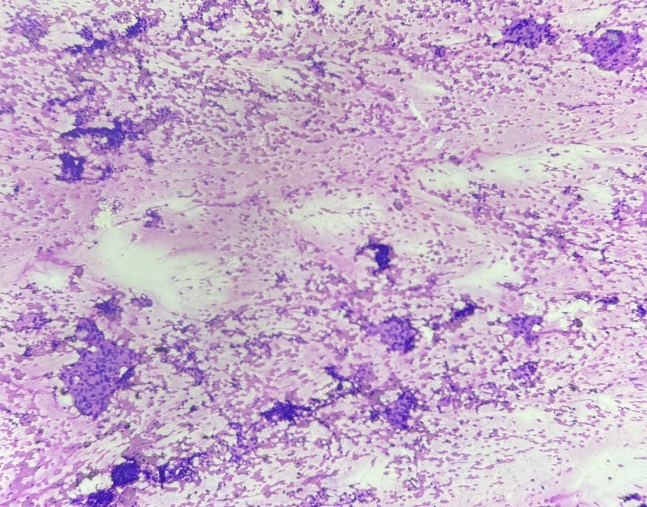
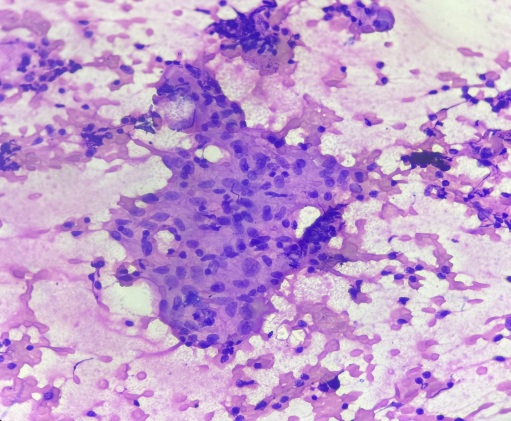
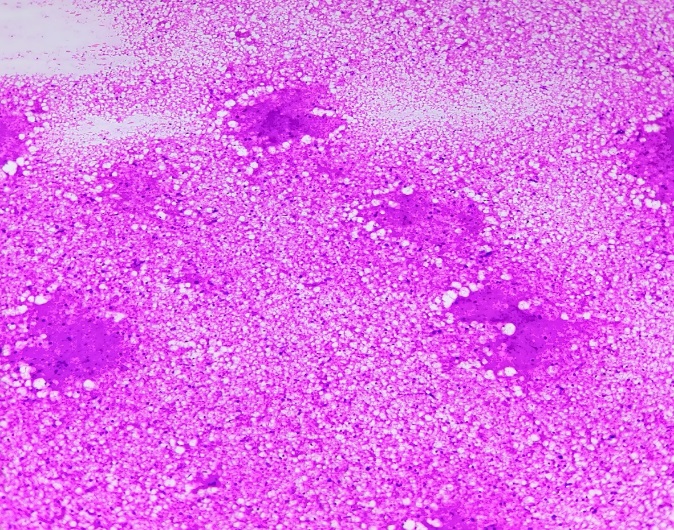
107 cases were selected for study. Detailed FNAC procedure was explained to patient and consent was taken on FNAC requisition form. FNAC of lymph nodes were performed with 24-gauge needle. FNAC material was divided into 2 parts. From first part 4 slides were made, 2 wet fixed slide in 95% alcohol for H and E and Papanicolaou (PAP) stain and 2 slides kept dry which were stained for May Grunwald Giemsa (MGG) and ZN stain.([Figure 1], [Figure 2], [Figure 3])
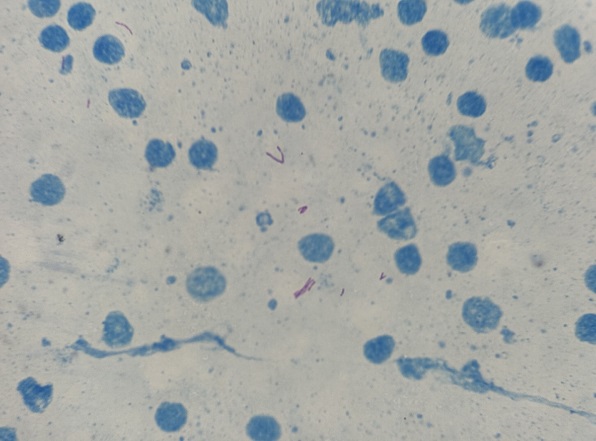
Slides were examined for cytological features and ZN stain observed under oil immersion to look for slender beaded bacilli.([Figure 4])
Second part of the material in needle hub was used for CBNATT testing in falcon tube with 1ml of saline and sample was transferred to TB chest department for CBNAAT testing. CBNAAT performed on GeneXpert machine according to the manufacturer’s instructions. After thoroughly mixing, the FNAC material was combined with sample reagent at a ratio of 2:1 and allowed to stand for 10 minutes at room temperature. Subsequently, it was shaken again and left undisturbed for an additional 5 minutes. Following this process, 2 ml of the material was transferred to the test cartridge, which was then inserted into the test platform. The results were then documented.
Results
In the present study total 107 cases were subjected to FNAC and CBNAAT. Majority of cases are in between age group 21-30 years with male preponderance ([Table 1]).
|
Age group (years) |
No. of cases |
Male |
Female |
|
1-10 |
7 |
4 |
3 |
|
11-20 |
12 |
6 |
6 |
|
21-30 |
26 |
16 |
10 |
|
31-40 |
22 |
12 |
10 |
|
41-50 |
23 |
12 |
11 |
|
51-60 |
11 |
5 |
6 |
|
61-65 |
6 |
2 |
4 |
|
Total |
107 |
57 (53.27%) |
50(46.72%) |
|
Site |
Total |
Percentage (%) |
CBNAAT positive |
|
Submandibular |
07 |
6.5 |
02 |
|
Supraclavicular |
07 |
6.5 |
02 |
|
Jugular |
83 |
77.5 |
25 |
|
Axillary |
6 |
5.6 |
02 |
|
Inguinal |
4 |
3.7 |
01 |
|
Total |
107 |
100 |
32 |
|
Type of aspirate |
Total |
CBNAAT Positive |
CBNAAT Negative |
|
Purulent |
18 (16.8%) |
12 (66.6%) |
6 |
|
Cheesy |
18 (16.8%) |
10 (55.5%) |
8 |
|
Blood mixed |
71 (66.38%) |
10 (14%) |
61 |
|
Total |
107 |
32 (29.9%) |
75(69.1%) |
|
Cytomorphological (FNA) diagnosis |
Total |
CBNAAT+ |
Not correlated with FNAC CBNAAT+/- |
ZN stain for AFB |
|
Granulomatous lymphadenitis |
25(23.3%) |
19(76%) |
6 |
4 |
|
Suppurative lymphadenitis |
14(13%) |
5(35.7%) |
9 |
1 |
|
Necrotising lymphadenitis |
14(13%) |
5(35.7%) |
9 |
2 |
|
Reactive lymphadenitis |
49(45.7%) |
3(6.1%) |
-- |
-- |
|
Metastatic deposits |
05(4.67%) |
-- |
-- |
-- |
|
Total |
107 |
32 |
24 |
7 |
|
Study |
Year of study |
Sensitivity (%) |
Specificity (%) |
|
Present study |
October 2022- September 2023 |
79 |
89 |
|
K arpitha et.al [7] |
July 2019- June 2020 |
80 |
86 |
|
Aruna L et al. [8] |
July 2017- July 2018 |
65 |
92.45 |
|
Komanapalli SK et al. [9] |
April 2017- March 2018 |
84.25 |
86.71 |
|
Patil SB et al. [10] |
Jan 2019- Dec 2019 |
55.5 |
83.80 |
|
Kumar A et al. [11] |
July 2016- July 2017 |
92.7 |
98.9 |
In [Table 2], shows most common site for aspiration was cervical (jugular) (83) followed by submandibular (7) and supraclavicular (7). Out of the 83 cervical cases 25 were CBNAAT positive, submandibular and supraclavicular were 2 cases each positive by CBNAAT.
In [Table 3], shows majority of aspirates were blood mixed i.e 71 (66.38%) out of which 10 were CBNAAT positive. Purulent aspirates were 18 out of which 12 were CBNAAT positive.
Among the 107 cases, cytological features indicative of reactive lymphadenitis were observed in 49 cases (45.7%), with 3 of them testing positive for CBNAAT.([Table 4]) Granulomatous lymphadenitis was identified in 25 cases (23.3%), and 19 of these cases were CBNAAT positive. Additionally, there were 14 cases each of suppurative and necrotizing lymphadenitis. Positive ZN stain for AFB was seen in 4 cases of granulomatous lymphadenitis, 1 of suppurative lymphadenitis and 2 of Necrotising lymphadenitis. So 76% of granulomatous lumphadentitis , 35.7% of Suppurative lymphadenitis, 35.7% of Necrotising lymphadenitis cases were positive for CBNAAT. 6.1% OF Reactive lymphadenitis cases were positive for CBNAAT. Diagnostic performance of the CBNAAT versus FNAC (32/107) showed sensitivity, specificity, positive predictive value and negative predictive value of 79%, 89.84%, 63% and 47.5%, respectively.
Discussion
Tuberculous lymphadenitis is one of the most common sites for extra pulmonary tuberculosis. Early diagnosis and optimal treatment will not only completely cure the patient but will also curb the transmission of infection and disease within the community. The United Nations Sustainable Development Goals aim to end the tuberculosis epidemic by 2030, as outlined in the 2019 WHO guidelines for TB, and this objective is considered attainable. [9]
As per the World Health Organization's report, the incidence of tuberculosis in India is decreasing. This serves as evidence that substantial progress against tuberculosis can be achieved rapidly, even in the largest and most geographically diverse nations worldwide. [12]
This current investigation is a prospective hospital-based study evaluating the diagnosis of suspected tubercular lymphadenopathy using CBNAAT compared to FNAC. In the current diagnostic context, FNAC plays a pivotal role in disease identification. Functioning as a cost-effective and minimally invasive outpatient procedure, FNAC has evolved into a routine and indispensable method for diagnosing extrapulmonary tuberculosis in contemporary healthcare practices. [13]
In present study cervical lymph node swellings formed majority of cases. Age group 21-30 had more cases affected by Tuberculosis and male preponderance was seen which is corelated with other studies done by Komanapalli SK et al., Rock RB et al., and Tadesse M et al. [13], [8], [10]
This study additionally examined the distribution of the type of FNAC aspirate in conjunction with the CBNAAT result, revealing a lack of correlation with the findings of Tadesse M et al. [10] In their study, caseous aspirates exhibited higher CBNAAT positivity at 69%, whereas the present study demonstrated a 66.66% positivity rate for purulent aspirates.([Table 3]) This aligns with the results observed in the study conducted by Komanapalli SK et al. [13]
In this investigation, the significance of CBNAAT is highlighted in identifying TB patients who initially tested cytologically negative for TB. CBNAAT proved advantageous for a total of 13 cases initially classified as cytologically negative, subsequently revealing a positive status through CBNAAT.
On comparison of CBNAAT diagnostic performance of present study (sensitivity 79%, specificity 89%) with Aruna L et al.,[11] (sensitivity-65%, specificity 92.45%), Komanapalli SK et al. [13], (sensitivity 84.25%, specificity 86.71%) Patil SB et al., [7] (sensitivity 55.5%, specificity 83.80%), Kumar A et al., [14] (sensitivity-92.7%, specificity 98.9%) and K arpitha et. al.[15] showed less sensitivity and more specificity.
Hence, FNAC deserves inclusion as the initial diagnostic investigation, and a comparative analysis with CBNAAT is recommended to enhance result accuracy. This approach aims to minimize the likelihood of overlooking cases that may be missed when relying solely on CBNAAT or FNAC independently.
Conclusion
CBNAAT demonstrated its utility in 10 cases initially diagnosed as cytologically negative but later confirmed as positive through CBNAAT. CBNAAT exhibits higher specificity in detecting extrapulmonary TB compared to FNAC. While FNAC proves to be cost-effective in diagnosing extrapulmonary tuberculosis (specifically suspected tubercular lymphadenopathy), combining it with CBNAAT offers the advantage of identifying cases missed by FNAC. Moreover, CBNAAT is a rapid test with high specificity, enhancing the overall diagnostic capabilities.
Source of Funding
None.
Conflict of Interest
None.
References
- . Tuberculosis. World Health Organization. 2018. [Google Scholar]
- Koo V, Lioe T, Spence R. Fine needle aspiration cytology (FNAC) in the diagnosis of granulomatous lymphadenitis. Ulster Med J. 2006;75(1):59-64. [Google Scholar]
- Nigussie M, Mamo G. Detection of acid fast bacilli (AFB) in tuberculous lymphadenitis among adult Ethiopians. Ethiop Med J. 2010;48(4):277-83. [Google Scholar]
- Purohit M, Mustafa T, Wiker HG, Mørkve O, Sviland L. Immunohistochemical diagnosis of abdominal and lymph node tuberculosis by detecting Mycobacterium tuberculosis complex specific antigen MPT64. Diagn Pathol. 2013;2. [Google Scholar] [Crossref]
- Maclean E, Kohli M, Weber S, Suresh A, Schumacher S, Denkinger C. Advances in Molecular Diagnosis of Tuberculosis. J Clin Microbiol. 2020;58(10). [Google Scholar] [Crossref]
- Boehme C, Nicol M, Nabeta P, Michael J, Gotuzzo E, Tahirli R. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet. 2011;377(9776):1495-505. [Google Scholar]
- Patil S, Dhage S, Umap P, Ghorpade S, Patharwat S. Cartridge based nucleic acid amplification test: A sensitive diagnostic tool for tuberculosis on fine needle aspirates samples. Int J Community Med Public Health. 2020;7(4):1511-5. [Google Scholar]
- Tadesse M, Abebe G, Abdissa K, Aragaw D, Abdella K, Bekele A. GeneXpert MTB/RIF Assay for the Diagnosis of Tuberculous Lymphadenitis on Concentrated Fine Needle Aspirates in High Tuberculosis Burden Settings. PLoS One. 2015;10(9). [Google Scholar] [Crossref]
- Aruna L, Ghanshyani K, Lakshmi E, Magar L. Correlation of cytomorphology and cartridge based nucleic acid amplification test (CBNAAT) on fine needle aspirates in the diagnosis of tuberculous lymphadenitis. Med Pulse Int J Pathol. 2018;7(3):128-32. [Google Scholar]
- Jayakumar P, Kaushal M, Duggal N. Comparison of CBNAAT and AFB screening using Ziehl Neelsen stain and fluorescent stain on FNAC sample for rapid diagnosis of tubercular lymphadenitis. Indian J Pathol Oncol. 2023;10(3):249-58. [Google Scholar]
- Rock R, Sutherland W, Baker C, Williams D. Extrapulmonary tuberculosis among Somalis in Minnesota. Emerg Infect Dis. 2006;12(9):1434-6. [Google Scholar]
- Dhote AR, Gaikwad A, Datar S, Kowe B. Utility of cartridge based nucleic acid amplification test in diagnosis of tubercular lymph nodes on fine needle aspiration and its comparison with zeihl-neelsen staining and concentration bleach method. Panacea J Med Sci. 2022;12(1):61-6. [Google Scholar]
- Komanapalli SK, Prasad U, Atla B, Vasundhara N, Yendluri D. Role of CB-NAAT in diagnosing extra pulmonary tuberculosis in correlation with FNA in a tertiary care center. Int J Res Med Sci. 2018;6(12):4039-45. [Google Scholar]
- Kumar A, Das S, Paul D. A study on the role of Cartridge Based Nucleic Acid Amplification Test (CBNAAT) for diagnosing pediatric tuberculosis in a tertiary care hospital in Eastern India. Acad J Ped Neonatol. 2018;6(3):52-8. [Google Scholar]
- Arpitha K, Kumar M, Sirasagi A, Pattar P. Comparison of Fine Needle Aspiration Cytology, Ziehl-Neelsen Staining and GeneXpert Methods in Suspected Cases of Tubercular Lymphadenopathy. National J Lab Med. 2021;10(3):26-9. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.131-136
-
CrossMark
- Citation
- Received Date January 28, 2024
- Accepted Date July 01, 2024
- Publication Date March 12, 2025