Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Bacteria on white coats of medical students: A cross-sectional study
Abstract
Background: To evaluate the danger of transmission of pathogenic organisms via the white coats of medical students in college. It is important to determine the degree and kind of microbial contamination that was present on white coats. This study also looked into how the students handled and cleaned their coats as well as what were their perceptions about contamination through white coats.
Materials and Methods: This was a cross-sectional study carried out at the NCRIMS, Meerut from August 2022 to September 2022. 176 white coats worn by medical students in total were sampled for potential contamination by bacteria.
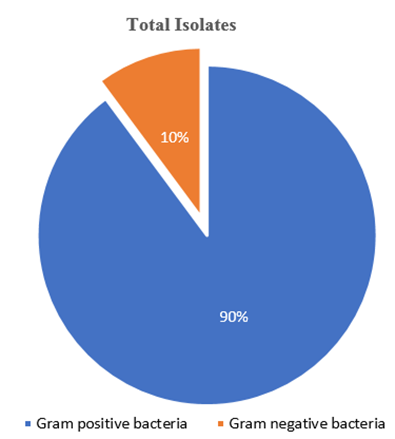
Result: 67.04% of the 176 white coats that were screened were found to be contaminated. Major contaminants were Gram-positive bacteria (89.83% of the contaminated coats) while only 10.16% were Gram-negative bacteria. The perception of medical students towards the spread of nosocomial infections through white coats was also studied which reflected a poor hygienic practice regarding their white coats.
Conclusion: The following recommendations may be made on the basis of this study. First, it should become mandatory to purchase white coats on an annual basis and to always have two or more on hand. Whitecoat wearers should be urged to wash their white coats on a weekly basis. This study offers microbiological proof in favour of barring white coats from non-clinical areas of the hospital.
Introduction
Most of the hospital-acquired infections are mainly contributed by the hospital environment. Many reports have been published to show the relationship between the organism found at site of infection and hospital environment.[1] Clinical white coats that are routinely wear by medical professionals is a symbol of healing and concern to the patient and important for doctor patient relationship is also a matter of concern as they can also play a role of vehicle in hospital-acquired infections both in and outside the hospital. [2]
According to an estimate it is found that about 1.4 million people all over the world suffer from hospital-acquired infections. [3] Although we usually follow strict infection control measures, even though we unknowingly bear microorganism on our white coats. [2]
Over past two decades use of white coat in the hospital setting has been decreased due to awareness regarding its role in transmitting hospital-acquired infections. [4],[5] Medical colleges are attached to hospitals and medical students usually carry their white coats to hospital, lecture theatre, practical classes of pre and paraclinical, cafeteria, library and in the common room of the college. It is very common to see students carrying white coats outside hospital premises. [6] Physicians often touch white coat during their working hour and a lack of hand hygiene habit definitely enhance white coat contamination. [7]
Our study was done to find out the prevalence of white coats contamination among medical students. In this study we also want know the prevalence of different bacteria by their identification and also their sensitivity pattern. We also study the perception of cleaning and handling of white coat among students with the help of a form with different questionnaire.
This study was conducted to find the level and type of microbial contamination on the white coats of medical students in order to assess the risk of transmission of pathogenic microorganisms by this route in a hospital setting. The student’s way of handling the coats and cleaning them, as well as their perception of white coat contamination also were investigated.
Materials and Methods
Specimens were collected from medical students by normal saline moistened cotton swabs by gently rotating it on cuffs and lower edge of white coats. After labelling the swab with name and age of medical students, swabs were send to the Microbiology laboratory of NCRIMS Meerut. Swabs were inoculated on Blood and MacConkey agar and incubated at 37°C for 24 hours.
After 24 hrs of incubation, if there is growth on culture media it was confirmed by colony morphology and gram-staining. Biochemical reactions (Catalase,MR, VP, Oxidase, Indole, Urease, TSI, Citrate, etc.) and according to CLSI guidelines Antibiotic sensitivity testing was performed. [8], [9]
At the same time, a consent form and questionnaire paper were filled out by the person from whom the swab was collected regarding, the usage of white coat, hygiene, purpose, and about students perception about the of contamination of white coats, etc.
Results
There were 176 samples in all, 92 of which were male and 84 of which were female. The majority of them, 127 (72.15%) were paraclinical students, followed by 43 (24.43%) clinical students and 6 (3.40%) preclinical students.
White coats are typically worn to seem professional by 131 subjects (74.43%) and to cover clothing 36 (20.45%), according to the majority of students. A few students used white coats for the usage of pockets 4 (2.27%), 3 (1.70%) to prevent oneself from contamination, 1 (0.56%) student used their white coats to make themselves realize of their duty & ethics & only 1 student (0.56%) for serving the society.However, only 6 of the subjects (3%) utilised their white coats within the hospital only, while the majority of them 162 (92.04%) used them in both hospital & college. Only 7 students (3.9%) used their white coats only during college & 1 (0.56%) used their white coats at other places also. Although both clinical and non-clinical students were very aware of the potential for white coat contamination, they continued to wear them in a variety of college settings, including the library, reading rooms, canteen, classes, and even outside the hospital grounds when it was not essential. By providing students with changing facilities on the hospital grounds, it's possible to decrease the amount of time they spend wearing white coats in classrooms and other non-clinical settings. Also restricting usage of white coats at non-clinical settings helps to prevent the spread of nosocomial infections.
In our study majority, 170 coats (96.5%) were full sleeves & only 6 (3.4%) coats were half sleeves. We during our study found that majority students (127 (72.15%) are in possession of 2 white coats, 30 students (17.04%) possessed 3 coats & 10.22% which is 18 subjects even owned 3 white coats which is satisfying. According to the statistics, ideally, 3 (or minimum 2) white coats should be possessed by every health care provider in the view that they can be laundered effectively.
143 students (81.25%) out of the study claimed that they used hand disinfectants regularly whereas 33 (19%) refused to use hand disinfectants regularly.
Out of all the 176 samples collected from students,118 students (67.04%) while the coats found to be contaminated by different organisms and of 58 students (32.95%) were found to be non-contaminated. Among 118 contaminated white coats most common organism isolated were gram positive among which most of were coagulase negative staphylococcus (92). Antibiotic sensitivity was performed by Kirby-Bauer disk diffusion susceptibility testingas per the CLSI guidelines.
|
Surveyed Variables |
Number of Students (N = 176) |
% |
|
Gender |
||
|
Male |
92 |
52.20% |
|
Female |
84 |
47.72% |
|
Current Working Location |
||
|
Preclinical |
6 |
3.40% |
|
Paraclinical |
127 |
72.15% |
|
Clinical |
43 |
24.43% |
|
The Reason for Wearing the White Coat |
||
|
To Cover Clothing |
36 |
20.45% |
|
To Appear Professional, The Dress Code of The Hospital |
131 |
74.43% |
|
For The Usage Of Pockets |
4 |
2.27% |
|
To Prevent OnselfFrom Contamination |
3 |
1.70% |
|
To Serve the Society |
1 |
0.56% |
|
To Make Myself Realise of My Duty & Ethics |
1 |
0.56% |
|
The Usage of Coats |
||
|
<1 Yr |
33 |
18.75% |
|
1-2 Yr |
85 |
48.29% |
|
2-3 Yr |
1 |
0.56% |
|
>3 Yr |
57 |
32.38% |
|
When The Coat Was Last Washed |
||
|
<3 Days |
138 |
78.84% |
|
1 Week |
35 |
19.88% |
|
2-4 Weeks |
3 |
1.70% |
|
>1 Month |
0 |
0.00% |
|
Type of Cleaning |
||
|
Home |
29 |
16.40% |
|
Laundry |
147 |
83.50% |
|
Type of White Coat |
||
|
Half- Sleeves |
6 |
3.40% |
|
Full- Sleeves |
170 |
96.50% |
|
Method of Carrying White Coat |
||
|
Cover |
35 |
19.88% |
|
Bags |
29 |
16.40% |
|
Hands |
99 |
56.25% |
|
Shoulders |
13 |
7.38% |
|
How Frequently White Coats Are Used |
||
|
Only Hospital |
6 |
3.00% |
|
Only College |
7 |
3.90% |
|
Hospital & College |
162 |
92.04% |
|
Other Places |
1 |
0.56% |
|
Duration of Usage Per Day |
||
|
4 Hours |
16 |
9.09% |
|
4-8 Hours |
131 |
74.43% |
|
>8 Hours |
129 |
16.40% |
|
Number of White Coats Possessed |
||
|
1 Coat |
1 |
0.56% |
|
2 Coats |
127 |
72.15% |
|
3 Coats |
30 |
17.04% |
|
>3 Coats |
18 |
10.22% |
|
Use of Hand Disinfectant Regularly |
||
|
Yes |
143 |
81.25% |
|
No |
33 |
18.75% |
|
Exchanged White Coats with Colleagues |
||
|
Yes |
39 |
22.15% |
|
No |
137 |
77.85% |
|
Left Their White Coats at Hospitals |
||
|
Yes |
15 |
8.52% |
|
No |
161 |
91.40% |
|
Washing Hand After Removing White Coats |
||
|
Yes |
99 |
56.25% |
|
No |
77 |
43.75% |
|
Stain Present Over White Coat |
||
|
Yes |
58 |
32.90% |
|
No |
118 |
67.04% |
|
Do You Think Your White Coat Carries Germs |
||
|
Yes |
81 |
46.02% |
|
No |
16 |
9.09% |
|
Maybe |
79 |
44.88% |
|
Organisms Isolated |
Number of Contaminated Coats (N=118) |
% |
|
Coagulase Negative Staphylococci |
92 |
77.96% |
|
Staphylococcus aureus |
14 |
11.86% |
|
E. coli |
8 |
6.77% |
|
Klebsiella |
1 |
0.84% |
|
Acinetobacter |
1 |
0.84% |
|
Pseudomonas |
2 |
1.69% |
|
S.No |
Antibiotic |
Resistant |
|
Gram positive bacteria N= 106 (89.8%) |
||
|
1. |
Cefoxitin |
23 (21.7%) |
|
2. |
Ceftriaxone |
23 (21.7%) |
|
3. |
Erythromycin |
23 (21.7%) |
|
4. |
Azithromycin |
23 (21.7%) |
|
5. |
Clindamycin |
3 (2.8%) |
|
6. |
Levofloxacin |
12 (11.3%) |
|
7. |
Ciprofloxacin |
12 (11.3%) |
|
8. |
Imipenem |
0 |
|
9. |
Meropenem |
0 |
|
10. |
Teicoplanin |
3 (2.8%) |
|
11. |
Vancomycin |
0 |
|
12. |
Linezolid |
0 |
|
Gram Negative bacteria N= 12 (10.16%) |
||
|
1. |
Ceftriaxone |
8 (66.6%) |
|
2. |
Cefoperazone |
8 (66.6%) |
|
3. |
Gentamycin |
1 (8.3%) |
|
4. |
Amikacin |
1 (8.3%) |
|
5. |
Levofloxacin |
6 (50%) |
|
6. |
Ciprofloxacin |
6 (50%) |
|
7. |
Imipenem |
0 |
|
8. |
Meropenem |
0 |
|
9. |
Cefoperazone + Sulbactam |
2 (16.6%) |
|
10. |
Piperacillin/Tazobactam |
2(16.6%) |
|
11. |
Tigecycline |
0 |
|
12. |
Colistin |
0 |
Discussion
The following two facts could explain the high rates of bacterial contamination of white coats: First of all, patients constantly discharge infectious microbes into the hospital setting, and medical professionals frequently come into contact with these individuals. Second, it has been shown that bacteria can survive on fabrics used to produce white coats, such as cotton, cotton and polyester, or polyester materials, for a period of 10 to 98 days. [10], [11]
Since white coats play a crucial role in the transmission of nosocomial infections, we examined 176 medical students. Out of the 176 white coats, 92 (52.2%) belonged to the male participants, while 84 (47.72%) belonged to the female subjects. Males had more contaminated white coats than females, according to a research by Muhadi et al., although there was no statistically significant difference in contamination between the two groups. [6]
The white coats of the medical students laundered by hostel laundry tended to be more polluted, but those living off-campus had less infected coats. These results were like the study of Treakle et al & Srinivasan A et al.. [12], [13] 81 (46.02%) of the individuals knew that even though they thought their white jackets were spotless and free of stains, they could serve as a vehicle for the spread of pathogenic organisms from the hospital. Most of the students 138 (78.4%) had washed their white coats in less than 3 days, 35 (19.88%) washed their coat once in a week & also 3 subjects (1.70%) had washed it for 2-4 weeks according to statistics on the students' cleaning habits. Despite this, and despite the time since the last wash, the contamination was substantial, 118 students (67.04%) while the coats of 58 students (32.95%) were found to be non-contaminated. This was in line with research done at Kilimanjaro Christian Medical Centre, Moshi, Tanzania by Josephat Qaday et al. [14]
The contamination of white coats is significantly influenced by the movement of white coats from their site of residence. In our survey, 13 students (7.38%) carried their white coats on their shoulders, 99 (56.25%) carried them in hands, and 29 (16.4%) kept their coats within their bags, which is a significant and hygienic method of transporting white coats from the residential location. Students who wear coats over their shoulders are thought to be significantly more contaminated than the others as founded in a study by Sandeep Samsan et al. [2]
Coagulase negative Staphylococci, which are skin commensals, was the main pathogen that was isolated in the current study, 118 subjects (67.7%), which is comparable to the findings of studies by Muhadi et al., [6] Treakle et al.,[12] and Wong et al. [15]
Staphylococci, which are Gram positive bacteria and may be infectious to patients who are admitted to the hospital, were also isolated in 14 subjects (7.95%). Joseph Qaday et al in his study reported that Staphylococcus was the major organism isolated. [14]
Out of which 14 infected form Staphylococcus 6 were MRSA & 8 were MSSA. 8 coats (4.54%) were found to be contaminated with E-coli, 1 infected with Kleibsella, 1 Acinetobacter & 2 were found to be infected with Psuedomonas.
Sandeep Samsan. N et al reported that the prevalence of E. coli was 13% & that of Kleibsella as 4 % which is much higher than what we observed during our study. [2]
A number of past investigations had shown that all healthcare workers, including doctors, had low adherence to the hand-hygiene standards.[10] Also 99 subjects (56.25%) were aware & believed in hand washing after removing their coats, still 77 (43.75%) were not in the practice of hand washing after removing coats which is an alarming number and pose increasing risk of transmission of pathogenic organisms in the community. Health professionals at some institutions did not follow hand hygiene practices as well as they should have, according to a research by Harris AD et al. [16]
Conclusion
According to this study, a significant number of white coats worn by medical and paramedical students are infected with microorganisms, including gram-negative pathogenic pathogens. In tertiary hospitals, white coats take over as the main means of spreading illnesses from students-patients-students. This is due to the inappropriate hygiene practises that we previously highlighted in this study as well as the use of white coats outside of clinical settings. Students should be taught the significance of white coats and the reason for which they are used, as well as how to use them properly and to refrain from wearing them outside of clinical settings, in order to prevent contamination and the spread of infection from students to patients. This study demonstrates that the white coat harbours various harmful bacteria and is a key factor in the spread of diseases in a hospital setting. It is crucial because once these factors are understood, suitable policies can be put in place. By possibly lowering nosocomial infections, proper white coat handling by medical students as well as other healthcare professionals could reduce cross-contamination and enhance patient safety.
Acknowledgement
The study was originally done as a part of the Indian Council of Medical Research-Short Term Studentship (ICMR-STS) programmed in 2022 (06082), and was approved by ICMR.
Source of Funding
None.
Conflicts of Interest
The authors have no financial interests or conflicts of interests.
References
- Atata R, Ibrahim Y, Olurinola P, Giwa A, Akanbi-II A, Sani A. Clinical bacterial isolates from hospital environment as agents of surgical wound nosocomial infections. J Pharm Bio Res. 2010;7(2):146-55. [Google Scholar]
- Sandeep S, Kumaran G, Naziyagulnaaz A. A Survey of White Coat Hygiene among the Medical Students and Paramedical Students in a Tertiary Health Care Hospital. Ann Rom Soc Cell Biol. 2021;25(4):3631-42. [Google Scholar]
- Mwamungule S, Chimana H, Malama S, Mainda G, Kwenda G, Muma J. Contamination of health care workers' coats at the University Teaching Hospital in Lusaka, Zambia: the nosocomial risk. J Occup Med Toxicol. 2015;10. [Google Scholar] [Crossref]
- Harnett P. Should Medical students Wear White Coats?. Med J Aust. 2001;174(7):343-4. [Google Scholar]
- Douse J, Derrett-Smith E, Dheda K, Dilworth J. Should doctors wear white coats?. Postgrad Med J. 2004;80(943):284-6. [Google Scholar]
- Muhadi S, Aznamshah N, Jahanfar S. A cross sectional study on the microbial contamination of the medical student’s white coats. Malayasian J Microbiol. 2007;3(1):35-8. [Google Scholar]
- Banu A, Anand M, Nagi N. White coats as a vehicle for bacterial dissemination. J Clin Diagn Res. 2012;6(8):1381-4. [Google Scholar]
- Koneman E, Allen S, Janda W, Schreckenberger P, Winn W. . Colour Atlas and textbook of Diagnostic Microbology. 2006. [Google Scholar]
- . . Clinical Laboratory Standards Institute. Performance standards for antimicrobial disk susceptibility testing. ;2020. [Google Scholar]
- Uneke C, Ijeoma P. The potential for nosocomial infection transmission by white coats used by physicians in Nigeria: implications for improved patient-safety initiatives. World Health Popul. 2010;11(3):44-54. [Google Scholar]
- Chacko L, Jose S, Isac A, Bhat K. Survival of nosocomial bacteria on hospital fabrics. Indian J Med Microbiol. 2003;21(4). [Google Scholar]
- Treakle A, Thom K, Furuno J, Strauss S, Harris A, Perencevich E. Bacterial contamination of health care workers' white coats. Am J Infect Control. 2008;37(2):101-5. [Google Scholar]
- Srinivasan A, Wolfenden L, Song X, Mackie K, Hartsell T, Jones H. An outbreak of Pseudomonas aeruginosa infections associated with flexible bronchoscopes. N Engl J Med. 2003;48(3):221-7. [Google Scholar]
- Qaday J, Sariko M, Mwakyoma A, Kifaro E, Mosha D, Tarimo R. Bacterial Contamination of Medical Doctors and Students White Coats at Kilimanjaro Christian Medical Centre. Int J Bacteriol. 2015. [Google Scholar] [Crossref]
- Wong D, Nye K, Hollis P. Microbial flora on doctors' white coats. BMJ. 1991;303(6817):1602-4. [Google Scholar]
- Harris A, Samore M, Nafziger R, DiRosario K, Roghmann M, Carmeli Y. A survey on handwashing practices and opinions of healthcare workers. J Hosp Infec. 2000;45(4):318-21. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.152-157
-
CrossMark
- Citation
- Received Date September 25, 2023
- Accepted Date April 24, 2024
- Publication Date March 12, 2025