Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Long-term treatment outcomes in cervical cancer patients aged 60 years and above: A comprehensive 12-year study in the Indian context
Abstract
Background: Cervical cancer remains a significant global health concern, with around 570,000 new cases and 310,000 deaths annually. Despite a decrease in incidence due to screening programs, rates among elderly women, typically aged 50 and above have remained steady. These demographic faces unique physiological and pathological factors, impacting treatment decisions and outcomes. Treatment of Cervical cancer is a multimodality approach which includes Surgery, concurrent chemo radiation, brachytherapy and in some cases Neoadjuvant chemotherapy determined by staging. However, the suitability of these treatments for elderly patients, considering their frailty, co morbidities, and age-related issues like malnutrition and cognitive decline, remains underexplored. There's a critical need to balance treatment benefits with risks, aiming to reduce mortality by individualizing care.
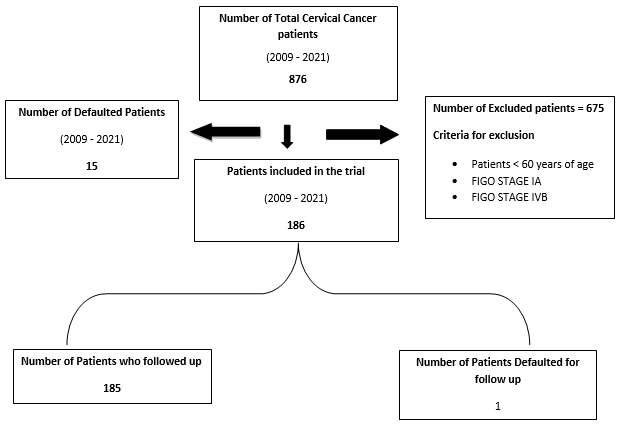
Materials and Methods: A retrospective study in India analyzed outcomes for elderly cervical cancer patients over 12 years. Out of 876 patients reviewed, 186 met inclusion criteria: aged 60 or older, with FIGO Stage IB to IVA and ECOG performance status I to III.
Results: The majority (61%) of patients were aged 60-65. Most had ECOG PS II status, and 96% had squamous cell carcinoma. Around 62.3% had locally advanced disease. Survival rates were highest in FIGO Stage IB, with overall survival statistically significant at 92.09 months, and disease-free interval at 103.24 months.
Conclusion: The study suggests age may not independently predict outcomes for elderly cervical cancer patients in India. Despite co morbidities necessitating treatment adjustments, radical management remains crucial, irrespective of age. Tailoring treatments to individual needs and improving survival prediction are essential for better outcomes in this population.
Introduction
Cervical cancer stands as one of the most commonly diagnosed malignancies afflicting women worldwide, with approximately 570,000 new cases emerging each year and an estimated 310,000 annual fatalities attributed to this disease.[1] While global efforts to implement various screening programs have brought about a decline in the incidence of cervical cancer, this decline has not been mirrored in the case of elderly females. [2] Disturbingly, statistics indicate that a substantial quarter of cervical cancer cases are diagnosed in the elderly age group. [3] A prior study has further substantiated these findings by revealing that the prevalence of cervical cancer is comparatively lower in women aged below 50 years, but as women surpass the age of 50, their risk of cervical cancer escalates by an annual 2% with each passing year. [4] Moreover, women aged 50 years and beyond typically find themselves in the perimenopausal or postmenopausal phase, leading to distinct disparities in their physiological and pathological characteristics when compared to women in their childbearing years. [5]
In light of these factors, a discernible trend of heightened concern for elderly patients grappling with cervical cancer has gradually emerged over time. The spectrum of treatment options for cervical cancer encompasses surgical interventions, brachytherapy and concurrent radio-chemotherapy, with the selection contingent upon the well-established FIGO staging. [6] However, the pivotal aspect of this equation—the intricate balance between treatment benefits and risks, particularly in the context of the elderly population—remains a domain that has not received adequate scrutiny. Decision-making for older females presents a multifaceted challenge, primarily owing to their frailty and the burden of multiple comorbidities such as diabetes or cardiac ailments. [7] These comorbidities hasten the deterioration of their health in tandem with age-related setbacks, including malnutrition, functional dependency and cognitive decline. Consequently, these patients face an elevated risk of adverse treatment effects. For these reasons, the landscape of cervical carcinoma treatment remains far from standardized within the geriatric population. Additionally, prognostic factors with the capacity to predict survival in cervical cancer patients aged 60 and beyond remain an area of limited investigation. [8]
The imperative thus lies in our pursuit of reducing mortality rates among elderly patients. Achieving this goal necessitates the development of prognostic tools for predicting survival, the identification of pertinent prognostic factors, and the formulation of tailored treatment strategies in response to the distinctive challenges posed by cervical cancer in elderly individuals.
With this objective in mind, this retrospective single-institutional study undertakes a comprehensive exploration, scrutinizing the outcomes of elderly patients diagnosed with cervical cancer within the context of the Indian scenario.
Materials and Methods
Patient selection
Over a span of 12 years, from 2009 to 2021, a total of 876 patients were initially presented with cervical cancer in the outpatient department. Out of this cohort, 186 patients satisfied the defined inclusion criteria. A detailed representation of the patient selection process is depicted in [Figure 1].
Inclusion criteria
Patients included in the study met the following criteria:
Diagnosis of cervical cancer
FIGO Stage IB to IVA
Age 60 years or older
ECOG performance status ranging from I to III
Exclusion criteria
Patients who fell under the following criteria were excluded from the study:
Age below 60 years
Metastatic cancer
FIGO Stage IVB
Demographic and clinico-pathological characteristics
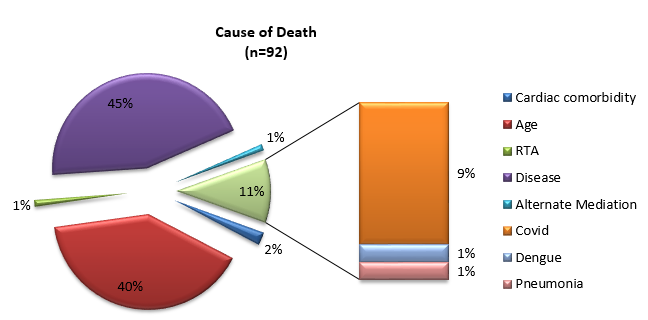
Patient demographics and clinico-pathological characteristics were comprehensively documented and are presented in [Table 1]. These characteristics encompassed ECOG performance status (I-III), FIGO Staging (IB-IVA), histo-pathological features (e.g., adenocarcinoma, squamous carcinoma, or adenosquamous carcinoma), radiotherapy and brachytherapy doses, overall survival, disease-free survival, current patient status (alive or deceased), and the cause of death if applicable.
Radiation therapy
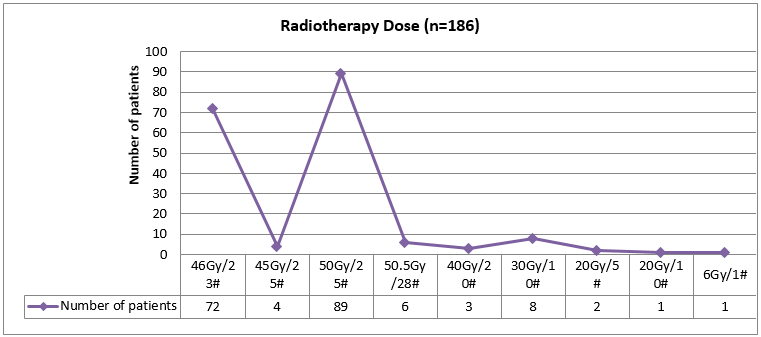
External beam radiation therapy, utilizing a 6 MV photon beam from a linear accelerator, was administered in varying doses, as illustrated in [Figure 2]. Following external beam radiation therapy, intracavitary brachytherapy to point A. Point A is defined as the point 2 cm above the distal end of the lowest source in the tandem and 2 cm lateral to the tandem A.
|
Characteristics |
Number of Patients |
Percentage (%) |
|
ECOG PS (n=186) |
|
|
|
• I |
2 |
1.07 |
|
• II |
167 |
89.78 |
|
• III |
17 |
9.10 |
|
Histopathology (n=186) |
|
|
|
• Squamous cell |
179 |
96.2 |
|
• Adenocarcinoma |
6 |
3.2 |
|
• Adenosquamous |
1 |
0.6 |
|
FIGO Stage (n=186) |
|
|
|
• IA |
5 |
2.68 |
|
• IIA |
19 |
10.21 |
|
• IIB |
46 |
24.73 |
|
• IIIA |
16 |
8.60 |
|
• IIIB |
51 |
27.41 |
|
• IIIC |
27 |
14.51 |
|
• IVA |
22 |
11.86 |
|
Radiotherapy dose (n=186) |
|
|
|
46Gy/23# |
72 |
38.70 |
|
• 45Gy/25# |
4 |
2.15 |
|
• 50Gy/25# |
89 |
47.89 |
|
• 50.5Gy/28# |
6 |
3.22 |
|
• 40Gy/20# |
3 |
1.61 |
|
• 30Gy/10# |
8 |
4.30 |
|
• 20Gy/5# |
2 |
1.07 |
|
• 20Gy/10# |
1 |
0.53 |
|
• 6Gy/1# |
1 |
0.53 |
|
Brachytherapy dose (n=186) |
|
|
|
• 9Gy |
55 |
29.56 |
|
• 7Gy |
74 |
39.78 |
|
• 9.5Gy |
5 |
2.68 |
|
• 6Gy |
5 |
2.68 |
|
• 5Gy |
2 |
1.11 |
|
• Not Received |
45 |
24.19 |
|
Boost Received (External Beam Radiotherapy) |
34 |
|
|
Response Assessment (n=185)* |
|
|
|
• Complete Response |
126 |
67.74 |
|
• Disease Recurrence |
28 |
15.05 |
|
• Residual Disease |
27 |
14.51 |
|
• Disease Progression |
4 |
2.15 |
|
Overall Survival (n=186) |
In months |
|
|
• Average |
63.3 |
|
|
• Maximum |
159 |
|
|
• Minimum |
2 |
|
|
Overall Survival (Stage wise) (n=186) |
In months |
|
|
• IB |
82.2 |
|
|
• IIA |
75.9 |
|
|
• IIB |
72.5 |
|
|
• IIIA |
65 |
|
|
• IIIB |
53.5 |
|
|
• IIIC |
26.53 |
|
|
• IVA |
20.28 |
|
|
Current Status (n=186) |
|
|
|
• Alive |
94 |
50.53 |
|
• Death |
92 |
49.47 |
|
Cause of Death (n=92) |
|
|
|
• Disease |
41 |
44.56 |
|
• Other causes |
51 |
55.44 |
Statistical analysis
Categorical variables were expressed as counts and percentages. Overall survival and disease-free survival were analyzed in the study population using the Kaplan–Meier approach. A significance level of p < 0.05 was employed for all statistical analyses.
Results
Patient characteristics
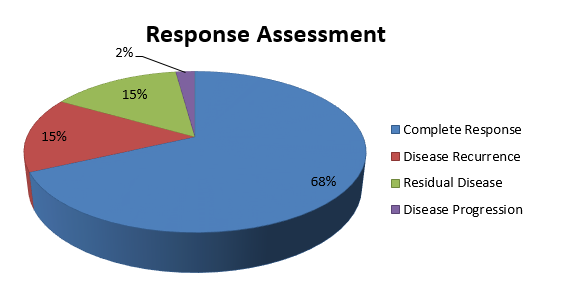
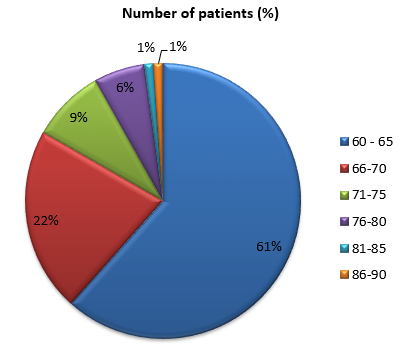
Out of a total of 876 cervical cancer patients presenting over a 12-year period (2009-2021), 186 patients met the inclusion criteria. The patient selection process is visually outlined in [Figure 1]. Detailed clinicopathological characteristics of the study population are documented in [Table 1]. The study population was age-standardized, revealing that 61% of patients belonged to the 60–65 years age group ([Figure 4]). The ECOG performance status analysis indicated that the majority of patients were classified under ECOG PS II ([Figure 5]). Among the 186 patients, 179 (96%) were histologically diagnosed with squamous cell carcinoma, while other histological types, such as adenocarcinoma, adenosquamous carcinoma, etc., were also considered ([Figure 6]). Approximately 62.3% of the population belonged to locally advanced stages (Stage III-IVA).
Response assessment
Response assessment was performed three months after the completion of chemo-radiotherapy followed by brachytherapy. The assessment utilized Recist 1.1 criteria.
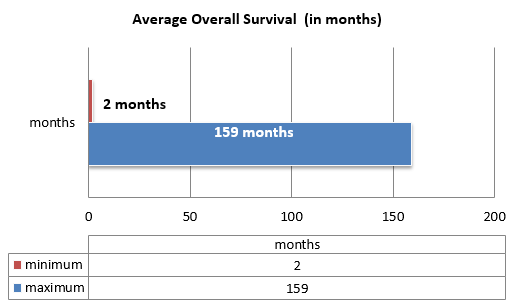
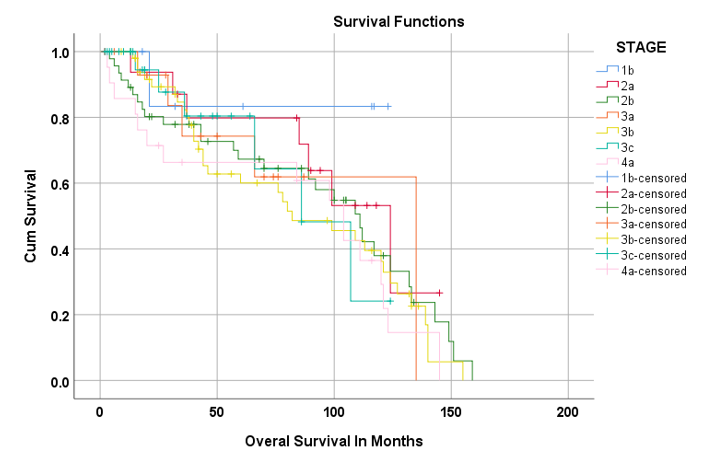
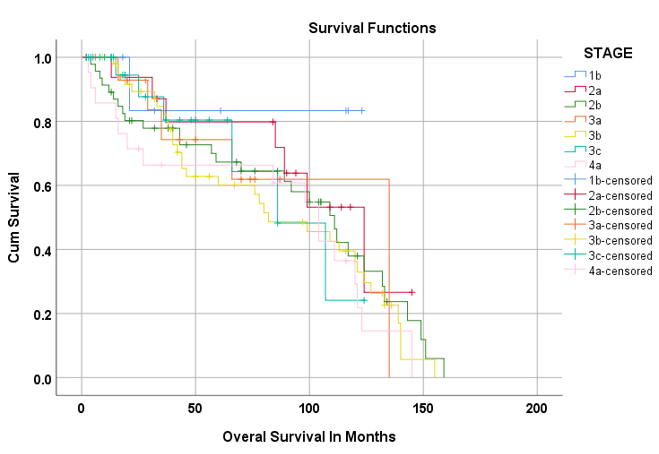
Survival analysis
Kaplan–Meier survival analysis was employed to assess overall survival and disease-free survival across different clinico-pathological characteristics within the cervical cancer patient population ([Figure 7], [Figure 8] ). The analysis showed that the maximum survival duration was 106.0 months in FIGO Stage IB patients compared to other stages. Overall survival was statistically significant at 92.09 months, with a 95% confidence interval ranging from 84.0 to 100.1 ([Table 2]). Similarly, the maximum disease-free interval was observed at 109.0 months in FIGO Stage IB, with an average disease-free interval of 103.24 months, significantly supported by a 95% confidence interval ranging from 85.42 to 122.08 ([Table 3]).
|
Treatment |
Average Survival Time in Month (Disease Cases) |
P-value |
||
|
Average |
95% Confidence Interval |
|||
|
Lower Bound |
Upper Bound |
|||
|
1b |
106.0 |
75.6 |
136.4 |
0.002 |
|
2a |
101.54 |
78.4 |
124.7 |
|
|
2b |
99.42 |
76.1 |
108.7 |
|
|
3a |
98.82 |
66.8 |
130.9 |
|
|
3b |
86.33 |
71.8 |
100.9 |
|
|
3c |
85.30 |
64.0 |
106.6 |
|
|
4a |
82.13 |
59.0 |
105.3 |
|
|
Overall |
92.09 |
84.0 |
100.1 |
[Table 2] is showing the Overall average Survival Time in month of the study population (n=186) . It is illustrated that the majority of survival was found 106.0 Months in FIGO IB as compared to other stages. The overall survival (in months) was 92.09months which was statistically significant with 95% Confidence Interval lower bound 84.0and upper bound 100.1in our study.
|
Treatment |
Average Survival Time in Month (Disease Free) |
P-value |
||
|
Average |
95% Confidence Interval |
|||
|
Lower Bound |
Upper Bound |
|||
|
1b |
109.0 |
75.58 |
136.42 |
0.004 |
|
2a |
106.24 |
65.72 |
122.76 |
|
|
2b |
104.76 |
61.21 |
132.32 |
|
|
3a |
98.55 |
61.95 |
121.15 |
|
|
3b |
95.63 |
65.45 |
105.82 |
|
|
3c |
91.07 |
61.61 |
106.54 |
|
|
4a |
83.25 |
49.78 |
96.71 |
|
|
Overall |
103.24 |
85.42 |
122.08 |
[Table 3] is showing the Disease free interval (in months) in the study population (n=186). It is illustrated that the maximum disease free interval was 109.0 month seen in FIGO Stage IB Stage, as compared to other stages and average disease free interval was 103.24 months which was significant with 95% Confidence Interval lower bound 85.42 and upper bound 122.08in our study.
Discussion
Cervical cancer is one of the most commonly diagnosed malignancies in women worldwide, with approximately 570,000 new cases diagnosed every year, leading to approximately 310,000 deaths annually. [1] In this study, which included 186 patients, 116 (62.3%) were diagnosed with stage III–IV disease. This indicates that a majority of older patients in our study presented with advanced-stage disease (62.3%) at the time of diagnosis. Notably, this percentage of patients with advanced-stage cervical cancer appears to be significantly higher than what is observed in large population studies.
While the global incidence of cervical cancer has been declining due to the implementation of various screening programs, the incidence among elderly females has remained unchanged. [9] The number of elderly patients being diagnosed with cervical cancer is on the rise worldwide, and elderly women now account for more than 40% of the deaths from cervical cancer. [10]
However, the impact of age on the survival of patients with cervical cancer remains uncertain. Some literature suggests that cervical cancer has a similar prognosis in both older and younger women. [11] Conversely, others have proposed that younger age is an unfavorable prognostic factor, particularly in more advanced stages of the disease. [12] In contrast, Wright et al. demonstrated that age is a poor prognostic factor for cervical cancer. [13] Furthermore, studies have indicated that younger patients may experience improved outcomes compared to older patients, and advanced age has been linked to decreased survival in various cancer types. [14]
Although large population-based studies have shown that survival for cervical cancer is inversely correlated with the stage of the disease, the survival among older women, regardless of the stage at diagnosis, has been reported to be worse than that of women in their 40s and 50s. [15] However, in our study, we did not observe a statistically significant difference in disease-free survival and overall survival. These findings align with a study conducted by Lindegaard et al., where age was not identified as a significant variable in any of the investigated endpoints. This conclusion was reached after reviewing radiotherapy treatment data from 114 women with a median age of 75.5 years. [16] Our study suggests that outcomes in older women may not be independently correlated with age alone.
Limitation of the study
Firstly, it has a retrospective study design, which may introduce biases. Secondly, the analysis of the data is confined to a single institution, which may limit the generalizability of the results. Additionally, we cannot exclude the possibility that other factors not considered in this study may be correlated with survival in cervical cancer patients. Further research is needed to better understand the complex relationship between age and survival in cervical cancer.
Conclusion
The study concluded that age may not be an independent risk factor for defining the outcome in cervical cancer patients in Indian Scenario. Even though elderly females may present with multiple co- morbidities, which may need alteration in the standard treatment protocol. However, the management of cervical cancer must have a radical approach irrespective of the age of the patient.
Source of Funding
None.
Conflict of Interest
None.
References
- . Cervical cancer. . . [Google Scholar]
- Altobelli E, Rapacchietta L, Profeta VF, Fagnano R. HPV-vaccination and cancer cervical screening in 53 WHO European Countries: An update on prevention programs according to income level. Cancer Med. 2019;8(5):2524-34. [Google Scholar]
- Quick A, Krok-Schoen J, Stephens J, JF. Cervical Cancer Among Older Women: Analyses of Surveillance, Epidemiology and End Results Program Data. Cancer Control. 2020;27(1). [Google Scholar] [Crossref]
- MM, Edosa K, Endashaw M, Bala E, Chaka E, Deriba B. Prevalence of Cervical Cancer and Associated Factors Among Women Attended Cervical Cancer Screening Center at Gahandi Memorial Hospital, Ethiopia. Cancer Inform. 10.1177/11769351211068431;11769351211068431. [Google Scholar]
- Sochocka M, Karska J, Pszczołowska M, Ochnik M, Fułek M, Fułek K. Cognitive Decline in Early and Premature Menopause. Int J Mol Sci. 2023;24(7). [Google Scholar] [Crossref]
- Todo Y, Watari H. Concurrent chemoradiotherapy for cervical cancer: background including evidence-based data, pitfalls of the data, limitation of treatment in certain groups. Chin J Cancer Res. 2016;28(2):221-7. [Google Scholar]
- Zullig L, Sung A, Khouri M, SJ, Shah N, Sitlinger A. Cardiometabolic Comorbidities in Cancer Survivors: JACC: CardioOncology State-of-the-Art Review. JACC Cardio Oncol. 2022;4(2):149-65. [Google Scholar]
- Xiu Y, Meng F, Wang Z, Zhao K, Wang Y, Chen Z. Prognostic factors for IB2-IIIB cervical cancer patients treated by radiation therapy with high-dose-rate brachytherapy in a single-institution study. J Contemp Brachytherapy. 2022;14(4):332-40. [Google Scholar]
- Neumeyer S, Tanaka L, Liang L, Klug S. Epidemiology of cervical cancer in elderly women: Analysis of incidence, treatment, and survival using German registry data. Cancer Med. 2023;12(16):17284-95. [Google Scholar]
- Gao Y, Ma J, Gao F, Song L. The evaluation of older patients with cervical cancer. Clin Interv Aging. 2013;8:783-8. [Google Scholar] [Crossref]
- MK, Rambeau A, Achkar S, Lecuru F, Mathevet P. Challenges and advances in cervix cancer treatment in elder women. Cancer Treat Rev. 2020;84. [Google Scholar] [Crossref]
- Ma J, Song L. The evaluation of older patients with cervical cancer. Clin Interv Aging. 2013;8:783-8. [Google Scholar] [Crossref]
- Wimberger P, Lehmann N, Kimmig R, Burges A, Meier W, Hoppenau B. Impact of age on outcome in patients with advanced ovarian cancer treated within a prospectively randomized phase III study of the Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group (AGO-OVAR). Gynecol Oncol. 2006;100(2):300-7. [Google Scholar]
- Frelaut M, Glas N, Zapardiel I, Kaidar-Person O, Kfoury M, You B. Are Older Patients with Cervical Cancer Managed Differently to Younger Patients? An International Survey. Cancers (Basel). 2019;11(12). [Google Scholar] [Crossref]
- Cooley J, Maguire F, Morris C, Parikh-Patel A, Abrahão R, Chen H. Cervical Cancer Stage at Diagnosis and Survival among Women ≥65 Years in California. Cancer Epidemiol Biomarkers Prev. 2023;32(1):91-7. [Google Scholar]
- JL, Thranov I, Engelholm S. Radiotherapy in the management of cervical cancer in elderly patients. Radiother Oncol. 2000;56(1):9-15. [Google Scholar]
Article Metrics
- Visibility 7 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.194-200
-
CrossMark
- Citation
- Received Date May 31, 2024
- Accepted Date January 29, 2025
- Publication Date March 13, 2025