Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Estimation of cord blood TSH level in a tertiary care hospital in Uttarakhand
Abstract
Introduction: Thyroid hormone is essential for growth and responsible for development of the brain. Congenital Hypothyroidism, which is defined as deficiency of thyroid hormone, is the commonest cause of the preventable mental retardation among children. In the general population, screening for congenital hypothyroidism remains one of the most cost-effective tools to prevent mental retardation.
Aims and Objective: To estimate the Thyroid Stimulating Hormone level in the birth canal (cord blood) of early neonates.
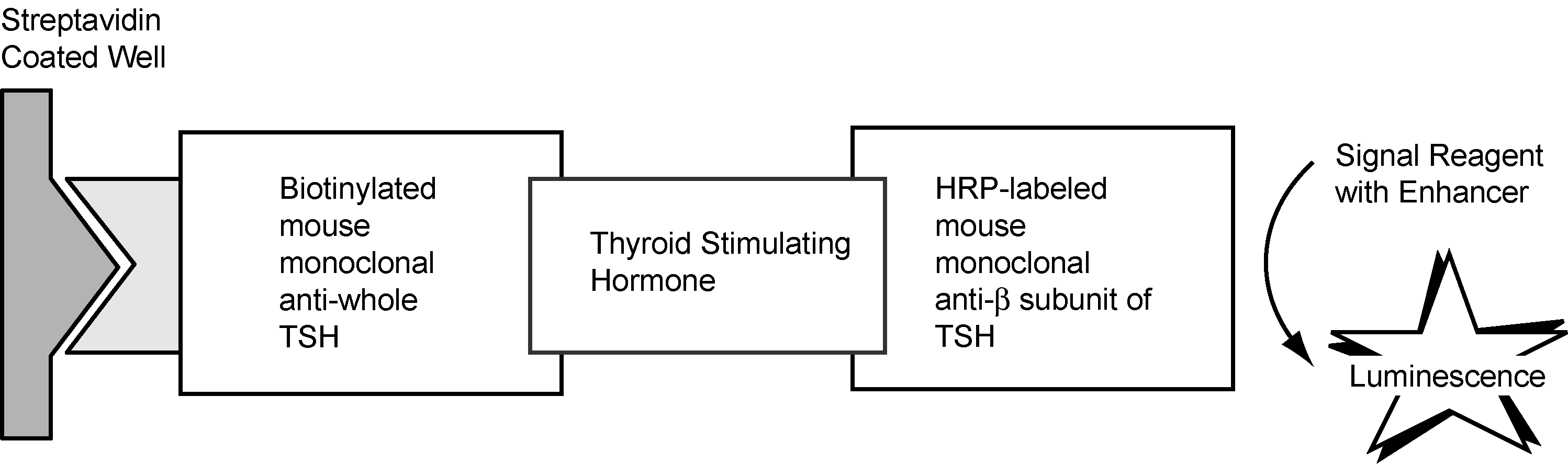
Materials and Methods: A Prospective observational study was conducted over a period of six month from January to July 2018 at Shri Guru Ram Rai Institute of Medical & Health Sciences, Dehradun. The study group comprising the 303 neonates irrespective of gender, neonates of the Diabetic mothers, eclampsia, and hypertensive mothers were excluded. Serum sample extracted from cord blood was utilized for the estimation of the TSH by processing in the dry chemistry analyzer of Ortho-clinical diagnostics VITROS 5600.
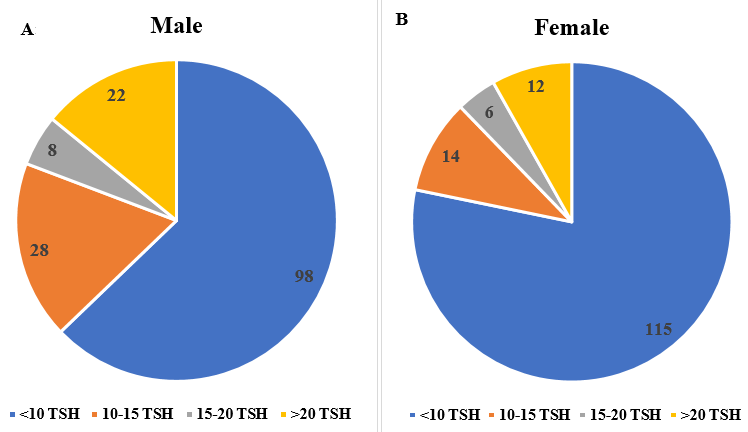
Result: It was found that the female neonates are less prone to have congenital hypothyroidism, with having TSH levels of <10 mIU/ml in about 80% of samples while on the other hand males are having TSH levels of <10 mIU/ml in about 62% of samples.
Conclusion: We concluded that the male neonates prone to have Congenital Hypothyroidism more.
Introduction
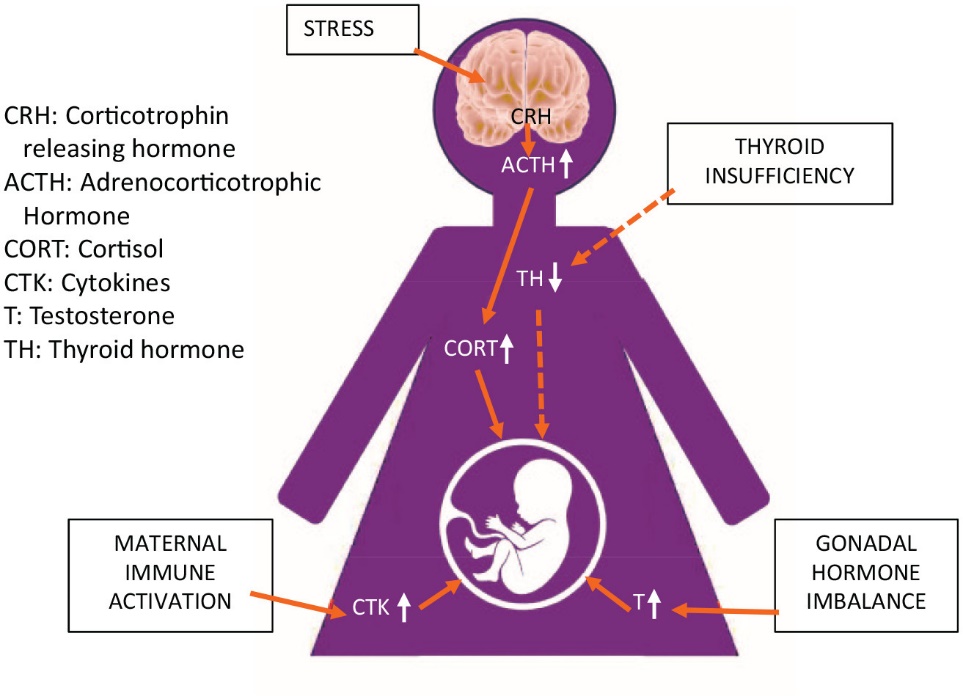
Thyroid hormone is essential for growth and play an important role in developing brain. The commonest cause of preventable mental retardation is deficiency of thyroid hormone at birth i.e. congenital hypothyroidism. It is also difficult to diagnose congenital hypothyroidism based on the clinical symptoms alone at birth. [1] In India, a multicentric attempt has been made to screen neonates in 2007 by ICMR, but national programme does not exist till date, and also there is not any uniform method for screening of the disorder. [2] It has an incidence of 1 in 4000 births in various neonatal screening programs. Umbilical cord blood thyroid‑stimulating hormone (TSH) levels remain an ubiquitous, simple and a practical test for screening of congenital hypothyroidism. [3] Also, the data regarding the neonatal cord blood TSH levels are very scars so we plan to conduct this study for utilization of cord blood TSH as a marker for screening of congenital hypothyroidism. Maternal stress during the gestation period can lead to congenital Hypothyroidism. [4]
Materials and Methods
A Prospective observational study was conducted over a period of six month from January to July 2018 at SGRRIM&HS Dehradun, Uttarakhand. The study group comprising 303 neonates irrespective of gender. After taking informed written consent, 5 ml cord blood sample was collected in the serum separated tube (SST) and SST was collected at the Clinical Biochemistry Laboratory. The SST was centrifuged, and separated serum was utilized for the estimation of the TSH by processing in the dry chemistry fully automated analyzer of Ortho-clinical diagnostics VITROS 5600. The neonates of the diabetic mothers, eclampsia, and hypertensive mothers were excluded from the study group. As no direct intervention was involved to the mother as well as to the neonate so the ethical waiver is granted for this study.
Result
Out of 303 neonates 147 (48.52%) were Females and 156 (51.48%) were males. Out of 147 females, 12 (8.16%) females were having the TSH levels of > 20 mIU/ml, 6 (4.09%) females were in the range of 15-20 mIU/ml, 14 (9.52%) were in the range of 10-15 mIU/ml and 115 (78.23%) females were having TSH value of less than 10 mIU/ml. Out of 156 male 22 (14.10%) males were having the TSH levels of > 20 mIU/ml, 8 (5.12%) were in the range of 15-20 mIU/ml, and 28 (17.94%) were in the range of 10-15 mIU/ml, and 98 (62.825%) were having TSH value of less than 10 mIU/ml. The results are represented graphically in the pie charts [Figure 3] A (Frequency of Male) and [Figure 3] B (Frequency of Female).
Discussion
In the Indian context, approximately 70-80% of mothers are discharged within 48 hours post-delivery, which poses a significant obstacle to early neonatal screening. In contrast to developed countries where health workers conduct primary newborn screenings, the sheer size of the population and the strain on the healthcare system in India make such home-based sample collection challenging. Consequently, post-discharge screening relies on parents to bring their seemingly healthy newborns back to the hospital for blood tests, a logistical challenge compounded by the difficulty in recalling neonates for screening within the first few days after delivery. As a result, cord blood TSH investigation stands out as an accessible and effective method for screening congenital hypothyroidism. Global studies have consistently demonstrated the efficacy of cord blood in screening. However, despite its potential, nationwide implementation in India has been hampered by various factors including inadequate facilities, limited awareness among healthcare providers, financial constraints, and the trend of early neonatal discharge. While India initiated universal salt iodization in 1992 as part of the National Iodine Deficiency Control Program, there remains a dearth of institutional data on maternal iodine status, despite the widespread use of iodized salt among the population. In our investigation, a significant proportion of neonates were discharged within the second- or third-day following delivery, even though some exhibited TSH levels exceeding 15 mIU/ml. Additionally, patient compliance was notably low, leading to inadequate follow-up visits. Interestingly, there was a tendency among caregivers to be more protective of male neonates, sometimes resulting in reluctance to continue treatment. Globally, a TSH cutoff of 20mIU/L in cord blood is commonly employed, which was consistent with our approach. Our findings revealed that 10% of samples exhibited cord blood TSH levels surpassing 10 mIU/L, albeit slightly higher than findings reported by Mekennon et al. and Manglik et al.[5], [6] Our investigation revealed that 11.22% of all samples exhibited values exceeding 20 μIU/mL, a finding consistent with the study conducted by Garg et al.[7] Based on the mode of delivery, our study found that newborns delivered via elective Caesarean Section exhibited notably lower mean levels of cord blood TSH compared to those delivered vaginally or via emergency LSCS (lower segment Caesarean section).[8], [9] This raises a new inquiry about the preference between caesarean section and normal vaginal delivery. In our investigation, male newborns demonstrated significantly elevated levels of cord blood TSH compared to female neonates. Similar findings have been documented by Gupta A et al. and Ryckmann KK et al.[10], [11]
The use of heel-blood TSH has been implemented to enhance the detection of moderate and mild cases of congenital hypothyroidism beyond the 24-hour mark post-delivery. Programs employing heel-blood samples have effectively achieved this objective by reducing cutoff values from 20 to 10–12 mIU/L TSH. [12], [13], [14] In a comparable investigation conducted by Jillela MR et al., 263 neonates, regardless of birth weight and gestational age, underwent testing for cord blood TSH levels at the Chalmeda Anand Rao Institute of Medical Sciences over a span of 2 years. Their findings indicated that cord blood TSH levels surpassing the cutoff value of 20 mIU/L served as a robust predictor for Congenital Hypothyroidism. [15]
Conclusion
We concluded that the Cord blood TSH is an effective and easy tool for the screening of the Congenital Hypothyroidism and the male neonates are more prone to have the congenital hypothyroidism as compared with the female neonates. We can safely use a cutoff of cord blood TSH value of >20 mIU/L for screening for congenital hypothyroidism.
Limitation of Study
The study is confined to Uttarakhand region only, multicentric studies with large cohort are needed to bring more light on this preventable cause of mental retardation.
Conflicts of Interest
None.
Source of Funding
There is not any source of funding involved for this research work.
References
- Grosse S, Vliet G. Prevention of intellectual disability through screening for congenital hypothyroidism: how much and at what level?. Arch Dis Child. 2011;96(4):374-9. [Google Scholar]
- Dutta R. ICMR to conduct first nationwide newborn screening for genetic disorders. Express Health Care Management. 1st. . 2005. [Google Scholar]
- Bhatia R, Rajwaniya D. Congenital Hypothyroidism Screening in Term Neonates using Umbilical Cord Blood TSH Values. Indian J Endocr Metab. 2018;22(2):277-9. [Google Scholar]
- Wilson H, Creighton C, Scharfman H, Choleris E, Maclusky N. Endocrine Insights into the Pathophysiology of Autism Spectrum Disorder. Neuroscientist. 2021;27(6):650-67. [Google Scholar]
- Manglik A, Chatterjee N, Ghosh G. Umbilical cord blood TSH levels in term neonates: a screening tool for congenital hypothyroidism. Indian Pediatr. 2005;42(10):1029-32. [Google Scholar]
- Mekennon Y, Gizachew W, Chamiso B, Raue F. Thyroid Stimulating Hormone values from cord blood in neonates. Ethiop J Health Dev. 2003;17(2):125-30. [Google Scholar]
- Garg M, Kumar P, Abirami S, Manikandan M, Krishnan L. Perinatal variables influencing cord blood thyroid stimulating hormone. Int J Contemp Pediatr. 2018;5(4):1537-41. [Google Scholar]
- Rico A, Prieto-Lloret J, Gonzalez C, Rigual R. Hypoxia and acidosis increase the secretion of catecholamines in the neonatal rat adrenal medulla: an in vitro study. Am J Physiol Cell Physiol. 2005;289(6):1417-25. [Google Scholar]
- Gülmezoglu A, Mahomed K, Hofmeyr G, Nikodem V, Kramer T. Fetal and maternal catecholamine levels at delivery. J Perinat Med. 1996;24(6):687-91. [Google Scholar]
- Gupta A, Srivastava S, Bhatnagar A. Cord blood thyroid stimulating hormone level - Interpretation in light of perinatal factors. Indian Pediatr. 2014;51(1):32-6. [Google Scholar]
- Ryckman K, Spracklen C, Dagle J, Murray J. Maternal factors and complications of preterm birth associated with neonatal thyroid stimulating hormone. J Pediatr Endocrinol Metab. 2014;27(9-10):929-38. [Google Scholar]
- Ford G, Lafranchi S. Screening for congenital hypothyroidism: A worldwide view of strategies. Best Pract Res Clin Endocrinol Metab. 2014;28(2):175-87. [Google Scholar]
- Botler J, Camacho LB, Cruz M. Phenylketonuria, congenital hypothyroidism and haemoglobinopathies: public health issues for a Brazilian newborn screening program. Cad Saude Publica. 2012;28(9):1623-31. [Google Scholar]
- Corbetta C, Weber G, Cortinovis F, Calebiro D, Passoni A, Vigone M. A 7-year experience with low blood TSH cutoff levels for neonatal screening reveals an unsuspected frequency of congenital hypothyroidism (CH). Clin Endocrinol (Oxf). 2009;71(5):739-45. [Google Scholar]
- Jillela M, Keshireddy P, Goli S, Chiluka A, Chitgope R. Umbilical cord blood TSH level: correlation with congenital hypothyroidism. Int J Contemp Pediatr. 2021;8(7):1204-8. [Google Scholar]
Article Metrics
- Visibility 10 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.148-151
-
CrossMark
- Citation
- Received Date January 26, 2024
- Accepted Date July 23, 2024
- Publication Date March 12, 2025