Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Utilities of tripsin and trypan blue for diagnosis of dermatophytes
Abstract
Introduction: Dermatophytes are group of keratinophilic fungi invading keratinized tissues of skin and its appendages. Althugh it is not a life threatening condition, the lesions may spread in size and are associated with significant negative cosmetic, social, psychological impact leading to adverse effects on the way of life. Although diagnosis of dermatophytosis is essentially clinical, laboratory methods will help to confirm the diagnosis and appropriate treatment of the disease. Early diagnosis and treatment of index case within family and/or community will reduce spread of dermatophytic infections.
Aim and Objectives: Detect dermatophytes infection by microscopic examination using 10% KOH (Potassium Hydroxide) as well as Neutral Red, to isolate dermatophyte on Sabourard's Dextrose agar with or without treatment with trypsin and to compare the effect of trypsin on isolation of dermatophytes.
Materials and Methods: Prospective cross sectional, laboratory-based study conducted at a tertiary care centre. A total of 60 samples were included in the study. Microscopical examination followed by culture was done for all the samples. The sample was divided into two parts out of which one was treated with trypsin and other without trypsin. Both parts were further processed by the standard mycological protocol. We also used neutral red to assess the viability of fungal pathogen.
Results: The study consisted of 40 (66.66 %) male patients and 20 (33.33 %) female patients.The mean age of the study population was 34.97 + 19.03 yrs.Majority of samples were for nail diseases, 83.33% Dermatophytes were visualized by direct microscopy with KOH mount in 12 (20%) cases. The neutral red staining after trypsonization yields positive result in 26 (43.33%) cases. The dermatophytes were cultured on SDA with and without trypsin treatment of the specimens. The growth was observed in 26 (43.33%) cases and 24 (40%) cases respectively. Culture positive growth (40 %) cases while KOH positivity was observed in 20% samples.
Conclusion: Trypsinization improves fungus culture. However use of Neutral red and Trypsinization helped in achieving better results as compared to conventional methods.
Introduction
Dermatophyte infection is a global concern that accounts for majority of superficial fungal infections. The prevalence of superficial fungal infection ranges 20-25% worldwide.[1] The infection caused by dermatophytes is also called as “tineas” and are named according to the affected body site. [2]
Dermatophyte infections are contagious. These are transmissible from human to human and/or animals to humans. After contact with infected person, hyphal fragments or arthroconidia are deposited on the superficial skin layers. Other factors like airborne spread fomites or even contact with infected animal may lead to deposition of arthroconidia on skin. Germination of the adhered spores takes utmost 4-6 hr. The dermatophytes invade the keratinized tissues of a healthy human host. The fungi then penetrate the surface barriers, causes lysis and absorption of tissue, and develop resistance to immune defences. [3]
The lesions may spread in size and are associated with adverse effects. It poses cosmetic, psychological and social adverse effects in many patients. [4] Although dermatophytosis is not a life threatening disease it is many times difficult to differentiate from other skin disorders.
Hence laboratory investigations is of significant importance for correct diagnosis and management.[5] Early diagnosis and treatment of index case within family and/or community will reduce spread of dermatophytic infections.
Simple method of diagnosis includes direct microscopic examination of skin, hair and nail samples. It is simple, rapid, inexpensive and efficient technique that can be done on an outpatient basis and the results will be available within 1-2 h. [6] However, direct microscopy has its limitation as it only detects the presence or absence of fungal elements but cannot differentiate among species. Also, it requires experience to interpret the smears otherwise inexperienced observer may misdiagnose certain artefacts.
Also, culture is essential after microscopy for definitive identification of the etiological species. The choice of therapy may depend upon the species causing infection. It has been observed that direct microscopic findings show fungal infection, but fungi do not grow on culture. [7] This may be seen due to presence of nonviable fungi in the specimen that yields negative growth on culture. Thus difficulties in diagnosis are double fold. [4]
The Fungi can be visualized by using potassium hydroxide mount, NAOH (sodium hydroxide), or Di-Methyl Sulphaoxide (DMSO). Treatment with trypsin helps in better digestion of tissue as compared to potassium hydroxide which gives good results of wet mount of fungal element. Neutral red gives better visualization of fungal element as it stains only viable cell which was confirmed by auto radiographic study using 3H-thymidine. Hence increased sensitivity of culture is obtained by doing trypsinization along with neutral red. Since conventional methods are not yielding sufficient evidence for the initiation of therapy, the quest for newer method is never ending process.
Here, we have compared the use of trypsinisation technique along with neutral red staining with conventional technique for recovery of dermatophytes.
We aimed to detect dermatophytes infection by microscopic examination using 10% KOH (Potassium Hydroxide) as well as Neutral Red, to isolate dermatophyte on Sabourard's Dextrose agar with or without treatment with trypsin and to compare the effect of trypsin on isolation of dermatophytes.
Very few studies are available on this topic. Furthermore the study may help in finding locally prevalent dermatophyte species which varies according to the geographical locations.
Materials and Methods
This was a Prospective cross sectional, laboratory-based study conducted at tertiary care centre after approval from the ECARP PG academic committee. The waiver of informed consent was taken since department receives specimens from suspected cases of dermatophyte infections, the present study was conducted on leftover samples received for routine mycological diagnosis. The study was conducted for a period of 18 months, from June 2019 till December 2020.
Patients of all ages and both sexes with clinically suspected dermatophytic infections were included in the study. Patients taking antifungal treatment before collection of samples and who had received topical/systemic antifungal treatment anytime during last 2 months were excluded from the study. A total of 60 samples were included in the study.
Sample collection
Skin scrapings were collected from the active edges of suspected lesions using sterile scalpel blade. The scrapings were collected in a sterile petri dish. Infected hairs were taken by plucking with forceps. If nails were involved, nail clipping were collected. A detailed treatment history of patient was also noted.
Samples were divided into 2 parts and processed as described below.
Sample processing
The sample processing was divided in two parts. First part was processed as per the regular protocol. In First part, the portion of sample was mixed with 10% potassium hydroxide for 30 minutes and then looked under microscope (40X) for fungal elements (direct microscopy) and remaining part was cultured on Sabouraud’s dextrose agar with and without chloramphenicol and tubes were incubated at 25 degree and 37 degree for 24 hours respectively.
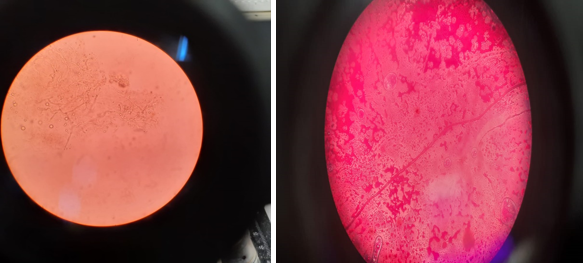
In second part, portion of the sample was treated with 2% trypsin and then looked for fungal elements under microscope using 1% Neutral red and 10% potassium hydroxide while the remaining portion was cultured on Sabouraud’s dextrose agar with and without chloramphenicol.
Two (2%) trypsin & 0.5% Neutral red was made in phosphate buffer saline; both solutions were sterilized by passage through 0.22 micro meter GS membrane filter. One part of scrapping was put in 1 ml of 2% trypsin solution and kept at 370 C for 2 hours. The scales were then washed with phosphate buffered saline (PBS) by centrifuging 3 times (1500 g for 10 min). The deposits were suspended in 300 microliter phosphate buffered saline (PBS). 200 microliters of this PBS treated sample was cultured on Sabouraud’s dextrose agar supplemented with cycloheximide alone and Sabouraud’s dextrose agar with gentamycin (0.026mg/dl) & cycloheximide (0.05mg/ml). 100 microliters of remaining part of suspended deposit was mixed with an equal amount of 1% neutral red and was kept at room temp for 1 hour.
This was then microscopically examined as wet mount under dry 40 X objective. The part of the sample, not treated with trypsin was processed by standard mycological techniques. All the culture tubes were incubated at 250C and 370C for 1 month before declaring negative result. The growth obtained was identified by gross appearance and then microscopically. All the yeasts were identified by germ tube test, sporulation on corn meal agar and Hichrome candida agar.
For primary isolation of fungi, Sabouraud's dextrose agar was used. Macroscopic and microscopic characteristics of the culture was then used for identification. Texture, rate of growth, pigmentation on obverse and reverse side of the cultures were employed to characterize the fungi. Lactophenol cotton blue mount was used to for microscopical examination. Slide culture was done to study microconidia, macroconidia and special structures such as spirals, pectinate, racquet hyphae, and chlamydospores.
Findings were tabulated, compared and results were interpreted.
Results
The present study consisted of 60 patients. It included 40 (66.66 %) male patients and 20 (33.33%) female patients. The male to female ratio was 2:1. The mean age of male patients was 36.92 ± 20.60 and of female patients was 31.07 ± 14.64.
The study participants were equally distributed in different age groups as shown in [Table 1]. Although the study had only 4 (6.67%) patients from above 61 age group. The mean age of the study population was 34.97 ± 19.03 with the range from 6 month to 88 years.
|
Age groups |
Male (A) |
Female (B) |
Total (A+B) |
|
0-20 |
11 |
5 |
16 |
|
21-40 |
12 |
8 |
20 |
|
41-60 |
13 |
7 |
20 |
|
>61 |
4 |
0 |
4 |
|
Total |
40 |
20 |
60 |
|
|
Mean- 36.92yr |
mean - 31.07yr |
Mean - 34.97yr |
|
|
SD- 20.60 |
SD- 14.64 |
SD- 19.03 |
|
Max – 88yr |
Max- 50yr |
Max- 88yr |
|
|
Min – 8yr |
Min - 6 month |
Min – 6 month |
Majority of the samples collected were for nail diseases. In our study, 50 (83.33%) samples were nails and 9 (15%) samples were of skin scrapings. Hair samples were the least 1 (1.67%) among the totalt samples collected.
Most of the patients enrolled in our study had nail disorders. The nail disorders included in the study were nail dystrophy 8 (13.33 %), Onychomycosis 18 (30 %) and T. unguium 24 (40 %). The clinical diagnoses of skin infections were Tinea Facei 2 (3.33 %), Tinea corporis 4 (6. 67%), Tinea cruris 3 (5 %) and least was Tinea capitis 1 (1.67%).
All the samples were mounted for direct examination under microscope using KOH. The KOH mount has helped to identify the fungal pathogen in 12 (20 %) of cases and was negative in 48 (80%).
All the samples were cultured and following species of fungi were identified- Candida albicans (11.67%), Candida glabarta (8.33%), Candida tropicalis (5%), Microsporon gypsum (1.67%), Syncephalostrum racemosum (1.67%), Trichophyton mentagrophyte (6.67%), Trichophyton rubrum (6.67%) and Trichophyton voilaceum (1.67%). In 56.67% samples, species could not be identified as growth was not observed in culture media.
After trypsinization, dermatophytes were visualized in 26 (43.33%) samples whereas Dermatophytes were visualized by direct microscopy with KOH mount in 12 (20%) cases. The neutral red staining after trypsinization gave positive result in 26 (43.33%) cases.
The dermatophytes were cultured on SDA without trypsin treatment of the specimens and growth was observed in 24 (40%) cases whereas when cultured on SDA after trypsin treatment of the specimens growth was observed in 26 (43.33%) cases.
The comparison of KOH and Culture positive dermatophyte isolates is shown in the following [Table 2].
|
KOH/Culture |
Culture positive |
Culture Negative |
Total |
|
KOH Positive |
12 (20%) |
0 |
12 (20%) |
|
KOH negative |
12 (20%) |
36 (60%) |
48 (80%) |
|
Total |
24 (40%) |
36 (60%) |
60 (100%) |
Discussion
Superficial cutaneous fungal infections are very common and affect 20% to 25% of the world's population.[8] The current study attempts to find the difference between conventional methods and after trypsinization of the sample.
KOH examination is the point of care of microscopic diagnosis of the dermatophytosis. Dimethyl Sulfoxide (DMSO), neutral red and Periodic Acid Schiff stain are some of the reagents used for visualization of the fungus in skin scrapings on direct microscopy.
Different concentrations of KOH, NaOH, dimethyl sulfoxide can be employed to clear the specimen. The specimen can be mounted in any of these solutions and heated to emulsify lipids before examination. However, confirmed diagnosis can be made on culture. Inability to visualize the fungus on direct microscopy or growing it in culture by standard method poses difficulties to report the results to the clinicians. Further long duration of treatment and emergence of resistance in fungal pathogen have warranted newer methods that gives results with accuracy and high sensitivity. [9]
In our study, microscopical examination and culture was done on all samples. One part of the sample was treated with trypsin and other part was processed without trypsin. Both parts were further processed by the standard mycological protocol. We also used neutral red to assess the viability of fungal pathogen.
Colony and microscopic appearance of fungi was examined as mentioned in the study by Pravesh Yadav et al. [10] The remaining part of the specimen was divided and inoculated into specific agar surfaces. Culture media employed for the growth was Sabouraud's dextrose agar with chloramphenicol (0.05 g/l), gentamicin (20 mg/l) and cycloheximide (0.5 g/l) and Dermatophyte Identification Media (DIM). The inoculated tubes were incubated at 25°C for optimal growth. Growth was confirmed by morphology of the colony and microscopic appearance on Lacto Phenol Cotton Blue (LPCB) mount. [10]
The trypsin treatment method for culture-based diagnosis of dermatophyte is easy to perform and less expensive. Xess et al have observed that treatment of specimens with trypsin prior to culture increases the sensitivity of the culture technique. [9]
The present study was performed on 60 patients who were clinically diagnosed with dermatophytic infections and their samples were obtained in the laboratory for confirmation of the clinical diagnosis.
Our study consists of 40 (66.66 %) male patients and 20 (33.33 %) female patients. The male to female ratio was 2:1. The study participants were equally distributed in different age groups. Although the study had only 4 (6.67%) patients from above 61 age group. The mean age of the study population was 34.97 ± 19.03 with the range from 6 month to 88 years. Dermatophytosis is found to be common in young adults although it has been observed that tinea capitis is more common in paediatric age group. [11] Dermatophytic infections are more common among males than females. The reason may be greater physical activity and increased exposure to sun and resultant increased sweating in males.
Raghvendra Pratap Singh et al. [12] observed that the mean age was 35.93 years with range between 14 to 72 years that included 64(62%) males and 40(38%) females. Jain et al.[13] found male: female ratio of 1.3:1.
Kaur et al.[14] observed the dermatophytosis infection common (20.4%) among age group of 21-30 years. Kaur et al.[14] observed male to female ratio of 1.6:1. Doddamani et al.[15] reported males (73%) were more frequently affected than females (27%) and Male to female ratio was 2.7:1. Smita kulkarni et al.[16] reported the male to female ratio was 2.04:1 and the predominant age group in males and females was 31 to 40 years. [16] Swati Jain et al.[13] found that dermatophytic infections were common in the adult age group (21–40 years) which is well correlated with the other studies. Thus Most of the studies showed findings similar to our study with the commonest age group involved being in the range of 20-40 years and male preponderance. The mean age of 34.97 of our study also matches the other studies. The other possible reasons might be due to the working culture which predisposes middle aged persons to climatic conditions and also causes occupational exposure. Also, increased socialization in this age group might further lead to infection spread.[13] The higher prevalence in the middle age group is possibly accorded to occupation-related trauma. The higher incidence of nail disorders in males may be related to more exposure to outdoor physical activity which makes the nail prone to trauma. Perea et al. [17] also reported a higher incidence in males as compared to females. Pravesh Yadav et al.[18] reported the mean age of the study population as 42.4 years in and 40% of the patients belonged to the age group of 31-45 years. Adhikari et al. have reported high prevalence (58.8%) of onychomycosis during the third decade [19] The majority of our patients were having nail disorders. The age group of presentation in our study matches the other studies done on onychomycosis.
The majority of the samples collected in our study were for nail diseases. 83.33% samples were nails. 15 % samples were of skin scrapings. The hair samples were the least among the different samples in our study. The nail disorders included in our study were Nail dystrophy (13.33 %), Onychomycosis (30 %) and T. unguium (40 %). The clinical diagnoses of skin infections in our study were Tinea Facei (3.33 %), Tinea corporis (6. 67%). and Tinea cruris (5 %).
All the samples were cultured and following species of fungi were identified- Candida albicans, Candida glabarta, Candida tropicalis, Microsporon gypsum, Syncephalostrum racemosum, Trichophyton mentagrophyte, Trichophyton rubrum and Trichophyton voilaceum. In 56.67 % samples, species cannot be identified as growth was not observed in culture media. The most common species identified were Candida albicans (11.67 %) followed by Candida glabarta (8.33 %) and then by Trichophyton mentagrophyte, (6.67%) and Trichophyton rubrum (6.67%). Pravesh Yadav et al. [18] have observed that the most common isolated fungus was T. interdigitale (61%), followed by T. rubrum (34%) and T.verrucosum (5%). However, studies from Delhi have reported T. rubrum as the commonest etiological fungus for onychomycosis. [20], [21] Swati Jain et al. [13] have observed that T. mentagrophyte (77.5%) was the most common dermatophyte isolated in their study followed by T. rubrum (13.3%). Smita kulkarni et al. [16] have found that most common pathogenic fungus in their study was T. rubrum. The other dermatophytes observe in their study were T. mentagrophytes, T. verrucosum, T. schoenlenii and T. tonsurans. However, the commonest isolated species in our study was Candida albicans (11.67 %) followed by Candida glabarta (8.33 %) and then by Trichophyton mentagrophyte, (6.67%) and Trichophyton rubrum (6.67%).
Trichophyton rubrum was the predominant fungus in studies from different parts of India, (Doddamani et al., 2013, [15] Lakshmi et al., 2015 [22] Kennedy kumar et al., 2007, [23] Madhavi et al., 2011 [24] Suman singh et al., 2003 [25] Smita Sharma et al., 2007 [20] Kannan et al., 2006. [26] While Microsporum canis is reported as prominent pathogenic fungus in middle east countries like Saudi Arabia, Kuwait (Abanmi et al., [27] Razzaq Adel et al., 2007). [28] Trichophyton spp follow Microsporum species in these countries also. In African countries like Nigeria (Kennedy et al., 2015), Egypt (Abdelkarim, et al., 2013) the infecting agents are similar to that of Indian subcontinent. [29], [30], [31] ([Table 3])
|
Author (sample size) |
KOH positive |
Culture positive |
KOH negative Culture positive |
KOH postive Culture negative |
KOH and Culture positive |
KOH and Culture negative |
|
Present study (n=60) |
12(20%) |
24 (40%) |
12(20%) |
0 |
12(20%) |
36(60%) |
|
Tanu arora et al [4] (n=657) |
189 (28.76%) |
91(13.85%) |
29(4.41%) |
127(19.33%) |
62 (9.43%) |
377(57.38) |
|
Manjunath M et al [5] (n=130) |
98(75.38%) |
04 (03.07%) |
28 (21.53%) |
66 (50.76%) |
32 (24.61%) |
|
|
Swati jain et al [13] (n=1200) |
1073 |
741 |
32 |
364 |
709 |
95 |
|
Adane Bitew et al [32] (n=318) |
131(41.2%) |
154(48.4%) |
75(23.6%) |
55(17.3%) |
62 (19.5%) |
105(33.3%) |
|
R. Shakthi et al [33] (n=100) |
67(67%) |
69(69%) |
10 (10%) |
18(18%) |
49(49%) |
23(23%) |
|
Surendran KAK et al [34] (n=100) |
96(96%) |
39(39%) |
4(4%) |
NA |
35(35%) |
4(4%) |
|
Doddamani et al [15] (n= 200) |
130 |
96 |
18 |
52 |
78 |
52 |
|
Veer et al[35] (n=88) |
72(81.8%) |
43(48.8%) |
5(5.6%) |
34(38.6%) |
38(48.1%) |
11(12.5%) |
|
Smita Kulkarni et al [16] (n=100) |
61 |
54 |
8 |
15 |
46 |
31 |
|
Kaur et al [14] (n=196) |
136(69.3%) |
144(73.4%) |
22(11.2%) |
4(2%) |
109(55.6%) |
41(20.9%) |
Dermatophytes were visualized by direct microscopy with KOH mount in 12 (20%) cases. The neutral red staining after trypsonization yields positive result in 26 (43.33%) cases. The difference in visualization by two difference methods is significant.
The dermatophytes were cultured on SDA with and without trypsin treatment of the specimens. The growth was observed in 26 (43.33%) cases and 24 (40%) cases respectively.
Raghvendra singh et al. [12] have observed that out of 104 patients included in the study 55 were culture positive and 49 were culture negative. Thus culture reports were positive in 52.84% cases.
Smita Kulkarni et al. [16] have conducted a study on 100 patients and observed that the 61 samples were KOH positive, while the remaining 39 were negative. Out of 100 cases 54 cases could be diagnosed by culture that indicates KOH mount was more sensitive than culture. Smita Kulkarni et al. [16] have noted that 46 samples were positive by both KOH and culture while 31 samples were negative for both KOH and culture. 15 samples were positive by KOH alone 8 samples were positive by culture alone. [16]
Tanu arora et al. [4] observed that 189 (28.76%) samples were KOH positive on direct microscopy of KOH mount while 91 (13.85%) samples showd growth on culture. Fungi were neither detected nor showed any visible fungal growth in 377 (57.38%) clinical samples. The limitation of KOH mount is that it requires adequate quantity of sample and appropriate collecting tool and expertise. These factors determine sensitivity and specificity of KOH. It was reported that less than a third of patients with clinical diagnosis of the disease had positive cultures. The reasons of negative growth on culture may include sampling error, defective culture medium or mishandling of the culture medium. [4]
Manjunath M et al conducted a study on 130 patients and found that 98 (75.38%) cases were positive for KOH &/or culture while remaining 32 (24.61%) cases were negative for both KOH & culture. 28(21.53%) cases were positive for KOH but negative for culture whereas 04(03.07%) cases were negative for KOH but yielded the fungal growth. Remaining 66(50.76%) cases have shown the fungal filaments in KOH mount and also yielded the growth. (Manjunath M Koppad M, Dadapeer S. Clinicomycological study of Dermatomycosis in a tertiary care hospital. Indian J Microbiol Res 2016;3(2):190-193.)
Swati jain et al. [13] have found that 1,073 cases (89.4%) were positive by KOH mount, 741 cases (61.75%) were positive by culture and 709 cases (59%) were positive by both KOH and culture. Mishra et al and Jain et al. [13] have reported KOH positivity was 85 and 72% and culture positivity was 64 and 62%, respectively.
Saraswati et al. [31] observed the overall positive rate either in KOH examination or culture to be 41.6 % whereas in our study it was 40%. In our study we found that culture positive growth (40%) cases while KOH positivity was observed in 20% samples, thus typsinization improved the chances of fungus culture. However use of Neutral red and Trypsinization helped in achieving better results as compared to conventional methods. Saraswati et al. [31] concluded that technical skills and expertise of the subject were pivotal in improving the isolation and identification in addition to good specimen collection methods. Thus, the findings of different mycological studies have variation in positivity rate.
Conclusion
We conclude that trypsinization improves the chances of fungus culture. However use of Neutral red and Trypsinization helped in achieving better results as compared to conventional methods.
Conflict of Interest
None.
Source of Funding
None.
References
- Sahoo A, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016;7(2):77-86. [Google Scholar]
- Welsh O, González G, Hospenthal D, Rinaldi M. Dermatophytosis (Tinea) and Other Superficial Fungal Infections. Diagnosis and treatment of fungal infections. 2015. [Google Scholar] [Crossref]
- Gnat S, Łagowski D, Nowakiewicz A. Major challenges and perspectives in the diagnostics and treatment of dermatophyte infections. J Appl Microbiol. 2020;129(2):212-32. [Google Scholar]
- Arora T, Oberoi L, Malhotra A, Kaur R. Mycological pattern of dermatophytes and non-dermatophytes in a tertiary care hospital. Int J Health Sci Res. 2020;10(4):37-41. [Google Scholar]
- MM, Koppad M, Dadapeer, Sushma. Clinicomycological study of Dermatomycosis in a tertiary care hospital. Indian J Microbiol Res. 2016;3(2):190-3. [Google Scholar]
- Kurade S, Amladi S, Miskeen A. Skin scraping and a potassium hydroxide mount. Indian J Dermatol Venereol Leprol. 2006;72(3):238-41. [Google Scholar]
- Naka W, Hanyaku H, Tajima S, Harada T, Nishikawa T. Application of neutral red staining for evaluation of the viability of dermatophytes and Candida in human skin scales. J Med Vet Mycol. 1994;32(1):31-5. [Google Scholar]
- Suganthi M. Pathogenesis and clinical significance of dermatophytes: A comprehensive review. Innov Pharm Pharmacother. 2017;4(1):62-70. [Google Scholar]
- Xess I, Dubey D, Purva M. Diagnosis of onychomycosis by trypsin treatment method. Indian J Dermatol. 2007;52(1):61-3. [Google Scholar]
- Yadav P, Singal A, Pandhi D, Das S. Clinico-mycological study of dermatophyte toenail onychomycosis in new delhi, India. Indian J Dermatol. 2015;60(2):153-8. [Google Scholar]
- Pires C, Cruz N, Lobato A, Sousa P, Carneiro F, Mendes A. Clinical, epidemiological, and therapeutic profile of dermatophytosis. An Bras Dermatol. 2014;89(2):259-64. [Google Scholar]
- Singh R, Rathore P. Clinico-mycological study of onychomycosis and pattern of drug resistance. Int J Contemp Med Res. 2020;7(1):1-4. [Google Scholar]
- Jain S, Kabi S, Swain B. Current Trends of Dermatophytosis in Eastern Odisha. J Lab Physicians. 2020;12(1):10-4. [Google Scholar]
- Kaur I, Thakur K, Chauhan S, Jaryal S. Clinico-mycological profile of clinically diagnosed cases of dermatophytosis in North India - a prospective cross sectional study. Int J Health Sci Res. 2016;6(8):54-60. [Google Scholar]
- Doddamani P, Harshan K, Kanta R, Gangane R, Sunil K. Isolation Identification and Prevelance of Dermatophytes in Tertairy Care Hospital in Gulbarga District. People’s. J Scientific Res. 2013;3(2):10-3. [Google Scholar]
- Kulkarni S, Bhakre J, Damle A. Clinico Mycological Study of Onychomycosis in Tertiary Care Centre of Maharashtra, India . Int J Curr Microbiol App Sci. 2017;6(11):2718-25. [Google Scholar]
- Perea S, Ramos M, Garau M, Gonzalez A, Noriega A, Palacio A. Prevalence and risk factors of tinea unguium and tinea pedis in the general population in Spain. J Clin Microbiol. 2000;38(9):3226-30. [Google Scholar]
- Yadav P, Singal A, Pandhi D, Das S. Deepika Pandhi, and Shukla Das Clinico-Mycological Study of Dermatophyte Toenail Onychomycosis. Indian J Dermatol. 2015;60(2):153-8. [Google Scholar]
- Adhikari L, Gupta A, Pal R, Sing T. Clinico-etiological correlates of onychomycosis in Sikkim. Indian J Patthol Micribiol. 2009;52(2):194-7. [Google Scholar]
- Sarma S, Capoor M, Deb M, Ramesh V, Aggarwal P. Epidemiologic and clinicomycologic profile ofonychomycosis from north India. Int J Dermatol. 2008;47(6):584-7. [Google Scholar]
- Kaur R, Kashyap B, Makkar R. Evaluation of clinicomycological aspects of onychomycosis. Indian J Dermatol. 2008;53(4):174-8. [Google Scholar]
- Poluri L, Indugula J, Kondapaneni S. Clinicomycological study of dermatophytosis in south india. J Lab Physicians. 2015;7(2):84-9. [Google Scholar]
- Kumar K, Kindo A, Kalyani J, Anandan S. Clinicomycological profile of dermatophytic skin infections in a tertiary care center - a cross sectional study. Sri Ramachandra J. med. 2007;1(2):12-5. [Google Scholar]
- Madhavi S, Ramarao M, Jyothsna K. Mycological study of dermatophytosis in rural population. Ann Biol Res. 2011;2(3):88-93. [Google Scholar]
- Singh S, Beena P. Profile of dermatophyte infections in Baroda. Indian J Dermatol Venereol Leprol. 2003;69(4):281-3. [Google Scholar]
- Kannan P, Janaki C, Selvi G. Prevalence of dermatophytes and other fungal agents isolated from clinical specimens. Indian J Med Microbiol. 2006;24(3):212-5. [Google Scholar]
- Abanmi A, Bakheshwain S, Khazzi NE, Zouman A, Hantirah S, Harthi F. characteristics of superficial fungal infections in the Riyadh region of Saudi Arabia. Int J Dermatol. 2008;47(3):229-35. [Google Scholar]
- Adel AR, Sultan A, Basmiah A, Aftab A, Nabel N. Prevalence of tinea capitis in Southern Kuwait. Mycoses. 2007;50(4):317-20. [Google Scholar]
- Wariso K, Igunmaso J, Oboro I. Pattern of Dermatophytes Isolated in the Medical Microbiology Laboratory of the University of Port Harcourt Teaching Hospital, Rivers State, Nigeria. Adv Microbiol. 2015;5(5):346-50. [Google Scholar]
- Aboueisha A, El-Mahallawy H. Public health significance of dermatophytes in Ismailia and Port Said Provinces, Egypt. Med Mycol J. 2013;54(2):123-9. [Google Scholar]
- Jayanthi R, Nagamani R, ML, Rao R. Incidence and Culture Characteristics of Dermatophytes Isolated at a Tertiary Care Hospital in the Outskirts of. Int J Curr Microbiol App Sci. 2016;5(8):372-80. [Google Scholar]
- Shakthi R, Venkatesha D. Comparison of KOH, Calcofluor White and Fungal Culture for Diagnosing Fungal Onychomycosis in an Urban Teaching Hospital, Hyderabad. Int J Curr Microbiol App Sci. 2019;8(7):1420-5. [Google Scholar]
- Surendran K, Bhat R, Boloor R, Nandakishore B, Sukumar D. A clinical and mycological study of dermatophytic infections. Indian J Dermatol. 2014;59(3):262-7. [Google Scholar]
- Veer P, Patwardhan NS, Damle A. Study of onychomycosis: Prevailing fungi and pattern of infection. Indian J Med Microbiol. 2007;25(1):53-6. [Google Scholar]
- Bitew A. Dermatophytosis: Prevalence of Dermatophytes and Non-Dermatophyte Fungi from Patients Attending Arsho Advanced Medical Laboratory. Dermatol Res Pract. 2018. [Google Scholar] [Crossref]
Article Metrics
- Visibility 8 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.180-186
-
CrossMark
- Citation
- Received Date January 17, 2024
- Accepted Date August 10, 2024
- Publication Date March 12, 2025