Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Knowledge, attitude and practices for Personal Protective Equipment (PPE) in nursing staff of ICU in a tertiary care centre in South Gujarat
Abstract
Background: To prevent nosocomial infections among Healthcare workers (HCW), patients and even their family members. So, nurses and other HCW ought to have knowledge regarding correct use of Personal Protective Equipment (PPE).
Aims and Objective: To assess their knowledge towards use of PPE. 2) To understand their attitude about prevention of nosocomial infections. 3) To determine their application of practices and behavior towards use of PPE.
Materials and Methods: The study was a cross sectional study carried out in a tertiary care centre in south Gujarat. Nurses were asked to fill out a questionnaire based on abovementioned topics after explaining them the purpose of the study, assuring them about privacy and asking for consent. The data was collected andanalyzedwiththehelpofMicrosoftofficetoolsandSPSSandresultswereobtained.
Results: The result in section of knowledge was 5.05(56.1%) which was lower than expected. Also results of attitude related questions were 4.38(62.5%) and could be improved. Inspite of this results in above categories there were excellent score i.e. 8.34(83.4%) practices among them and good response to improving compliance towards the same.There was a positive correlation between knowledge and attitude and nurses with higher work experience had higher scores in this area.
Conclusion: Nursing staff of ICU in a tertiary care centre in South Gujarat are overall well prepared in terms of PPE availability and maintaining a healthy practice of PPE usage. But some gaps are found which can be filled with monthly or quarterly seminars, more meetings for the same cause and increasing teamwork to have better infection control practices.
Introduction
A breach in infection management practices facilitates transmission of infection from patients to health care personnel, other patients and attendants.[1] Nurses are repeatedly exposed to numerous infections throughout their nursing activities. [2]
In 1987, the CDC recommended that regardless of patient’s infection standing, the precautions should be systematically used. This extension of blood and bodyfluid precautions to all patients is referred as “universal blood and body fluid precautions” or simply “universal precautions.”[3]They are precautions that ought to be practiced by all clinical employees without exception, to limit the chance of potentially harmful organisms being transmitted to the patient, healthcare worker, visitor or the environment.[4] In the hospitals, prevention of various microbial infections is more important as the strains are often more aggressive and drug resistant than the community acquired strains. With COVID-19 pandemic around and no definite cure or treatment established, preventive care is the best control method against spreading of the virus.
Specialized clothing or equipment worn by workers for protection against health and safety hazards is called Personal Protective Equipment (PPE). PPE provides a physical barrier between microorganism and wearer. Common personal protective equipment used by ICU nurses is Respirators/ Face masks, Gloves, Eye protection/Face shields, Gowns etc. [5]
Proper guidelines for use of PPE must be followed therefore, we can prevent nosocomial infections among Health Care Worker’s (HCW), patients and even their family members. So, nurses and other HCW ought to have knowledge regarding correct use of PPE as it is as important as the efficacy of the PPE used. Within the ICUs nurses play a significant role for taking care of patients, as the patient is already physiologically weak and at a higher chance of getting infected. That is why it is very important to assess their knowledge and compliance towards use of PPE. [2], [6], [7], [8]
This was an institution based cross-sectional study which was conducted in a tertiary care centre in South Gujarat. Nurses with experience in ICU units and responsible for control of nosocomial infections were requested to participate in the study which was conducted with the help of a well-structured questionnaire which helped to analyze the knowledge, attitude as well as practices and behavior of nurses towards PPE.
The study gave an idea regarding knowledge of nurses like components of PPE, their donning, doffing technique, effectiveness of various components in various situations. We also got an insight on the use of PPE, whether used with proper protocol, their PPE disposal knowledge and habits; do the nurses believe in PPE to control the nosocomial infections, the behaviors of colleagues as well as their superiors towards the measure. It also provided an idea of hand hygiene habits among the nurses. The reason behind bad attitude or noncompliance were also obtained like unavailability, misbelieves, etc. It also provided knowledge about reuse of PPE among different patients.
Materials and Methods
This was an institution based cross-sectional study which was conducted in a tertiary care centre in South Gujarat to analyze knowledge, attitude and practices for Personal Protective Equipment (PPE) in nursing staff of ICU. Total 102 nurses having experience in the ICU’s of surgery, Medicine, Pediatrics, neonates and obstetrics department were enclosed in the study. Data was collected with the assistance of a well-structured questionnaire. The questionnaire is prepared with the help of WHO guidelines and alternative references.[9] Questions include details of their personal and professional information as well as their knowledge, attitude and practice pertaining to their compliance with usage of PPE.
Sampling method
Eligible participants were selected by random sampling. The study took place in microbiology lecture hall in 3 different batches on 3 different days of March 2021. The nurses were allowed to choose their batch as per their schedule. Information about the study was provided and explained to the nurses in their own language as well as they were assured about the confidentiality and protection of their identity by assigning a participant ID. The consent form was explained and given to them to sign voluntarily. The questionnaire was provided to them and was explained to them, when needed. The nurses absent during the study and incompletely or inappropriately filled form entries were excluded. Also, the nurses with experience of less than 6 months were excluded from the study.
Data analysis
All the data obtained was entered into excel sheets and they were scored 0 or 1 for wrong and correct answer respectively for knowledge and practice related questions. Likert grading system was used for the attitude and some behavior questions. The descriptive statistics was done with the help of Package on Social Services (SPSS). Result was assessed according to scores of individuals. The score of <50%- poor, 50-70%-good and>70% -excellent.
Results
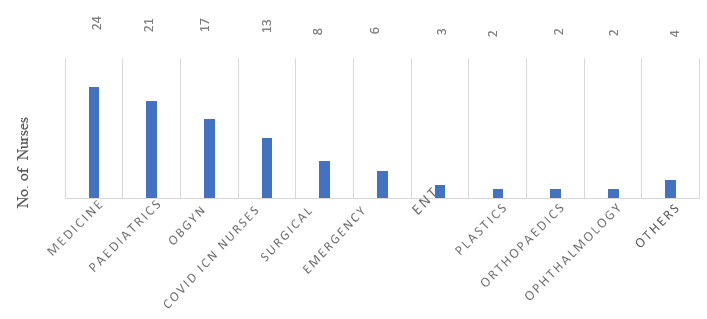
The study population of 102 nurse were working in different departments as follows: Medicine 24(23.5%), Pediatrics 21(20.6%), Obsgyn 17(16.7%), Covid ICN 13(12.7%), Surgical 8(7.8%), Emergency 6(5.9%), Plastics 2(2%), Orthopedics 2(2%), Ophthalmology 2 (2%), Others 4 (3.9%).[[Table 1]]
All of them had attended the Hospital training programme regarding PPE protocols and usage. Proportion of the participants had gained knowledge from extra sources: Medical journals 23(22.5%), Internet 32(31.4%), Friends and colleagues 19(18.6%).
|
N=102 |
|
|
Mean |
8.569 |
|
Std. Error of Mean |
0.8364 |
|
Median |
4.250 |
|
Mode |
2.0 |
|
Std. Deviation |
8.4476 |
|
Range |
26.5 |
|
Minimum |
0.5 |
|
Maximum |
27.0 |
|
Percentiles: 25th |
2.375 |
|
50th |
4.250 |
|
75th |
14.250 |
They had an average work experience ranging from minimum of 6 months to maximum of 27 years with mean of 8.5 years, median of 4.25 years and a mode of 2 years with 7-8 hours of work per day.
|
N=102 |
Knowledge Score |
Attitude Score |
Behavior Score |
|
Mean |
5.05 |
4.38 |
8.34 |
|
Std. Error of Mean |
0.138 |
0.116 |
0.137 |
|
Median |
5.00 |
4.00 |
9.00 |
|
Std. Deviation |
1.396 |
1.169 |
1.382 |
|
Skewness |
-0.156 |
0.195 |
-0.986 |
|
Std error of skewness |
0.239 |
0.239 |
0.239 |
|
Range |
7 |
6 |
7 |
|
Minimum |
1 |
1 |
3 |
|
Maximum |
8 |
7 |
10 |
|
Percentiles |
|||
|
25th |
4.00 |
4.00 |
8.00 |
|
50th |
5.00 |
4.00 |
9.00 |
|
75th |
6.00 |
5.00 |
9.00 |
Overall statistics is show above [[Table 2]] with good (50-70%) result in knowledge and attitude section while excellent (>70%) result in behavior and practices section. Results of individual sections are as follows:-
Knowledge related questions
The scores among individual questions were distributed as shown in [Figure 2].
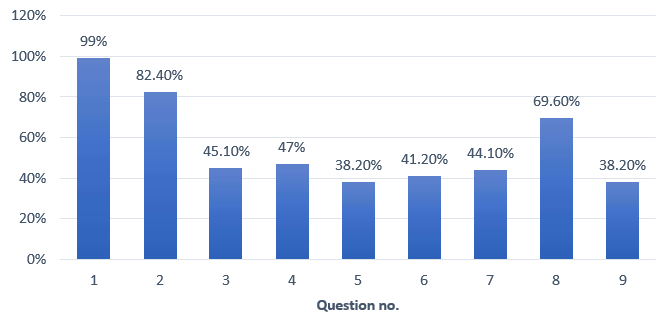
Q1 i.e. full form of PPE was chose correctly by 99% (101) nurses. Q2 asked about parts of PPE which included gloves, gown, hairnet, mask and respirators, goggles, shoe cover, face shield was answered correctly by 82.4%(84). Q3 and Q6 asked about donning and doffing sequence of PPE which was correctly answered by 45.1%(46) and 41.2%(42) nurses respectively. Q4 asked whether one should use alcohol based hand rub when they are visibly soiled. The answer was false, as they should be washed by soap and water with correct method. 47%(48) nurses correctly chose false. Q5 asked whether correct use of PPE eliminates need of hand hygiene which was correctly answered no by 38.2%(39) nurses as hand hygiene is an integral part of infection control practices which has to be used along with proper PPE to maximize the control of infection. Q7 asked about most effective method of protection from infected body fluids and was answered correctly by 44.1%(45) nurses. Q8 asked most cost effective method to prevent hospital acquired infection which was answered correctly by 69.6% (71) nurses. Q9 asked about size of particles filtered by N95masks which was correctly by 38.2%(39) nurses.
The number of people with excellent score i.e. more than 7(>70%) were 2(2%), good i.e.5-7(50-70%) were 63(61.8%) and poor score i.e. less than 5 (<50%) were 37 (36.3%). Mean score of the participants were 5.05 indicating overall result in this section was good.
Attitude related questions
Analysis of attitude related questions are shown in [Figure 4].
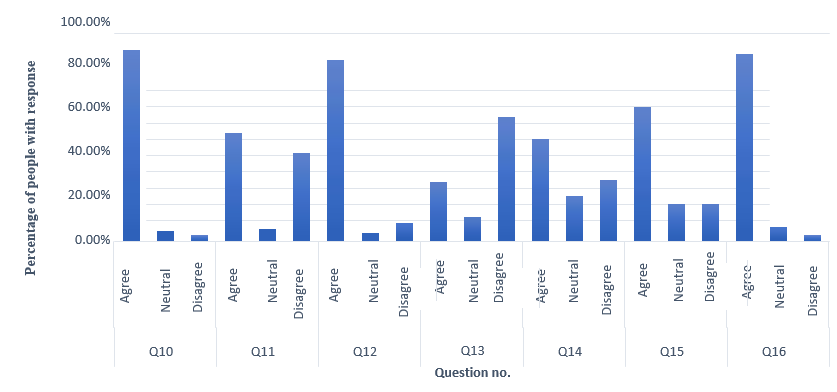
Q10 analysis found that 92.1% (94) nurses agree that they know correct use of PPE. According to responses on Q11, 51.9% (53) nurses believe they should on PPE inside the patient’s room and 42.2% (43) nurses disagree while5.9%(6) are neutral regarding the topic. Q12 responses suggest 87.3% (89) nurses agree to proper technique of gown removal i.e. turning the gown inside out, in a peeling motion and holding away from body. By analyzing Q13 answers we found 28.4% (29) nurses agree while 59.8%(61) disagree on using same gloves on all patients in same room as long as they are not visibly soiled.49%(50) nurses agree that PPE will keep patients and health care workers.
From getting infected while 21.6% (22) are neutral and 29.4% (30) disagree on the matter as suggested by Q14. As per Q15 responses; 17.6%(18) nurses disagree and same number of nurses are neutral to the question that PPE interfere with patient care and while 64.7% (66) nurses agree to the matter.Q16 asks whether wearing face mask and goggles during procedures with aerosol production is mandatory; to which 90.2%(92) nurses agree while 6.9% (7) are neutral and 2.9%(3) disagree to it.
17(16.7%) participants were found to have excellent attitude by scoring more than 5 (>70%) in this section. 64 (62.7%) participants had good attitude by scoring 3-5 (50-70%) in this section and 21(20.6%) participants had a poor attitude by scoring less than 3 (<50%) Average attitude levels were 4.38 indicating good attitude.
Behavior and Practices related question
Analysis of behavior and practices related questions is shownin [Figure 4].
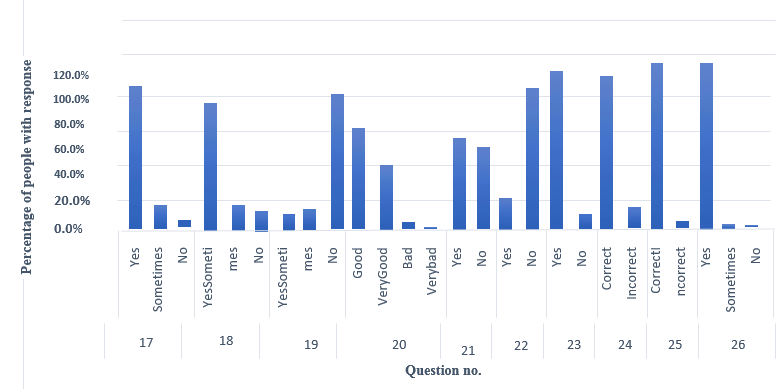
According to Q17, 82.4% (84) nurses say yes, 13.7% (14) say sometimes and 3.9%(4) nurses say no to availability of recommended PPE at all times in the ICU. 73.5%(75) nurses think that the head nurse or attending physician would always reprim and someone for not using PPE, while 14.7% (15) nurses think sometimes and 11.8% (12) think they wouldn’t get punished as per responses to Q18.77.5% (79) nurses deny to Q19 that their colleagues often forget to use recommended PPE; 12.7% (13) say sometimes and 9.8% (10) agree to the question.Q20 asks nurse’s views regarding compliance to PPE where,37.3% (38) chose “very good”, 57.8% (59) chose “good”, 3.9%(4) chose “bad” and 1% (1) chose “verybad”. According to Q21, 52.9% (54) nurses remove PPE immediately after leaving the patient’s room and 47.1% (48) did not. Q22 suggests 81.4% (83) nurses don’t forget to change PPE between patients, while 18.6%(19) often forget. 91.2% (93) nurses say yes to Q23 that they believe compliance can be improved towards PPE. Q24 asks nurses what PPE components they may use in taking care of a patient with Mycoplasma pneumonia infection and 88.2% (90) answer correctly. 96.1% (98) nurses know that red bag must be used to discard goggles and gloves as per responses to Q25. 96.1% (98) say yes to following hand hygiene before PPE donning, 2.9% (3) says sometimes.
78(76.5%) nurses had an excellent score i.e. more than 7 (>70%) in this section while 23(22.5%) nurses had average i.e.5-7 (50-70%) and 1(1%) had poor result i.e. <5(<50%). Average score in this section was 8.34 indicating excellent behavior and practices.
Correlations
We found a positive correlation between knowledge and attitude with 2-tailed sig levels of 0.027 [[Table 3]].
|
N=102 |
Knowledge Score |
Attitude Score |
|
|
Knowledge Score |
Pearson Correlation |
1 |
0.219* |
|
|
Sig.(2-tailed) |
|
0.027 |
|
Attitude Score |
Pearson Correlation |
0.219* |
1 |
|
|
Sig.(2-tailed) |
0.027 |
|
We also found a positive correlation between working experience and knowledge [Sig (2-tailed) =0.018] and attitude scores [Sig (2-tailed)=0.020] by spearman’s rho test indicating higher the work experience, higher the knowledge and better attitudes overall. [[Table 4]]
|
N=102 Spearman’s rho Test |
|
Working experience (in years) |
Knowledge Score |
Attitude Score |
|
Working experience (in years) |
Correlation Coefficient |
1.000 |
.235* |
0.231* |
|
Sig.(2-tailed) |
|
0.018 |
0.020 |
|
|
Knowledge Score |
Correlation Coefficient |
0.235* |
1.000 |
0.171 |
|
Sig.(2-tailed) |
.018 |
|
0.086 |
|
|
Attitude Score |
Correlation Coefficient |
.231* |
0.171 |
1.000 |
|
Sig.(2-tailed) |
0.020 |
0.086 |
|
Discussion
Hospital acquired infection have been recognized as a serious problem affecting the quality of health care.[10] Its control relies mainly on operational effectiveness of health care workers which we have tried to indirectly analyze by this study of Knowledge, Attitude and Practices regarding PPE.
The result of the whole section was 5.05(56.1%) which was lower in comparison with Ginny Kaushal et al.[11] which had 78.69%, Hossain et al.[12] which had >99% and Garg Kamakshi et al.[13] which had 78.17%. The above scores were not expected due to regular training programs held in the hospital. Considering that a high number of nurses deny unavailability of PPE, leniency of their seniors regarding inappropriate use of PPE there must be other reason for this result like high patient load, lack of appreciation towards importance of using the recommended sequence, laziness, etc. [14]
Attitude levels were also good i.e. 4.38(62.5%) but were lower compared to Ginny Kaushal et al.[11] which had 88.89%,Hossainetal.[12] which had 88% but higher than Garg Kamakshi et al.[13] which had 58.95%. It was a shocking finding that only about half of the nurses believe that PPE will protect patients from infections. This attitude may be due to personal experience of ineffectiveness, improper use, etc. Also a high number of nurses think PPE interferes with patient treatment which might be due to time consumed for donning and doffing and can result in decreased compliance and wrong belief that PPE won’t protect against infections.
Despite of average levels of knowledge and attitudes there is excellent behaviour and practice among the nurses i.e. 8.34 (83.4%). This was lower than Ginny Kaushal et al.[11] which had 90.78% but higher than Hossain et al.[12] which had 51.7% and Garg Kamakshi et al.[13] which had 74.3%. Majority of nurses follow hand hygiene before PPE donning which is a good sign. A large percentage of nurses also use appropriate PPE in given situations and use correct method and of bags disposal accordingly. More than 90% of nurses believe that compliance towards PPE can be improved and thus they can be helped by various methods like timely lectures, improving understanding, guidance of seniors to their peers, scheduled training etc.
We found a positive correlation between knowledge and attitude which was seconded by Ginny Kaushal et al.[11] and Hossain et al.[12] and we also found a positive correlation between working experience and scores of knowledge and attitude which was a new finding not noted previously.[15]
Conclusions
Nursing staff of ICU in a tertiary care centre in South Gujarat are overall well prepared in terms of PPE availability and maintaining a healthy practice of PPE usage. But there are gaps found in knowledge regarding protocols, procedures, and attitude. Also the majority nurses agree on the notion of increasing the compliance towards PPE which is a very positive finding. Observational studies must be done to confirm the findings above and find reason behind the observed results. They can be asked about their views and suggestions which can lead to more compliant population. Knowledge gaps can be filled with monthly or quarterly seminars, more meetings for the same cause, encouraging reading and subscription to medical journals and increasing teamwork to have better infection control practices.
Ethical Approval
The study was conducted after getting approval from Human Research Ethics Committee (No. GMCS/STU/ETHICS/Approval/13204/2020).
Source of Funding
None.
Conflict of Interest
None.
Acknowledgement
The present study is selected and approved by ICMR-Short Term Studentship (STS) 2020 having a reference ID: 2020-05195.
References
- Lakshmi PA, Jennifer H, Stanly A, Paul C. A study on personal protective equipment use among health care providers, Tamil Nadu. Int J Community Med Public Health. 201824;5(5):1771-4. [Google Scholar]
- Abukhelaif A. Personal Protective Equipment Knowledge and Practices among Nurses Working at Al-Baha King Fahad Hospital, Saudi Arabia. J Healthc Commun. 2019;4(1). [Google Scholar] [Crossref]
- Notes E, Update R. Epidemiologic Notes and Reports Update: Human Immunodeficiency Virus Infections in Health-Care Workers Exposed to Blood of Infected Patients. MMWR Weekly. 1987;36(19):285-9. [Google Scholar]
- Mudedla S, Tej W, Reddy K, Sowribala M. A study on knowledge and awareness of standard precautions among health care workers at Nizam's institute of medical sciences Hyderabad. J Natl Accreditation Board Hosp Amp Healthc Provid. 2014;1(2). [Google Scholar]
- . National Personal Protective Technology Laboratory | NPPTL | NIOSH |CDC [Internet]. . 2021. [Google Scholar]
- Hinkin J, Gammon J, Cutter J. Review of personal protection equipment used in practice. Br J Community Nurs. 2008;13(1):14-9. [Google Scholar]
- . Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. . 2021. [Google Scholar]
- Suzuki T, Hayakawa K, Ainai A, Iwata-Yoshikawa N, Sano K, Nagata N. Effectiveness of personal protective equipment in preventing severe acute respiratory syndrome coronavirus 2 infection among healthcare workers. J Infect Chemother. 20211;27(1):120-2. [Google Scholar]
- . Personal Protective Equipment [Internet]. . 2021. [Google Scholar]
- Sodhi K, Arya M, Chanchalani G, Sinha V, Savio R, AAK. Comparison of knowledge and awareness of infection control practices among nurses in India: A cross-sectional survey. Am J Infect Control. 2022;50(12):1368-73. [Google Scholar]
- Kaushal G, Doke P, Shah A, Verma V. An Analysis of Knowledge, Attitude and Practices regarding Standard Precautions of Infection Control and Impact of Knowledge and Attitude of ICU Nurses on Self-reported Practices of Infection Control. Int J Res Found Hosp Healthc Adm. 2015;3(2):79-85. [Google Scholar]
- Hossain M, Rashid M, Khan M, Sayeed S, Kader M, Hawlader M. Healthcare Workers' Knowledge, Attitude, and Practice Regarding Personal Protective Equipment for the Prevention of COVID-19. J Multi discip Healthc. 2021;14:229-38. [Google Scholar] [Crossref]
- Garg K, Grewal A, Mahajan R, Kumari S, Mahajan A. A Cross-Sectional Study on Knowledge, Attitude, and Practices of Donning and Doffing of Personal Protective Equipment: An Institutional Survey of Health-Care Staff during the COVID-19 Pandemic. Anesth Essays Res. 2020;14(3):370-5. [Google Scholar]
- Sobeh D, SM, Abdelkader H. Nurses Knowledge and Practice Regarding Infection Control Measures in Intensive Care Units. Port Said Sci J Nurs. 2023;10(3):91-108. [Google Scholar]
- Sahiledengle B, Gebresilassie A, Hiko D, Getahun T. Infection Prevention Practices and Associated Factors among Healthcare Workers in Governmental Healthcare Facilities in Addis Ababa. Ethiopia. Ethiop J Sci. 2018;28(2):177-86. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 5 Views
- DOI 10.18231/pjms.v.15.i.1.168-173
-
CrossMark
- Citation
- Received Date February 28, 2024
- Accepted Date June 25, 2024
- Publication Date March 12, 2025