Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Analysis of cervical cytology by conventional Pap smear at a tertiary care hospital in western Maharashtra
Abstract
Background: Cervical cancer is a major health problem and an important cause of mortality in women worldwide, particularly in developing countries. It is easily detectable and hence readily preventable disease. Cervical cytology helps to reduce significantly the incidence and mortality of cervical cancer.
Aim and Objectives: To study and categorize cervical cytology smears according to “The Bethesda system for reporting cervical cytology 2014”
Materials and Methods: This is an observational descriptive study, conducted in the Department of Pathology, in a tertiary care hospital from January 2016 to June 2020. A total of 1254 cervical cytology cases were studied. The clinical details were recorded from requisition forms. All the cervical cytology smears were of conventional preparation and were reported according to the Bethesda system for reporting cervical cytology 2014.
Results: The present study included patients in the age range 20 - 88 years. Cervical smears which were satisfactory for evaluation were 90.51% and unsatisfactory for evaluation were 9.49%. Negative for intraepithelial lesion or malignancy cases were 1074 and 61 cases were epithelial cell abnormalities. Atypical squamous cells cannot exclude high grade squamous intraepithelial lesion (ASC-H) [32.79%] was the most common epithelial cell abnormality. Out of 108 cervical cytology cases with available histopathological examination, 99 cases showed concordant findings and 9 cases showed discordant findings.
Conclusion: Cervical smear is an important, useful and simple tool for detection of precancerous lesions of cervix and should be used as a primary screening tool for early detection of cervical cancer.
Introduction
Cervical carcinoma is an important cause of mortality in the women worldwide. Cervical cancer is largely preventable disease and early-stage detection is associated with improved survival rate. The most effective way to screen for cervical cancer is to obtain smears from cervix (Pap smears).[1] This test not only plays a crucial role in the detection of cervical cancer and its precursor lesions but also aids in the diagnosis of other infective and inflammatory conditions. Pap smear (cervical smear) screening has sensitivity of 50%–75% and specificity of 98%–99%.[2]
Materials and Methods
The present study is an observational descriptive type of study conducted in the Department of Pathology at our institute over a period of four and half years i.e. January 2016 to June 2020. The retrospective data was collected from 1st January 2016 to 30th October 2018 and the prospective data was collected from 1st November 2018 to 30th June 2020.
Inclusion criteria
All cervical smears included in our study from 1st January 2016 to 30th June 2020 from the patients who are willing to provide written informed consent are included.
Study setting
Detailed history was taken and particulars regarding age, clinical presentations, per speculum and per vaginal examination findings were recorded. One or two slides of cervical cytology smears were received from all the patients. All the slides were labelled with a glass marker. The smears were fixed in methanol for 30 minutes. Rapid Pap stain and / or Haematoxylin and eosin (H & E) staining were done. All the slides were mounted with DPX. Light microscopic examination was done. The findings were interpreted according to the Bethesda system for reporting cervical cytology 2014. [3]
Results
A total of 1254 cervical cytology smears with age range of 20-88 years were studied. Majority of the women in the present study were in the age group of 31- 40 years. The mean age was 43.28 years. Out of 1254 women, 1211(96.57%) were parous and 43 women (3.43%) were nulliparous. Many patients presented with more than one symptom. Per vaginal discharge was the most common symptom followed by pain in abdomen and menstrual irregularities. On per speculum examination, majority of the women had healthy cervix i.e 524 cases [41.79 %]. White discharge was found in 18.18 % of the cases. Cervix bleeding on touch was found in 31 (2.47 %) patients. Cervical growth was noted in 9 cases accounting for 0.72%.
On per vaginal examination, most of the patients [572, (45.61%)] had normal sized, anteverted uterus and fornices were free and non-tender followed by bulky anteverted uterus with fornices free and non-tender in 211 cases (16.83%).
Out of 1254 cervical cytology smears, 1135 cervical smears were satisfactory and 119 cervical smears were unsatisfactory for evaluation. Most of the cervical smears (69 cases) were unsatisfactory due to scant cellularity followed by obscuring inflammation (28 cases).
Out of 1135 satisfactory cervical cytology smears, 1072 (94.45 %) cervical smears were Negative for intraepithelial lesion or malignancy (NILM), two (0.18 %) cervical smears belonged to general category Other - NILM with endometrial cells and 61 (5.37 %) cervical smears were of epithelial cell abnormalities ([Table 1]).
Out of 1072 NILM cervical smears, 22.82% cervical smears showed NILM with other non-neoplastic findings, 2.52% cases showed presence of organisms while NILM with other i.e. endometrial cells was noted in two (0.19%) cases which were found in the age group of 41-50 years and 61-70 years respectively ([Table 2]).
Most common age group was 31-40 years age group followed by 21-30 years. 87.99% women with NILM cervical smear were multiparous, 8.75% women were primiparous and 3.35% were nulliparous. The most frequent clinical presentation of patients with NILM cervical smears was per vaginal discharge (406) followed by pain in abdomen (349) and menstrual irregularities (191). On per speculum examination, most of the cases of NILM showed healthy cervix (473 cases, (44.04%)) followed by white discharge (194 cases, (18.06%)).
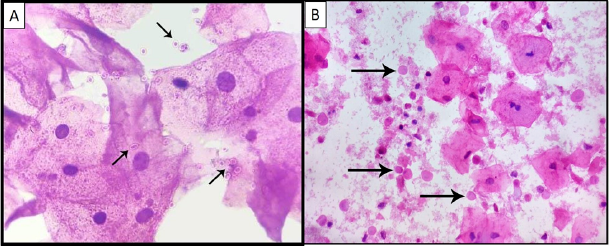
Out of 30 cases of NILM with organisms, fungal organisms morphologically consistent with candida species was the most common lesion. White discharge was the most common per speculum finding in infectious conditions like candida while foul-smelling discharge was common in infection caused by trichomonas vaginalis.
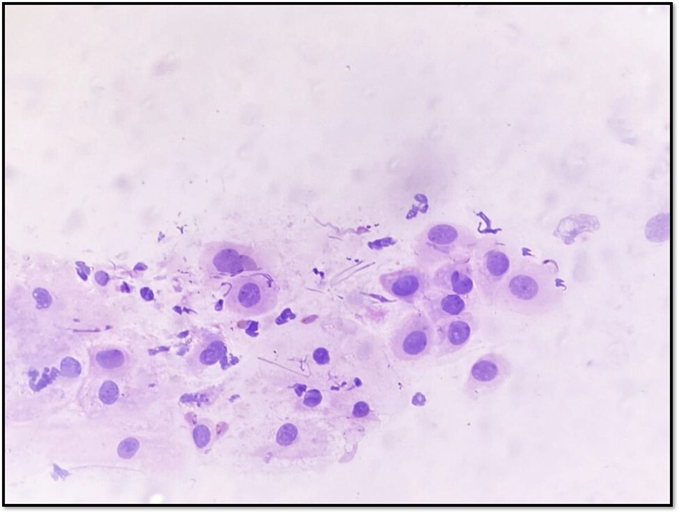
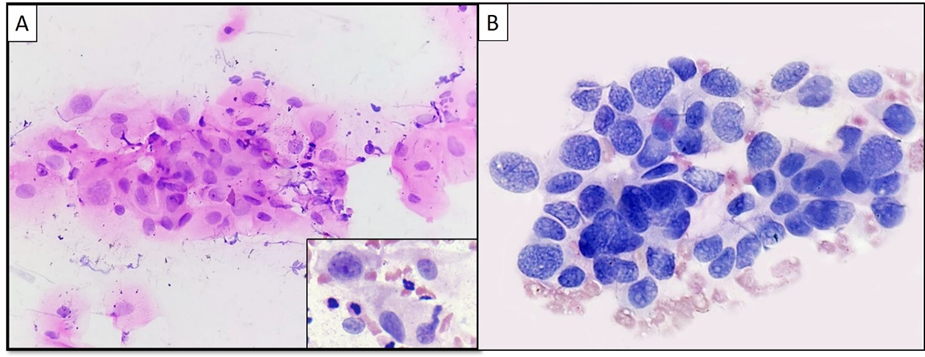
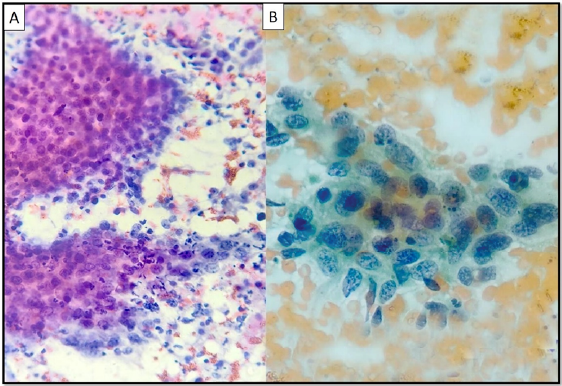
Out of 61 cases of epithelial cell abnormalities, 58 cases (95.08%) showed squamous cell abnormalities whereas 3 cases (4.92%) showed glandular cell abnormalities. ([Table 3]) Most of the epithelial abnormalities were seen in the age group of 41-50 years (19 cases, 31.15%) followed by 51-60 (12 cases,19.67 %). Most of the patients showing epithelial cell abnormalities on cervical smears i.e. 56(91.80%) were multiparous.
ASC-H was the most common finding which was seen in 20 out of 61 cases. The most common age group of ASC-H was 41-50 years followed by 31-40 years. The most common clinical presentation in ASC-H was per vaginal bleeding
The mean age of patients with LSIL, HSIL and HSIL with features suspicious for invasion was 43.5 years, 56.83 years, 52.5 years respectively. The age range of patients with squamous cell carcinoma was 42-80 years with mean age of 60.45 years.
Patients with glandular cell abnormalities like atypical endocervical cells, not otherwise specified (NOS) was in the age range of 28-47 years with mean age of 37.5 years. There was a single case of atypical glandular cell - favour neoplastic, in a 56 years old woman.
The most common per speculum finding of the patients showing epithelial cell abnormalities on cervical smears was white discharge (14 cases, 22.95%) followed by cervix bleeding on touch and healthy cervix in equal frequency (12 cases, 19.67%).
Out of 1254 cervical smears in the present study, 63 patients (5.02%) were HIV positive and rest of the patients (1191, 94.98%) were HIV negative. Majority of the HIV positive patients were in the age group of 31-40 years (42.86%) followed by 41-50 years (41.27%). Out of 63 HIV positive cases, 13 (20.63%) cases had epithelial cell abnormalities, 43 (68.25%) cases were interpreted as NILM and seven (11.11%) cases were reported as unsatisfactory for evaluation. The cytology findings of HIV positive cases are given in [Table 4].
Out of 108 cervical cytology cases with available histopathological examination, 99 cases showed concordant findings and 9 cases showed discordant findings. Ninety-three cases of NILM and 15 cases of epithelial cell abnormalities had histopathological examination. Majority of the cases i.e. 92 reported as NILM on cytology were reported as cervicitis (chronic or acute on chronic) and papillary endocervicitis on histopathology.
One case of NILM with endometrial cells in a woman aged 62 years on cervical cytology was reported on histopathology as endometrial carcinoma. One case of ASCUS on cytology was reported as papillary endocervicitis on histopathology. Two cases of ASC-H were reported as SCC on histopathology. One case of ASC-H was reported as endometrial carcinoma on histopathology. The clusters of small cells showing nuclear atypia on cytology were misinterpreted as that of metaplastic type cells rendering the diagnosis of ASC-H. One case of LSIL and two cases of HSIL were upgraded to SCC on histopathology. Six cases of SCC were concordant on histopathology as SCC. One case of HSIL with features for invasion on cervical smear cytology was reported as suspicious for malignancy on histopathology as well. Atypical glandular cell favour neoplastic was reported as papillary endocervicitis on histopathology.
Sensitivity of cervical cytology in the present study was 50 %, specificity was 97.87 %, positive predictive value was 77.77 % and negative predictive value was 92.92 %. Diagnostic accuracy was 91.66%.
|
Cytology categorization |
Number of cases |
Percentage (%) |
|
1. Negative for intraepithelial lesions or malignancy (NILM) |
1072 |
94.45% |
|
2. Other – NILM with endometrial cells |
02 |
0.18% |
|
3. Epithelial cell abnormalities |
61 |
5.37% |
|
Total |
1135 |
100% |
|
Interpretation |
Number of cases |
Percentage (%) |
|
A - Negative for intraepithelial lesion or malignancy (NILM) |
798 |
74.21% |
|
B - NILM with associated non neoplastic findings – (n- 244 cases, 22.82 %) |
||
|
I) Non-neoplastic cellular variation - a. Squamous metaplasia |
221 |
20.67 % |
|
b. Atrophy |
18 |
1.68 % |
|
c. Keratotic changes |
2 |
0.19 % |
|
II) Reactive cellular changes associated with inflammation |
3 |
0.28 % |
|
C - NILM with Organisms - (n – 30 cases, 2.52 %) |
||
|
i) Trichomonas vaginalis |
8 |
0.74 % |
|
ii) Fungal organisms morphologically consistent with candida |
19 |
1.77 % |
|
iii) Shift in flora suggestive of bacterial vaginosis |
3 |
0.28 % |
|
D - NILM with Other - Endometrial cells |
2 |
0.19 % |
|
Total |
1074 |
100% |
|
Interpretation - Epithelial cell abnormalities |
Number of cases (%) |
Age range |
Mean age |
Parity (Number of cases) |
||
|
|
|
|
|
Nulli |
Primi |
Multi |
|
I. Squamous cell |
||||||
|
A) Atypical squamous cells |
||||||
|
1. Of undetermined significance |
13(21.31%) |
25-67 |
47.53 |
- |
2 |
11 |
|
2. Cannot exclude HSIL |
20(32.79%) |
30-86 |
54.95 |
- |
- |
20 |
|
B) Low grade squamous intraepithelial lesion |
6(9.84%) |
34-55 |
43.5 |
- |
1 |
5 |
|
C) High grade squamous intraepithelial lesion (HSIL) |
||||||
|
1. HSIL |
6(9.84%) |
45-68 |
56.83 |
- |
- |
6 |
|
2. HSIL with features suspicious for invasion |
2(3.28%) |
48-57 |
52.5 |
1 |
- |
1 |
|
D) Squamous cell carcinoma |
11(18.03%) |
42-80 |
60.45 |
- |
- |
11 |
|
II. Glandular cell – |
||||||
|
1. Atypical endocervical cells-NOS |
2(3.28%) |
28-47 |
37.5 |
1 |
- |
1 |
|
2. Atypical glandular cells - favor neoplastic |
1(1.64%) |
56 |
- |
- |
- |
1 |
|
Total |
61(100%) |
2(3.28%) |
3(4.92%) |
56(91.80%) |
|
General category |
Interpretation |
No of cases |
Percentage (%) |
|
Negative for intraepithelial lesion or malignancy (n-43, 68.25%) |
NILM |
33 |
52.38% |
|
NILM with squamous metaplasia |
6 |
9.52% |
|
|
NILM with organisms - candida |
4 |
6.35% |
|
|
Epithelial cell abnormalities (n-13, 20.63%) |
ASC-US |
2 |
3.17% |
|
ASC-H |
5 |
7.94% |
|
|
LSIL |
3 |
4.76% |
|
|
HSIL |
1 |
1.59% |
|
|
SCC |
2 |
3.17% |
|
|
Unsatisfactory (n-7,11.11%) |
Obscuring inflammation |
3 |
4.76% |
|
Scant cellularity |
4 |
6.35% |
|
|
Total |
63 |
100% |
|
Interpretation |
Umarani et al (2016) |
Rana et al (2018) |
Ajmera et al (2019) |
Zubair et al (2019) |
Present study |
|
% (cases) |
% (cases) |
% (cases) |
% (cases) |
% (cases) |
|
|
Epithelial cell abnormalities |
|
|
|
|
|
|
I. Squamous cell |
|
|
|
|
|
|
A) Atypical squamous cells |
|||||
|
1. ASC-US |
56.56 (69) |
50 (3) |
52.94 (9) |
35.03 (18) |
21.31(13) |
|
2. ASC-H |
6.56(8) |
- |
- |
- |
32.79 (20) |
|
B) LSIL |
18.85 (23) |
33.33 (2) |
11.76 (2) |
39.2 (20) |
9.84 (6) |
|
C) HSIL |
|||||
|
1. HSIL |
7.38 (9) |
16.67 (1) |
5.88 (1) |
13.7 (7) |
9.84 (6) |
|
2. HSIL –SFI |
- |
- |
- |
- |
3.28 (2) |
|
D) SCC |
3.28 (4) |
- |
23.53 (4) |
2 (1) |
18.03 (11) |
|
II. Glandular cell |
|
|
|
|
|
|
A. AEC-NOS |
- |
- |
- |
- |
3.28 (2) |
|
B. AGC-NOS |
7.38 (9) |
- |
- |
9.8 (5) |
- |
|
C. AGC-FN |
- |
- |
- |
- |
1.64%(1) |
|
III. Adenocarcinoma |
- |
- |
5.88 (1) |
- |
- |
|
No other findings |
- |
- |
- |
1.92 (1) |
- |
|
Total |
100 (122) |
100 (6) |
100 (17) |
100 (51) |
100 (61) |
|
General category |
Madan et al (2016) |
Kusumam et al (2016) |
Present study |
|
|
% (No. of cases) |
% (No. of cases) |
% (No. of cases) |
||
|
NILM |
NILM |
76.71% (191) |
88.00 % (88) |
61.90% (39) |
|
|
Candida |
2.41% (6) |
- |
6.35% (4) |
|
|
BV |
2.01% (5) |
- |
- |
|
|
TV |
1.61% (4) |
- |
- |
|
|
Atrophy |
0.80% (2) |
- |
- |
|
ECA |
ASCUS |
4.42% (11) |
1 % (1) |
3.17% (2) |
|
|
ASC-H |
1.61% (4) |
- |
7.94% (5) |
|
|
LSIL |
2.01% (5) |
9% (9) |
4.76% (3) |
|
|
HSIL |
2.81% (7) |
- |
1.59% (1) |
|
|
SCC |
0.80% (2) |
2% (2) |
3.17% (2) |
|
Unsatisfactory |
4.82% (12) |
- |
11.11% (7) |
|
|
|
- |
- |
||
|
Total |
100% (249) |
100% (100) |
100% (63) |
Discussion
Cervical cancer is the fourth most common female cancer in the world. Aside from the Human Papillomavirus (HPV), which is responsible for up to 70% of cases, various genetic and epigenetic variables have been linked to the development of cervical cancer. [4] Pap Smear is a simple and cost-effective screening test for early diagnosis of premalignant and malignant cervical lesions. It is widely used as a cervical cytology screening method due to its ability to detect precursor lesions of cervical cancer, low cost and feasibility.
In the present study, the highest frequency of cervical cytology smears was noted in the age group of 31- 40 years- 400 cases (31.90 %) which is similar to the observations in the study conducted by Umarani et al. [5] 464 (33 %), Das et al. [6] 1671 (33.25 %), Sarvaiya et al. [7] 147 (33.79%) and Zubair et al. [8] 212 (36.68%).
In the present study, maximum number of patients were multiparous (1105 women, 88.11%) followed by primipara (106, 8.45 %). Similar observations were found in studies done by Kour et al. [9] 108 (90.00 %), Mhaske et al. [10] 435 (94.16 %), Verma et al.[11] 179 (89.5 %) and Mishra et al. [12] 167 (83.5 %). In our study, per vaginal discharge was the most common clinical presentation noted in 472 cases. In studies done by Shekhar et al. [13], Shaki et al. [14], Mishra et al. [12], Korade et al. [15] and Sarvaiya et al. [7] also, per vaginal discharge was the commonest clinical presentation.
The unsatisfactory cytology reported by various studies was, Sachan et al. [16] 6.42%, Madan et al. [17] 4.80%, Singh et al. [18] 3.4% and Vedvathi et al. [19] 2%. In our study, the unsatisfactory rate was 9.49%. This may be due to larger sample size, or technical error while collecting the smear or women having more inflammation at presentation. Liquid based cytology can reduce the rate of unsatisfactory smears, but it is costly and not feasible in low resource settings.
Frequency of NILM and epithelial cell abnormalities were comparable with studies done by Gupta et al. [20] and Rawat et al. [21] The percentage of NILM with endometrial cell in the present study (0.19 %) was comparable with study done by Zubair et al. (0.20%). [8] This may be due to increased awareness among the women regarding the importance of cervical cancer screening in the target population.
Candidiasis (19 cases, 63.33%) was the most common finding among the inflammatory NILM cytology smears in the present study which was similar to study done by Mulay et al. [22] (182 cases, 50%), Rana et al. [23] (28 cases, 49.12%) and Tailor et al. [24] (53 cases, 82.81%) whereas the most common organism in the study done by Pun et al. [25] was bacterial vaginosis. Most of the candidiasis cases i.e. 9 (30%) in the present study were noted 31-40 years age group. Similar findings were noted in study done by Rana et al.[23] with a frequency of nine (15.79%). Four cervical smears with trichomonas vaginalis (13.33%) were seen in the age group of 31-40 years which is similar to the observation noted by Rana et al. [23]
In the present study 13 (21.31%) cases of ASCUS were noted which was similar to the findings noted in Zubair et al. [8] while Rana et al., [26] Ajmera et al. [27] and Umarani et al. [5] observed it to be higher. This may be explained by variation in population under consideration or due to subjective variation in application of ASCUS criteria early in these lesions.
LSIL was seen in 9.84% cervical smear cases in the present study which is comparable with Ajmera et al. [27] Umarani et al., [5] Rana et al. [26] and Zubair et al. [8] reported a higher frequency of LSIL in their studies (18.85%, 33.33% and 39.2% respectively).
In our study, HSIL was noted in 9.84% of cervical smear cases which was comparable with Umarani et al. [5] while other studies done by Rana et al. [26] and Zubair et al. [8] showed higher HSIL cervical smear cases and Ajmera et al. [27] showed slightly lower HSIL cervical smear cases.
SCC was noted in 18.03% of cervical smear cases in present study which is comparable with that of Ajmera et al. [27] Umarani et al. [5] and Zubair et al. [8] observed lower SCC cervical cytology cases in their study. The probable reason for higher rate of malignancies in the present study was due to the late presentation of the patients.
Findings of atypical endocervical cells not otherwise specified and atypical glandular cells favour neoplastic were noted in the present study, these were not seen in other studies done by Rana et al.,[26] Ajmera et al.[27] and Zubair et al.[8]
Most of the patients with LSIL were from the age group of 34-55 years which is comparable to the study done by Zubair et al. [8] with 31-77 age range of years. The mean age of LSIL in present study was 43.5 years which is higher than that of Rawat et al. [21] (39.5 years) and lower than that of Zubair et al (51.5 years).[8]
The age range for HSIL in the present study was 45-68 years which is comparable to the study done by Zubair et al. [8] with age range of 47-70 years. The mean age of patients with HSIL in present study was 56.83 years which correlated with similar finding in the study done by Zubair et al. (56.3years). [8] Rawat et al.[21] showed lower mean age of HSIL than the present study (51.5 years)
In the present study, patients with SCC on cervical cytology smears were from the age range of 34-55 years. The mean age of SCC in present study was 43.5 years. Single case of SCC was found in the study done by Zubair et al.[8] with 50 years of age. Mean age of patients with SCC in Rawat et al., study was 64.6 years. [21]
Out of 1254 cervical smear cases studied, 63 were HIV positive cases and 1191 were HIV negative. Majority of the cases were NILM (61.90%) which is similar to the studies by Madan et al. [17] and Kusumam et al. [28]
In the present study, 20.63% HIV positive patients had epithelial abnormalities and 11.11 % of the HIV positive patients showed unsatisfactory smear which is higher than the study done by Madan et al.,(12 % and 4.80% respectively). [17]
Among epithelial cell abnormalities, in the present study ASC-H was noted in 7.94% cases which is higher than that seen in study by Madan et al. [17] In the study by Madan et al., ASCUS was the most common finding constituting to 4.42 % which is higher than our study. [17] The comparison of cytology findings of various studies in HIV positive cases is summarised in [Table 6].
The sensitivity and specificity reported in various studies were 65-76%. [29], [30], [31] In the present study, sensitivity and specificity of cervical cytology were 50% and 97.87% respectively. In the present study, the screening error may be due to presence of very few atypical cells in smears, clusters of atypical cells embedded in abundant inflammatory infiltrates, subjective error in interpretation and inadequate sampling. The sensitivity of pap smears can be improved by co- testing with HPV DNA and serial cervical cytology as per recommendations. All abnormal cytology cases should do colposcopy guided biopsies.
The positive predictive value and the negative predictive value in various studies ranged from 82-96% and 71-86% respectively. [29], [30], [31] The positive predictive value and negative predictive value of the present study was 77.77 % and 92.92 %. The overall diagnostic accuracy in our study was 91.66 % which is higher than other studies which showed diagnostic accuracy of 80-89%. [29], [30], [31] This study shows a good correlation between cervical cytology smear and cervical histopathology.
Conclusion
Our study highlights the role of conventional cervical cytology smears with 2014 Bethesda system of reporting cervical cytology as an important screening tool for carcinoma cervix. Screening of cervical cancer can detect pre-invasive lesions and timely intervention can be done to prevent development of invasive cervical cancer. But knowledge regarding cervical cancer and it’s screening is poor in the general society. It is therefore important that there should be awareness programme and educational activities for cervical cancer screening in order to reduce morbidity and mortality associated with cervical cancer.
Source of Funding
None.
Conflict of Interest
None.
References
- Naki M, Kose F. Cervical premalignant lesions and their management. J Turk Ger gynecol Assoc. 2014;15(2):109-21. [Google Scholar]
- Aswathy S, Quereshi M, Kurian B, Leelamoni K. Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. Indian J Med Res. 2012;136(2):205-10. [Google Scholar]
- Pangarkar M. The Bethesda System for reporting cervical cytology. Cytojournal. 2015;19. [Google Scholar] [Crossref]
- Hoque M, Haque E, Karim M. Cervical cancer in low-income countries: A Bangladeshi perspective. Int J Gynaecol Obstet. 2021;152(1):19-25. [Google Scholar]
- Umarani M, Gayathri M, Kumar M. Study of cervical cytology in Papanicolaou (Pap) smears in a tertiary care hospital. Indian J Pathol Oncol. 2016;3(4):679-83. [Google Scholar]
- Das D, Kar A, Rath S, Baliarsingh S, Prusty D, Dash AK. Cytological pattern of papanicolaou smears and detection of cervical cancers: An experience from a tertiary care centre of eastern zone of India. Oncol J India. 2018;2(2):25-8. [Google Scholar]
- Sarvaiya A, Chauhan S. Cervical smear cytopathological study in a tertiary care centre. Int J Clin Diagn Pathol. 2019;2(1):236-8. [Google Scholar]
- Zubair A, Kulkarni S, Preethi M. Cytomorphological patterns of cervical Papanicolaou smear abnormalities based on 2014 Bethesda System in North Karnataka region. Trop J Path Micro. 2019;5(5):251-9. [Google Scholar]
- Kour P, Lal M, Panjaliya R, Dogra V, Gupta S. Study of the Risk Factors Associated with Cervical Cancer. Biomed Pharmacol J. 2010;3(1). [Google Scholar]
- Mhaske M, Jawadekar S, Saundale S. Study of association of some risk factors & cervical dysplasia/cancer among rural women. National J Community Med. 2011;2(2):209-12. [Google Scholar]
- Verma A, Verma S, Vashist S, Attri S, Singhal A. A study on cervical cancer screening in symptomatic women using Pap smear in a tertiary care hospital in rural area of Himachal Pradesh, India. Middle East Fertility Soc J. 2017;22(1):39-42. [Google Scholar]
- Mishra P, Thapa R, Dinkar A. A study on cervical cancer screening using pap smear in urban area in state of Meghalaya, India. Int J Reprod Contracept Obstet Gynecol. 2018;7(8):3113-6. [Google Scholar]
- Shekhar H, Pancharia A, Chauhan S, Kaur A, Chauhan S. Cytological pattern of cervical Papanicolaou smear in Rajasthan: a screening and diagnostic procedure. Int J Dent Med Res. 2014;1(3):1-7. [Google Scholar]
- Shaki O, Chakrabarty B, Nagaraja N. A study on cervical cancer screening in asymptomatic women using Papanicolaou smear in a tertiary care hospital in an urban area of Mumbai, India. J Family Med Prim Care. 2018;7(4):652-7. [Google Scholar]
- Korade ST, Birare SD. Cytopathological study of lesions of uterine cervix by papanicolaou smear: A two-year study. Int J Pathol. 2019;11(2):95-8. [Google Scholar]
- Sachan P, Singh M, Patel M, Sachan R. A study on cervical cancer screening using pap smear test and clinical correlation. Asia Pac J Oncol Nurs. 2018;5(3):337-41. [Google Scholar]
- Madan A, Patil S, Nakate L. A Study of Pap Smear in HIV-Positive Females. J Obstet Gynaecol India. 2016;66(6):453-9. [Google Scholar]
- Singh S, Nnadi D, Anas R, Ango I, Umar A, Mohammed U. Cervical Cytology: A Review of 597 Cases in a Tertiary Health Centre in Nigeria. Case Rep Clin Med. 2018;7(4):259-68. [Google Scholar]
- Vedavathi V, Senigala K, Bandi S, Rohini N. Analysis of Cervical Cytology Using PAP Smear in Women Residing in Bangalore Rural, India. J Evid Based Med Healthc. 2019;6(51):3156-9. [Google Scholar]
- Gupta K, Malik N, Sharma V, Verma N, Gupta A. Prevalence of cervical dysplasia in western Uttar Pradesh. J Cytol. 2013;30(4):257-62. [Google Scholar]
- Rawat K, Rawat N, Mathur N, Mathur M, Chauhan N, Tinna R. A study of cytological pattern of cervical papanicolaou smears in western Rajasthan, India. Int J Reprod Contracept Obstet Gynecol. 2016;5(9):3186-90. [Google Scholar]
- Mulay K, Swain M, Patra S, Gowrishankar S. A comparative study of cervical smears in an urban Hospital in India and a population-based screening program in Mauritius. Indian J Pathol Microbiol. 2009;52(1):34-7. [Google Scholar]
- Rana S, Jairajpuri Z, Jetley S. Cervical smear cytology on routine screening in a semi urban population in New Delhi A review of 610 cases. Arch Med health Sci. 2013;1(2):131-5. [Google Scholar]
- Tailor H, Patel R, Patel P, Bhagat V. Study of cervical pap smears in a tertiary care hospital of South Gujarat, India. Int J Res Med Sci. 2016;4(1):286-8. [Google Scholar]
- Pun RG, Shrestha J, Awale PJ, Chitrakar N, Jha R, Khadka SS. Cytological pattern of cervical pap smears. J Pathol Nepal. 2018;8(1):1280-4. [Google Scholar]
- Rana R, Singh M, Jha K, Poudyal P, Kafle S. Study of cervical cytology in papanicolaou smears in a newly established tertiary care centre in eastern region of Nepal. Int J Health Sci Res. 2018;8(1):20-4. [Google Scholar]
- Ajmera D, Kucheria D, Kathed D, Farooque D, Sharma D, Chourasia D. Analysis of cervical pap smears as per bethesda system in a tertiary care centre. IJMBS. 2019;3(6):96-100. [Google Scholar]
- Kusumam V, Beevi N, Sreenivas S, Nurul A, Menon V. Comparative study of Pap smear abnormalities in HIV infected and HIV non-infected women. Int J Reprod Contracept Obstet Gynecol. 2016;5(3):783-7. [Google Scholar]
- Atla B, Uma P, Shamili M, Kumar S. Cytological patterns of cervical pap smears with histopathological correlation. Int J Res Med Sci. 2015;3(8):1911-6. [Google Scholar]
- Joshi C, Kujur P, Thakur N. Correlation of Pap Smear and Colposcopy in Relation to Histopathological Findings in Detection of Premalignant Lesions of Cervix in A Tertiary Care Centre. Int J Sci Stud. 2015;3(8):55-60. [Google Scholar]
- Bindroo S, Garg M, G. Correlation of Cervical Pap Smear with Histopathological Diagnosis in Cervical Lesions: A 2 Years Retrospective Study. Int J Contemp Med Res. 2019;6(7):17-20. [Google Scholar]
Article Metrics
- Visibility 8 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.207-213
-
CrossMark
- Citation
- Received Date March 20, 2024
- Accepted Date January 07, 2025
- Publication Date March 13, 2025