Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

A comparative study of hemodynamic response following laryngoscopy and endotracheal intubation with direct Macintosh laryngoscope versus D-blade video laryngoscope intubation in patients undergoing general anesthesia
Abstract
Background: Laryngoscopy forms a crucial part of general anesthesia in obtaining a good visualization of the vocal cords for the facilitation of smooth endotracheal intubation. Direct laryngoscope visualization using Macintosh laryngoscope is best seen in the sniffing position. The recent generation C-MAC video laryngoscope poses a special D blade with greater curvature to facilitate intubation.
Aim and Objective: The primary objective of our study was to compare the hemodynamic responses during laryngoscopy and endotracheal intubation between Macintosh laryngoscopes and C-MAC D-blade video laryngoscopes. The secondary objective was focused on the duration of laryngoscopy, duration of intubation, total duration of intubation, and ease of intubation.
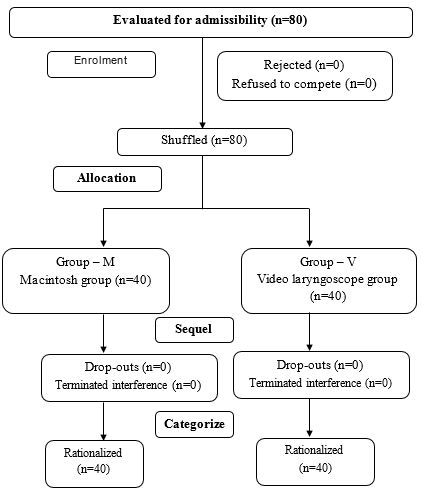
Material and Methods: Our study was a prospective randomized single-blinded study and is grouped as Group M (Direct laryngoscope group) and Group V (Video laryngoscope group). The randomization was done by computer-generated method and the differences between the groups were statistically analyzed with the Independent t-test for continuous variables and Pearson’s chi-square test for categorical variables.
Results: The hemodynamic stress response to laryngoscopy and intubation was less marked with D blade video laryngoscope when compared to Macintosh blade with statistical significance at 1 and 3 minutes (p=0.000 and 0.02 respectively) following tracheal intubation. Duration of laryngoscopy and intubation was lesser with D-blade video laryngoscope (p=0.0001 and 0.01 respectively). Better glottic visualization with minimal required extra lifting force and slight external laryngeal manipulations was noted in D blade video laryngoscope.
Conclusion: The D-blade video laryngoscope showed less hemodynamic response to endotracheal intubation along with better visualization of the glottis, less external laryngeal manipulation, and identical IDS score when compared to macintosh laryngoscope in general anesthesia for elective surgeries.
Introduction
The anesthesiologist’s primary role is to protect and maintain patent airway during anesthesia for adequate ventilation; which should be promptly established before irreversible injury.[1] Laryngoscopy forms a crucial part of general anesthesia in obtaining a good visualization of the vocal cords for facilitation of smooth endotracheal intubation and it also includes wide range of airway manipulations. [2]
Forces exerted by the laryngoscope blades on the tongue base and supraglottic region produce hemodynamic variations through reflex responses which manifest as tachycardia, hypertension, glottic closure, reflex bronchoconstriction, arrythmias, increased cerebral metabolic oxygen consumption rate, increased cerebral blood flow and increased EEG activity which might pose detrimental effects. [3]
Direct Macintosh laryngoscope visualization is best seen in sniffing position which improves the glottic view. [4] In recent days, video laryngoscopes are used for endotracheal intubation which facilitates the intubation performance by positioning the head in neutral position without altering the range of neck movements and also uses minimal force during intubation producing negligible airway response. [5]
The recent generation C-MAC D-blade video laryngoscope, the first Macintosh type video laryngoscope poses several distinguished improvements in the design of blade in its caudal end with an illumination source and cam device attached to a video input device providing the desired glottic view. [4] This video laryngoscope can hold and fit for Macintosh size blades 2, 3 & 4 and also helps in difficult airway situations. [6]
There are very limited studies confined to the evaluation of hemodynamic responses following video laryngoscopes guided endotracheal intubation and conventional Macintosh endotracheal intubation.
The primary objective of our study was to differentiate the plethysmograph responses during laryngoscopy and endotracheal intubation between Macintosh laryngoscopes and C-MAC D-blade video laryngoscopes. The secondary objective was focused on the period of laryngoscopy, time span of intubation, total extent of intubation, and simplicity of intubation.
Materials and Methods
Our prospective randomized single blinded study was carried out after obtaining Institutional human ethical committee clearance, registered in clinical trial registration of India (CTRI/2020/11/029369 dated 25.11.2020) and obtained informed written consent in the study participants in their vernacular language.
The sample size for the study was obtained with reference to Kanchi et al. [7] using the variable diastolic blood pressure taken at 3 minutes after endotracheal intubation, calculated using Zα-1.96 at 5% significance, Zβ-0.84 at 80% power and a value of 0.05 as significance. The required sample size by calculation was 35 in each group; but we considered 40 as sample size in each group for feasible study.
Inclusion criteria
80 patients of age group between 20 to 60 years belonging to both sexes and ASA 1 & 2, who were slated for scheduled surgery under inhalational anesthesia requiring direct laryngoscopy and airway management were included in the study.
Exclusion criteria
Patients with anticipated difficult intubation, obesity, pregnant mothers, cardiac, renal disease, uncontrolled hypertension, antihypertensives, antipsychotics, antiarrhythmics and emergency surgery were excluded in our study.
Procedure
The study population was distributed randomly into two categories of 40 each and lot casting was done by computer generated random method and the corresponding number was represented with the concerned group for the study. Our study population were grouped as Group M (Direct laryngoscope group) – Laryngoscopy performed with direct macintosh laryngoscope; Group V (Video laryngoscope group) – Laryngoscopy performed with C-Mac D-blade laryngoscope.
Routine pre-anesthetic evaluation including airway evaluation was done on the day prior to proposed procedure. Standard fasting guidelines followed and all the patients received Tablet Pantoprazole 40 mg and Tablet Metoclopramide 10 mg night before surgery and on the day of surgery 2 hour prior to induction as pre-medication. No benzodiazepine was given as pre-medication prior to surgery. On arrival inside the operating suite, 500 mL normal saline was started in the established 18gauge intravenous cannula, ASA standard pre induction monitors like pulse oximetry, five lead electrocardiogram, non-invasive blood pressure, temperature, EtCO2 and end tidal anesthetic agent concentration were connected and monitoring of these parameters started after noting the baseline values.
Airway assessment confirmed with modified Mallampati score and Cormack lehane grading at the time of intubation. After recording the baseline parameters, tidal volume pre-oxygenation was done for 3 minutes with 100% oxygen at 6 liters flow. Injection Fentanyl 2mcg/kg iv was given over 30 seconds followed by injection Propofol 2mg/kg dose for induction, ventilated using Atracurium 0.5mg/kg and intubated using appropriately sized cuffed endotracheal tubes.
Laryngoscopy was done using 3 or 4 size Macintosh blade in group M and D-blade video laryngoscope used in group V. The tube position was checked by presence of bilateral air entry by 5-point auscultation and confirmed by quantitative waveform capnography. Neither preservative free lignocaine nor pharmacological measures to attenuate the airway stress responses was used in our study. No surgical stimulus or any other stimulus was given to the patient from the time of pre-oxygenation till 10 minutes after induction of anesthesia. Anesthesia continued with oxygen and nitrous oxide in the ratio of 50:50, intermittent Atracurium relaxant and 2% Sevoflurane achieving MAC around 0.8 to 1.0. Patient was reversed from muscle relaxation using Neostigmine 0.05mg/kg iv and Glycopyrrolate 0.01mg/kg iv and proceeded for extubating meeting its criteria.
During intubation, the parameters like duration of laryngoscopy, intubation duration, glottic vision assessed using Cormack Lehane grading and POGO scoring, and the ease of securing the airway by intubation difficulty scale score were noted down in both the groups along with hemodynamic parameters.
Intubation Difficulty Scale (IDS) [8] assessed applying the following parameters;
Number of attempted intubations – Determined the attempts made during advancement of the endotracheal tube along the direction of the glottis in the course of direct laryngoscopy.
Numeral use of additional operant – Represents the number of extra persons straightly involved in intubation.
Number of changeable techniques executed – Deals with revision in equipment’s use with its adjuncts blade, endotracheal tube or inclusion of stylet.
Cormack Lehane grading – Addresses the glottic exposure.
Requirement of lifting force – Determine the bearing capacity applicable during laryngoscopy.
Requirement of laryngeal pressure – States the requirement to enhance required glottic visualization applying external laryngeal pressure.
Location of the vocal cord’s positions while intubating – Focus on the position of plica vocalis in abduction or adduction position during intubation.
POGO Score – Percentage of the glottic opening was noted.
Circulatory dynamics parameter monitored using the non-invasive arterial parameters which includes mean arterial blood pressure (MAP) derived from systolic and diastolic blood pressure (SBP & DBP), heart rate, SpO2 will be measured at baseline, preinduction, preintubation and postintubation at 1, 3 and 5 minutes.
Any complications such as apnoea and hypotension during this time frame were recorded. Hypertension and tachycardia defined as increase in blood pressure and heart rate more than 20% from baseline were managed with deepening the plane of anesthesia and supplementation of incremental doses of injection Esmolol at a dosage of 1.5mg/kg dosage. Hypotension was measured as drop in systolic blood pressure with a drop of 20% values from the reference point. Hypotension was managed with initial fluid bolus of 5mL/kg normal saline and further hypotension was treated with injection Mephentermine bolus of 6mg iv. Bradycardia (heart rate less than 45 beats per minute) was treated with injection atropine 0.12mg iv bolus.
Statistical analysis
All the data were entered in Excel 2019 and statistical assessment executed applying the statistical software, statistical package for social sciences (SPSS 22.0). Statistics were expressed as percentages and mathematical average values (with standard deviation). Disparity among the groups were analyzed applying Pearson’s chi-square test towards categorical variables and a two-sided unpaired t-test for continuous variables. The outcome was considered statistically significance when the p value showed less than the significance level 0.05.
Results
This randomized comparison was conducted on 80 patients with 40 participants in each group and majority of the study participants were in the peer group between 30-56 years with average age of 43.80, 42.40 in group M and group V respectively. Other demographic parameters like sex distribution of the individual, BMI, height, weight, and ASA grades were in the same class as among both the clusters [[Table 1]].
The hemodynamic stress response to laryngoscopy and insertion of an airway tube was less marked with D blade video laryngoscope in comparison with Macintosh blade with statistical significance at 1 and 3 minutes (p=0.000 and 0.02 respectively) following tracheal intubation [[Table 2]]. Duration of laryngoscopy (p=0.0001) and intubation (p=0.01) was lesser with D-blade video laryngoscope [[Table 3]]. Better glottic visualization with minimal required extra lifting force and slight external laryngeal manipulations was noted in D blade video laryngoscope (p=0.000) [[Table 4]].
|
Parameters |
Group M |
Group V |
p Value |
|
|
1. Age |
Mean in yrs. ± S. D |
43.80 ± 12.61 |
42.40 ± 12.27 |
0.616 |
|
2. Sex |
Male |
20 (50%) |
13 (32.5%) |
0.654 |
|
Female |
20 (50%) |
27 (67.5%) |
|
|
|
3. Weight |
Mean in kg ± S. D |
66.60 ± 9.56 |
68.00 ± 12.15 |
0.622 |
|
4. Height |
Mean in cm ± S. D |
161.90 ± 7.64 |
164.52 ± 7.53 |
0.087 |
|
5. BMI |
Underweight |
4 (10%) |
2 (5%) |
|
|
Normal |
21 (52.5%) |
21 (52.5%) |
0.673 |
|
|
Overweight |
15 (37.5%) |
17 (42.5%) |
|
|
|
6. ASA |
I |
5 (12.5%) |
14 (35%) |
0.018 |
|
II |
35 (87.5%) |
26 (65%) |
|
|
Parameter |
Duration |
Group M |
Group V |
p value |
|
1. Heart rate |
Baseline |
88.53±14.41 |
83.48±12.95 |
0.103 |
|
Pre-induction |
89.03±14.43 |
83.20±12.08 |
0.054 |
|
|
Pre-intubation |
84.55±10.71 |
83.43±10.08 |
0.630 |
|
|
1 min post-intubation |
93.68±13.05 |
86.45±13.88 |
0.019 |
|
|
3 mins post-intubation |
88.53±12.34 |
84.93±12.93 |
0.207 |
|
|
5 mins post- intubation |
81.50±12.28 |
81.20±13.76 |
0.918 |
|
|
2. SBP |
Baseline |
137.20±16.91 |
133.40±23.46 |
0.409 |
|
Pre-induction |
129.08±18.77 |
124.93±21.56 |
0.361 |
|
|
Pre-intubation |
111.58±17.09 |
106.23±18.93 |
0.189 |
|
|
1 min post-intubation |
137.18±24.32 |
117.43±19.59 |
0.000 |
|
|
3 mins post-intubation |
114.93±18.73 |
105.03±18.86 |
0.021 |
|
|
5 mins post- intubation |
103.23±18.54 |
97.05±15.51 |
0.110 |
|
|
3. DBP |
Baseline |
83.08±10.56 |
79.20±12.36 |
0.136 |
|
Pre-induction |
78.48±11.64 |
75.80±12.59 |
0.327 |
|
|
Pre-intubation |
73.95±14.40 |
71.80±16.12 |
0.269 |
|
|
1 min post-intubation |
87.25±17.38 |
73.78±14.07 |
0.000 |
|
|
3 mins post-intubation |
73.50±16.83 |
65.15±15.03 |
0.022 |
|
|
5 mins post- intubation |
66.18±13.61 |
61.05±13.56 |
0.096 |
|
|
4. MAP |
Baseline |
98.03±12.15 |
93.45±14.34 |
0.128 |
|
Pre-induction |
92.13±12.86 |
88.68±13.55 |
0.246 |
|
|
Pre-intubation |
84.85±14.79 |
81.25±15.98 |
0.962 |
|
|
1 min post-intubation |
101.33±19.62 |
85.35±14.93 |
0.000 |
|
|
3 mins post-intubation |
84.93±17.01 |
75.83±16.05 |
0.016 |
|
|
5 mins post- intubation |
76.98±14.82 |
70.98±13.66 |
0.064 |
|
|
5. SpO2 |
Baseline |
99.88±0.40 |
99.78±0.57 |
0.372 |
|
Pre-induction |
99.53±0.81 |
99.43±0.81 |
0.638 |
|
|
Pre-intubation |
99.97±0.18 |
100±0 |
0.321 |
|
|
1 min post-intubation |
99.93±0.25 |
100±0 |
0.155 |
|
|
3 mins post-intubation |
99.93±0.36 |
100±0 |
0.321 |
|
|
5 mins post- intubation |
99.97±0.18 |
100±0 |
0.321 |
|
Domains |
Group M |
Group V |
p Value |
|
1. Mallampatti distribution |
|
|
|
|
|
11 (27.5%) |
8 (20%) |
0.431 |
|
|
29 (72.5%) |
32 (80%) |
|
|
2. Cormack Lehane grading |
|
|
|
|
|
10 (25%) |
17 (42.5%) |
|
|
|
21 (52.5%) |
22 (55%) |
0.016 |
|
|
9 (22.5%) |
1 (2.5%) |
|
|
3. Ease of intubation |
|
|
|
|
Easy |
9 (22.5%) |
17 (42.5%) |
|
|
Slight difficulty |
30 (75%) |
23 (57.5%) |
0.112 |
|
Moderate to major difficulty |
1 (2.5%) |
0 (0%) |
|
|
4. Duration of Laryngoscopy (seconds) |
14.47 ± 3.55 |
12.15 ± 3.11 |
0.0001 |
|
5. Period of Intubation (seconds) |
13.85 ± 3.51 |
12.07 ± 3.23 |
0.010 |
|
6. Total duration of Intubation (seconds) |
28.32 ± 7.16 |
24.22 ± 6.34 |
0.639 |
|
Parameters |
Group M |
Group V |
p Value |
|
|
Lifting force |
Normal – 0 |
19 (47.5%) |
37 (92.5%) |
0.000 |
|
|
Increase - 1 |
21 (52.5%) |
3 (7.5%) |
|
|
Number of intubation attempts |
1st – 0 |
39 (97.5%) |
40 (100%) |
|
|
|
2nd – 1 |
1 (2.5%) |
0 (0%) |
0.314 |
|
Number of operators |
1 – 0 |
40 (100%) |
40 (100%) |
- |
|
Need of stylet |
Yes – 1 |
4 (10%) |
0 (0%) |
0.040 |
|
|
No – 0 |
36 (90%) |
40 (100%) |
|
|
Need for change of blade |
Yes – 1 |
1 (2.5%) |
0 (0%) |
0.314 |
|
|
No – 0 |
39 (97.5%) |
40 (100%) |
|
|
External laryngeal manipulation |
Yes – 1 |
27 (67.5%) |
7 (17.5%) |
0.000 |
|
|
No – 0 |
13 (32.5%) |
33(82.5%) |
|
|
Cormack Lehane grading |
1 |
10 (25.0%) |
17 (42.5%) |
|
|
|
2 3 |
21 (52.5%) 9 (22.5%) |
22 (55.0%) 1 (2.5%) |
0.016 |
|
POGO Score |
% |
84.1 (10.4) |
78.1 (10.4) |
0.047 |
Discussion
Laryngoscope blades of various sizes and shapes have been designed in such a way which can help in decreasing the hemodynamic responses and provide good laryngoscope view for smooth endotracheal intubation. [4] Ineffective respiration, wrong placement of tube in the esophagus and difficult tracheal intubation were the most common causes of unpleasant outcomes. [9]
The Macintosh blade’s curvature hinders the line of sight, the oral axis sets up an angle with the laryngeal axis and the epiglottis obscures the glottis, impeding the glottic view. [10] The use of C-MAC video laryngoscope favors the benefit of evading the alignment during advancement of the scope inside the oral cavity to visualize the laryngeal inlet structure for improved view of laryngoscopy. [11]
Minimizing the circulatory stress reactions during visualization of the larynx and airway support continues to be a major considerations and challenge for the anesthesiologists. Various methods have been tried for reducing the response which includes deep narcosis, local injectable anesthetics, opiate drugs, beta blockers, calcium channel blockers, clonidine, dexmedetomidine, gabapentin, nitroglycerin and laryngeal mask airway. [12]
In our study, the demographic parameters were analogous among both study groups. 30 to 55 years were the major age group involved in the study with no exponential significance in both the groups in terms of the age of the patients, sex, weight, height, and BMI except ASA of the patients with statistical significance (p = 0.018).
The arithmetic mean heart rate recorded at starting point, preinduction, preintubation, 3-minutes and 5-minutes post intubation were alike in both clusters. The mean heart rate at 1 minute after intubation was lower in group V in contrast to group M and was statistically relevant. This observation was in concordance with Hiteshi et al. [12] studies with significance; but in contrast to Kanchi et al. [7] studies, where there was no statistical significance in hemodynamic responses between the two groups in their study.
Hemodynamic stress response to laryngoscopy and intubation was lower pronounced with D blade video laryngoscope in contrast to macintosh; which was presumably due to the reduction in force necessary to obtain a clearer view of the larynx. [13] In our study we also noticed that D blade video laryngoscope intubation improves the laryngoscope view and also significantly attenuates the stress response.
The mean SBP was equivalent in both the clusters at baseline, preinduction, preintubation and post 5 minutes following intubation. The mean SBP at 1 minute after intubation and 3 minutes after intubation were lower in group V compared to 1 minute after intubation and 3 minutes after intubation in group M with statistical certainty. Our finding was in concordance with the Kanchi et al. [7] findings with decrease in MAP, SBP and DBP, but statistical significance was not noted in their study.
The mean DBP at baseline, preinduction, preintubation and 5 minutes after intubation were comparable in both group M and group V. The mean DBP at 1 minute after intubation and 3 minutes after intubation were lower in group V compared to 1 minute after intubation and 3 minutes after intubation in group M with statistical relevance p= 0.000 and p= 0.022 respectively. This finding in our study was similar to Hiteshi et al. [12] studies observing a significant statistical difference at 1,2,3,4 and 5th minute after intubation.
With regard to MAP, the parameters noted from baseline, preinduction, preintubation and 5 minutes after intubation were statistically insignificant. The mean MAP at 1 minute after intubation and 3 minutes after intubation were lower in group V in contrast to 1 minute after intubation and 3 minutes after intubation in group M with (p=0.000) and (p=0.016) respectively showing statistical significance. Sarkilar et al. [14] in contrast does not show any change in MAP between Macintosh and CMAC video laryngoscopes.
The number of performers in both the peers were alike. 52.5% in group M necessitated additional bearing force in comparison with 7.5% in group V; 67.5% required external laryngeal manipulation in group M compared to 17.5% in group V and were analyzed to be statistically relevant. Four patients in group M required stylet whereas none of the patients in group V required stylet for intubation and proved mathematical significance (p=0.040). There wasn’t statistical significance with regard to change of blade during intubation. In group M, CL grading 1,2,3 was noted in 10,21 and 9 patients respectively, where as in group V it was 17,22 and in 1 patient with CL grading 1,2 and 3 correspondingly with statistical significance (p=0.016).
Ease of intubation in group M was noted to be easy, slightly and moderately difficult in 9, 30 and in 1 patient respectively compared to 17 and 23 with no moderate difficulty in group V with statistical insignificance (p=0.112). In the current study the statistical power showed substantial reduction of Cormack lehane grading system while using CMAC laryngoscope, was analogous to the research by Maharaj et al studies. [15]
Fu-shan xue et al. [16] concluded C MAC video laryngoscope had a superior laryngoscopy view of larynx, enhanced success rate and shorter period of time than the direct laryngoscope. Similarly in our study C MAC video laryngoscope has lesser intubation time, 12.15 ± 3.11 seconds, when compared to direct laryngoscopes with 14.47 ± 3.55 seconds. Jungbauer et al. [11] described that video laryngoscopy as an alternative to direct laryngoscopy provides better in laryngoscope vision for endotracheal intubation, ease and faster in duration of intubation and lesser need for optimizing the maneuvers for intubation with higher rate of success and our study also showed similar results with statistical significance (p=0.0001).
Sarkilar et al. [14] concluded that there is no difference in hemodynamic responses on account of direct laryngoscopy and video laryngoscopy. In contrast in the present study the average airway management duration was pronounced lesser in video laryngoscope proportionate to direct laryngoscope. Stress response to airway was least pronounced with C-MAC video laryngoscope in contrary to Buhari and Selvaraj et al studies. [17]
Hansel et al. [18] showed that the video laryngoscopes may reduce the decreased unsuccessful intubation, augment the vocal cord visibility and may diminish the incidence of airway trauma which was in accordance with our study improving the glottic view for intubation.
Bhat et al. [19] concluded C-MAC takes smaller time frame than for intubations in lateral position. In our study C-MAC video laryngoscope takes less time than conventional laryngoscope. Rajasekhar et al. [20] showed as long as the anesthesia depth is constant the hemodynamic responses using McCoy or Macintosh or C-MAC laryngoscope for endotracheal intubation were statistically noteworthy (p˃0.05). In our study we did not monitor the depth of anesthesia but found statistical significance with SBP, DBP and MAP when compared to these studies.
The limitations of our study include institutional trial, requires larger sample size compared to smaller sample for better statistical significance and the induction techniques vary between other institutions.
Conclusion
The Macintosh type designed D blade video laryngoscope showed less hemodynamic response to endotracheal intubation along with better visualization of the glottis, less external laryngeal manipulation and identical IDS score when compared to normal macintosh type laryngoscope in general anesthesia for elective surgeries.
Ethical Approval
This study was approved by Institutional Ethical Review Board with ref. no. PSG/IHEC/2019/Appr/FB/041.
Source of Funding
The authors neither received support nor funding for the above study
Conflict of Interest
There is no conflict of interest
References
- Nadkarni M, Patel R, Behera P, Walzade A. Comparison of Macintosh, McCoy and Miller Laryngoscope Blades for Intubation- A Prospective Randomised Study. J Dent Med Sci. 2016;18(8):85-91. [Google Scholar]
- Arora S, Sayeed H, Bhardwaj N. A Comparison of Truview EVO2 Laryngoscope with Macintosh Laryngoscope in Routine Airway Management: A Randomized Crossover Clinical Trial. Saudi J Anaesth. 2013;7(3):244-8. [Google Scholar]
- Jain D, Bala I, Gandhi K. Comparative effectiveness of McCoy laryngoscope and CMAC(®) videolaryngoscope in simulated cervical spine injuries. J. Anaesthesiol. Clin. Pharmacol. 2016;32(1):59-64. [Google Scholar]
- Baliarsing L, Gore M, Akulwar P. Comparison of Glottis View and Hemodynamic Response by using Macintosh and MacCoy Laryngoscopes for Endotracheal Intubation in General Anaesthesia for Elective Surgery. Int J Contemp Med Res. 2016;3(8):2186-8. [Google Scholar]
- Hagberg C. Benumof and Hagberg's Airway Management: Third Edition. . 2013. [Google Scholar]
- Sabry L, Shaarawy S, Ellakany M, Elmasry A. Comparison between C-MAC D-blade and McCoy laryngoscopes in intubating patients during cervical immobilization. Res Opin Anesth Intensive Care. 2016;3(3):122-8. [Google Scholar]
- Kanchi M, Nair H, Banakal S, Murthy K, Murugesan C. Haemodynamic Response to Endotracheal Intubation in Coronary Artery Disease: Direct versus Video Laryngoscopy. Indian J Anaesth. 2011;55(3):260-5. [Google Scholar]
- Adnet F, Borron S, Racine S, Clemessy J, Fournier J, Plaisance P. The Intubation Difficulty Scale (IDS). Anesthesiology. 1997;87(6):1290-7. [Google Scholar]
- Cook T, Tuckey J. A Comparison between the Macintosh and the McCoy Laryngoscope Blades. Anaesthesia. 1996;51(10):977-80. [Google Scholar]
- Kulkarni A, Tirmanwar A. Comparison of Glottic Visualisation and Ease of Intubation with Different Laryngoscope Blades. Indian J Anaesth. 2013;57(2):170-4. [Google Scholar]
- Jungbauer A, Schumann M, Brunkhorst V, Börgers A, Groeben H. Expected Difficult Tracheal Intubation: A Prospective Comparison of Direct Laryngoscopy and Video Laryngoscopy in 200 Patients. Br J Anaesth. 2009;102(4):546-50. [Google Scholar]
- Aggarwal H, Kaur S, Baghla N, Kaur S. Hemodynamic Response to Orotracheal Intubation: Comparison between Macintosh, McCoy, and C-MAC Video Laryngoscope. Anesth Essays Res. 2019;13(2):308-12. [Google Scholar]
- Kaplan M, Hagberg C, Ward D, Brambrink A, Chhibber A, Heidegger T. Comparison of Direct and Video-Assisted Views of the Larynx during Routine Intubation. J Clin Anesth. 2006;18(5):357-62. [Google Scholar]
- Sarkılar G, Sargın M, Sarıtaş T, Borazan H, Gök F, Kılıçaslan A. Hemodynamic Responses to Endotracheal Intubation Performed with Video and Direct Laryngoscopy in Patients Scheduled for Major Cardiac Surgery. Int J Clin Exp Med. 2015;8(7):11477-83. [Google Scholar]
- Maharaj C, O’croinin D, Curley G, Harte B, Laffey J. A Comparison of Tracheal Intubation Using the Airtraq or the Macintosh Laryngoscope in Routine Airway Management: A Randomised, Controlled Clinical Trial. Anaesthesia. 2006;61(11):1093-9. [Google Scholar]
- Xue F, Li H, Liu Y, Yang G. Current Evidence for the Use of C-MAC Videolaryngoscope in Adult Airway Management: A Review of the Literature. Ther Clin Risk Manag. 2017;13:831-41. [Google Scholar] [Crossref]
- Buhari F, Selvaraj V. Randomized Controlled Study Comparing the Hemodynamic Response to Laryngoscopy and Endotracheal Intubation with McCoy, Macintosh, and C-MAC Laryngoscopes in Adult Patients. J Anaesthesiol Clin Pharmacol. 2016;32(4):505-9. [Google Scholar]
- Hansel J, Rogers A, Lewis S, Cook T, Smith A. Videolaryngoscopy versus Direct Laryngoscopy for Adults Undergoing Tracheal Intubation. Cochrane Database Syst Rev. 2022;4(4). [Google Scholar] [Crossref]
- Bhat R, Sanickop C, Patil M, Umrani V, Dhorigol M. Comparison of Macintosh Laryngoscope and C-MAC Video Laryngoscope for Intubation in Lateral Position. J Anaesthesiol Clin Pharmacol. 2015;31(2):226-9. [Google Scholar]
- Rajasekhar M, Yadav M, Kulkarni D, Gopinath R. Comparison of Hemodynamic Responses to Laryngoscopy and Intubation Using Macintosh or McCoy or C-MAC Laryngoscope during Uniform Depth of Anesthesia Monitored by Entropy. J Anaesthesiol Clin Pharmacol. 2020;36(3):391-7. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.187-193
-
CrossMark
- Citation
- Received Date October 08, 2023
- Accepted Date August 28, 2024
- Publication Date March 13, 2025