Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

A case control study to assess clinical and lipid profile in patients with xanthelasma palpebrarum in a tertiary care centre
Abstract
Background: Xanthelasma palpebrarum is used to describe xanthoma that occurs on the eyelids or inner canthi of the eyes. It is frequently associated with cardiovascular disease, diabetes, obesity etc. Various authors have found a positive relationship between xanthelasma palpebrarum and lipid profile.
Aim and Objective: Xanthelasma palpebrarum is a common condition observed in dermatology OPD for the cosmetic problem posed by it. Most of these patients would not have undergone a lipid profile and there is a need to know whether lipid profile is mandatory for all the patients presenting with xanthelasma palpebrarum. Hence this study was undertaken
Materials and Methods: In this case-control study, 55 subjects diagnosed with xanthelasma palpebrarum and 55 healthy controls were chosen. All cases and controls underwent detailed clinical examination and fasting lipid profile study.
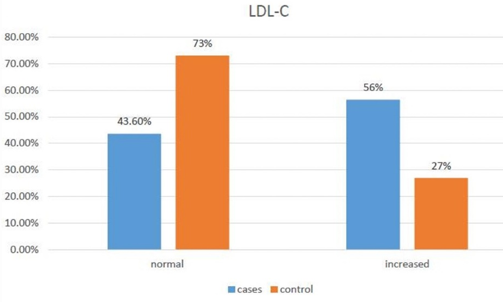
Results: Total cholesterol levels were found increased in 36 cases (65.5%) in contrast to 20 controls (36%) with p=0.004(highly significant).Increase in LDL cholesterol levels were found in 31 cases (56.4%) as against 15 controls (27%) making it statistically significant( p= 0.001). Other cholesterol fractions were not found to have a significant relationship.
Conclusion: At the end of this study it was observed that there is a significant elevation in total cholesterol and LDL cholesterol in xanthelasma patients as compared to controls, thereby making lipid profile study mandatory for all patients.
Introduction
Xanthelasma palpebrarum is used to describe the xanthoma that occurs on either eyelids or the inner canthi. It is the commonest type of cutaneous xanthoma occurring usually bilaterally. It may become permanent. It tends to be progressive and symmetrical. It is found to frequently point to underlying cardiovascular disease, diabetes, obesity etc.[1]
Xanthelasma usually appears during middle age. Its prevalence is higher in women than in men and tends to increase with age. [1] They are usually plaque like yellow lesions that are often found near the inner canthus of eyelids. [2]
‘Xanthelasma’ has been derived from the greek words xanthos (yellow) and elasma (beaten metal plate). [2] Erasmus Wilson coined the term ‘Xanthelasma’ about a century ago. Rayer, A French dermatologist, in 1835, first documented a picture of the same under the cutaneous xanthomas in his atlas on skin disorders.
Although the exact cause is unknown, the etiopathogenesis has been attributed to several factors like lipid abnormalities, hormones, local factors and macrophages. [3] A recent update even points to the role of acetylated LDL and macrophages with the scavenger receptors in their causation.[3] The movement of lipids from within the blood vessel to the surrounding tissues have found to be aggravated by various factors such as raised temperature, physical movement or even friction. No explanation has been advanced for the localization of the lesion to the eyelids.[4]
Xanthelasma palpebrarum can hence be described as a type of planar xanthoma that occurs on the eyelid, which could be either soft, semisolid or calcerous.[5], [6]
Materials and Methods
Between September 2017 and October 2020, 55 patients diagnosed with xanthelasma palpebrarum who visited the outpatient department and in-patients admitted with xanthelasma palpebrarum In a tertiary care hospital were included in this study. Correspondingly, 55 age and sex-matched controls without xanthelasma palpebrarum who fulfilled inclusion and exclusion criteria were also chosen for the study after obtaining informed consent.
A detailed history was taken from the patient with respect to the lesion, to age of onset, duration, the progression of lesion etc. Details regarding associated illnesses like Diabetes mellitus, hypertension, dyslipidemia and biliary diseases, history of treatment for respective disorders and compliance to therapy were taken. Past history and relevant family history for the occurrence of similar lesions was documented.
Blood pressure, pulse rate, height, weight, and BMI of all cases were recorded. All cases were also examined for the presence of pallor, icterus, cyanosis, clubbing, lymphadenopathy, andedema. Systemic examination was done in all cases and controls.
All cases underwent a very detailed cutaneous examination with respect to the site of the lesion (Circumferential/ Upper eyelid/ Medial canthus/ Lower eyelid), size of the lesion, shape, morphology (Macule/ Papule / Plaque), symmetry and multiplicity of the lesions.
For both cases and controls,about 5 ml of fasting (8-12 hours) venous blood was obtained with aseptic precautions . After centrifugation serum was used for estimation of parameter required for the study i.e total cholesterol, LDL cholesterol, HDL, VLDL and triglycerides. Total cholesterol, LDL cholesterol, HDL cholesterol, VLDL, Triglycerides. Lipid profile was analyzed according to NCP-ATP3 guidelines.
Inclusion criteria
All XP patients of any age and sex attending dermatology OPD and willing to give informed consent to participate in the study.
Controls of similar age and sex group without xanthelasma palpebrarum, willing to participate in the study.
Exclusion criteria
Patients who are on lipid-lowering drugs.
Patients with familial dyslipidemias.
Collected data was analyzed by ‘t’ test & chi-square test using SPSS software 26.
Results
The study showed a female preponderance with 43 females (78.2%) and 12 males (21.8%) among the cases ([Table 1]). Mean age of the cases was found to be 45.12±11.23 years and of controls found to be 45.3±10 with a p-value of 0.824 making the two groups comparable.
|
Sex |
Number of patients |
Percentage |
|
Male |
12 |
21.8 |
|
Female |
43 |
78.2 |
Majority of patients belonged to the age group of less than 50 years that is 42 cases (76.4%), followed by more than 50 years that is 13 cases (23.6%).
When diet history was taken it was found that 53 patients were consuming non vegetarian diet and 2 were vegetarians. Duration of the illness was between 1-5 years in most of the cases that is 37 cases (67.2%).
18 cases (32.7%) had a history of hypertension whereas 19 cases (34.5%) had history of diabetes mellitus. Twelve patients had both diabetes mellitus and hypertension. One patient had dyslipidemia. All of the affected individuals were on regular treatment for the above. Examination showed that 44(80%) had bilateral lesions ([Figure 1]) and 11 cases (20%) had unilateral lesions. ([Figure 2])


Symmetry of the lesions were seen in 37 cases (67.3%) and 18 cases (32.7%) showed no symmetry. Out of 48 right eye involved cases, 27 cases (56.8%) showed lesions over the upper eyelid, 6 cases (12.5%) showed lesions over the lower eyelid, and 15 cases (30.2%) had lesion over the upper eyelid and lower eyelid ([Figure 3]).

Out of 51 left eye involved cases, 32 cases (62.7%) showed lesions over the upper eyelid, 9 cases (17.6%) over the lower eyelid, and 10 cases (16%) had over both the upper and lower eyelid.
It was found that 15 cases (31.2%) showed papular lesions on the right eye and about 33 cases (68.8%) showed plaque like lesion on the same eye. On the left eye 15 cases (29.4%) showed papular lesions and 36 cases (70.6%) showed plaque like lesion
Total cholesterol levels was found elevated in 36 cases (65.5%) as compared to 20 controls(36%) ([Table 2]) with p=0.004, (highly significant).
|
Total Cholesterol |
Cases |
Controls |
|
Normal |
19(34.5%) |
35(64%) |
|
Increased |
36(65.5%) |
20(36%) |
LDL cholesterol levels was found to be elevated in 31 cases (56.4%) as against 15 controls (27%) making it statistically significant (p=0.001) ([Table 3], [Figure 4])
|
LDL-Cholesterol |
Cases (%) |
Control (%) |
P value |
|
Normal |
24(43.6) |
40(73.0) |
0.001 |
|
Increased |
31(56.4) |
15(27.0) |
|
|
Mean |
140.80±58.3 |
109.47±35.93 |
An increase in HDL cholesterol was seen in 8 cases (14.5%) as compared to 5 controls (9.9%) with a non-significant p value of 0.31. VLDL cholesterol was increased in 16 cases (29%) and 11 controls (20%) with a non-significant p value of 0.02.
Triglycerides were increased in 30 cases (54.5%) and 17 controls (30.9%) with a non-significant p value of 0.16.
Discussion
Our study showed a female preponderance with 43 females (72.2%) and 12 males (21.8%) among the cases. Female to male ratio of 3.58:1 was observed, ([Table 1]) similar to studies done by Jain et al, Gangopadadhya et al., Epstein et al. and Pedace et al. [1], [3], [7], [8] However Chhetri et al. [9] and Dey et al. [10] showed a male preponderance. Marcelo and Janis [11] found to have equal prevalence among gender in their study.
According to Gangopadadhya et al. maximum cases (30%) belonged to the age group of 31- 40 years.[1] Reddy et al. also reported maximum cases in the same age group of 31-40 years and a peak in incidence in the fourth and fifth decades.[12] Chhetri et al. reported to have observed this peak incidence between 40- 50 years (41.84%).[9] This was similar to our study in which the mean age of the cases were 45.12±11.23 years and majority of the cases that is 42 cases (76.4%) were less than 50 years.
As per Gangopadadhya et al. family history of XP was reported in 27.5% of the cases.[1] Similarly, it was 12.1% according to Jain et al.[9] Significant family history of XP was also observed in 10% cases by Vacca et al.[13] Our study however did not reveal any significant family history in any of the patients.
Gangopadadhya et al. also reported significant comorbidities in the form of diabetes in 20% of patients, Hypertension in 32.5%, heart disease in 20% and other types of xanthoma in 2.5% of patients [1] Jain et al. reported that 42.4% of patients had associated systemic diseases inclusive of HTN, CAD, DM and cholelithiasis.[3] Association with xanthelasma palpebrarum was found to be 6% by Ribera et al and 34.2% by Vacca et al.[13], [14]
According to Marcelo et al. [11] some patients had previous history of myocardial infection and pancreatitis. Hossein kavoussi et al. [15] even reported a case of rheumatoid arthritis and acromegaly patient each in association with XP. In our study there were 18(32.7%) cases of hypertension,19 (34.5%) of diabetes mellitus and 1(1.8%) of dyslipidemia.
Epstein et al reported obesity in 51.4% of the cases. [7] In study by Ribera et al, patients with xanthelasma had a greater mean body weight and were found to be more frequently obese. [8] Pedace et al. reported 26.3 % of the cases to be having obesity.[8] 22 percent of the cases in our study 12(21.3%) had high BMI .
Jain et al. reported that 91% of patients had more than one lesion and 72.7% had both the eyelids being involved. It was noticed that two or more eyelids were involved in 87.9% of the cases.[3] Chhetri et al found both eye lesions in 39% cases, with two eyelids being involved in 53.2% cases and only one eyelid involvement in 7.8% cases.[9] Ribera et al noticed that about 11.3 % patients had only one eyelid involvement, 42.6% had two eyelids, 12.2% had three eyelids & 33.9% had four eyelids being involved.[14] Examination in our study showed the following results i.e 44 cases (80%) had bilateral lesions and 11 cases (20%) had unilateral lesions.
Chhetri et al reported that majority of the cases had two eyelids involvement and in a few the lesion extended to form a ring around the eye. In most of the cases, lesions were situated near the medial corner of the eye lids, but in some it was present in the medial and lateral part of the same lid.[9] Bates et al and Tursen et al also observed that xanthelasma were most often found near the inner canthus of the eyelids. [6], [16]
Following are the findings of our study in which both the right and left eye were analyzed separately. On the right eye, 27 cases (56.3%) had these lesions over the upper eyelid, 6 cases (12.5%) had lesions over the lower eyelid, whereas 15 cases (30.2%) had both upper eyelid and lower eyelid involvemet. On the left eye 32 cases (62.7%) showed lesions over the upper eyelid, only 9 cases (17.6%) over the lower eyelid, whereas 10 cases (19.7%) had involvement of both, upper and lower eyelid. Thereby in our study upper eyelid was the most common site of involvement.
Chhetri et al also noticed in his study that the lesions were yellowish in colour, flat topped and also raised slightly from the surface. [9] Bates et al and Tursen et al observed in their study that xanthelasma are usually plaque like yellow lesions. [6], [16] Whereas our study reported that on the right eye 15 cases (31.2%) showed papular lesions and 33 cases (68.8%) showed plaque like lesions. On the left eye 15 cases (29.4%) showed papular lesions and 36 cases (70.6%) showed plaque like lesions.
Biochemical profile in xanthelasma palpebrarum
Increased total cholesterol values have been observed by various authors. [1], [7], [8], [17] However few of these authors included only cases in their assessment. Our study also showed similar results with total cholesterol levels increased in 36 cases (65.5%) as compared to 20 controls (36%) with p=0.004, making it highly significant.([Table 2])
Increase LDL cholesterol levels have been observed by various authors [1], [14], [18], [19], [20] except for study done by Vermeer et al [21] where it was found to be normal. This was in concurrence with our study showing increased LDL cholesterol levels in 31cases (56.4%) as compared to 15 controls (27%) which was more significant in comparison to other studies and was statistically significant with p value of 0.001.
Our study showed an abnormal HDL cholesterol in 8 cases (14.5%) as against 5 controls (9.9%) with a non-significant p value of 0.31. This was similar to the study done by Ozdol et al in which 12% controls and 8% cases showed low HDL cholesterol levels.[5] However, many authors observed a significant decrease in HDL cholesterol levels. [1], [6], [14]
Watanabe et al observed that VLDL levels were significantly higher than the control levels (p=0.001) in cases.[18] Sharma et al and Jain et al also observed a statistically significant increase in VLDL levels in patients as compared to controls (p<0.01,p=0.001).[3], [22] However, in our study VLDL cholesterol were increased in 16 cases (29%) and 11 controls (20%) and showed a non-significant p value of 0.02.
In our study triglycerides were increased in 30 cases (54.5%) and 17 controls (30.9%) with a non-significant p value of 0.1624.These findings were similar to study done by Ribera et al in which 5.21 % cases and 6.66% controls showed hypertriglyceridemia.[14] But many authors observe elevated triglyceride levels in cases, although there were no comparison with controls.[1], [3], [5], [9], [17]
Conclusion
Xanthelasma palpebrarum is found to be much more common in females when compared to males , the most common site of involvement being the upper eyelid.
Mean total cholesterol and LDL cholesterol levels in patients diagnosed with XP are significantly higher as compared to controls, thereby implying a relationship between elevation in values of total cholesterol and LDL cholesterol with xanthelasma palpebrarum. Hence, a lipid profile study is mandatory for all patients of XP.
There is no significant relationship observed between the extent of the lesion and the multiplicity oflesions with the levels of various cholesterol fractions.
Source of Funding
None.
Conflict of Interest
None.
References
- Gangopadadhya D, Dey S, Chanda M, Pal D, Chaudhuri S. Serum lipid profile in xanthelasma. Indian J Dermatol. 1998;43(2):53-7. [Google Scholar]
- Bergman R. The pathogenesis and clinical significance of xanthelasma palpebrarum. J Am Acad Dermatol. 1994;5(2 Pt 1):236-42. [Google Scholar]
- Jain A, Goyal P, Nigam P, Gurbaksh H, Sharma R. Xanthelasma palpebrarum clinical and biochemical profile in tertiary care hospital of Delhi. Indian J Clin Biochem. 2007;22(2):151-3. [Google Scholar]
- Haque M, Ramesh V. Evaluation of three different strengths of trichloroacetic acid in xanthelasma palpebrarum. J Dermatolog Treat. 2006;17(1):48-50. [Google Scholar]
- Ozdol S, Sahin S, Tokgozoglu L. Xanthelasma palpebrarum and its relation to atherosclerotic risk factors and lipoprotein(a). Int J Dermatol. 2008;47(8):785-9. [Google Scholar]
- Bates M, Warren S. Xanthelasma: clinical indicator of decreased levels of high-density lipoprotein cholesterol. South Med J. 1989;82(5):570-4. [Google Scholar]
- Epstein N, Rosenman R, Gofman J. Serum lipoproteins and cholesterol metabolism in xanthelasma. AMA Arch Derm Syphilol. 1952;65(1):70-81. [Google Scholar]
- Pedace F, Winkelmann R. Xanthelasma palpebrarum. JAMA. 1965;193:893-4. [Google Scholar] [Crossref]
- Chhetri M, Chowdhury N, De B. Xanthelasma palpebrarum:An analysis of 141 cases. J Assoc Physicians India. 1967;15(12):405-12. [Google Scholar]
- Dey A, Aggarwal R, Dwivedi S. Cardiovascular Profile of Xanthelasma Palpebrarum. Biomed Res Int. 2013. [Google Scholar] [Crossref]
- Marcelo GH, Xanthelasma JP. . . 2005. [Google Scholar]
- Reddy S, Singh G, Pandey S, Tiwari D. Clinical and Lipid Profile Studies in Xanthelasma Palpebrarum. Indian J Dermatol Venereol Leprol. 1983;49(3):127-31. [Google Scholar]
- Vacca J, Knight W, Broun G. Clinical observations regarding xanthelasma. Ann Intern Med. 1959;51:1019-31. [Google Scholar] [Crossref]
- Ribera M, Pinto X, Argimon JM, Fiol C, Pujol R, Ferrandiz C. Lipid metabolism and apolipoprotein E phenotypes in patients with xanthelasma. Am J Med. 1995;99(5):485-90. [Google Scholar]
- Kavoussi H, Ebrahimi A, Rezaei M, Ramezani M, Najafi B, Kavoussi R. Serum lipid profile and clinical characteristics of patients with xanthelasma palpebrarum. An Bras Dermatol. 2016;91(4):468-71. [Google Scholar]
- Tursen U, Eskandari G, Kaya TI, Tamer L, Ikizoglu G, Atik U. Apolipoprotein E polymorphism and lipoprotein compositions in normolipidaemic xanthelasma patients. J Eur Acad Dermatol Venereol. 2006;20(3):260-3. [Google Scholar]
- Kahn A, Kahn I, Timar V. Lipid anomalies in cases of xanthelasma. Am J Ophthalmol. 1967;63(2):320-5. [Google Scholar]
- Watanabe A, Yoshimura A, Wakasugi T, Tatami R, Ueda K, Ueda R. Serum lipids, lipoprotein lipids and coronary heart disease in patients with xanthelasma palpebrarum. Atherosclerosis. 1981;38(3-4):283-90. [Google Scholar]
- Mannino G, Papale A, Bella FD, Mollo R, Morgia P, Gabrieli C. Use of Erbium:YAG laser in the treatment of palpebral xanthelasmas. Ophthalmic Surg Lasers. 2001;32(2):129-33. [Google Scholar]
- Fusade T. Treatment of xanthelasma palpebrarum by 1064nm Q-switched Nd-YAG laser: a study of 11 cases. Br J Dermatol. 2008;158(1):84-7. [Google Scholar]
- Vermeer BJ, Mateysen A, Gent CV, Sabben RV, Emeis J. The lipid composition and localization of free and esterified cholesterol in different types of xanthoma. J Invest Dermatol. 1982;78(4):305-8. [Google Scholar]
- Sharma S, Dwivedi S, Prabhu K, Kumar N, Baruah M. Preliminary studies on serum lipids, apolipoprotein-B and oxidative stress in xanthelasma. Indian J Clin Biochem. 1999;14(2):245-8. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 4 Views
- DOI 10.18231/pjms.v.15.i.1.220-224
-
CrossMark
- Citation
- Received Date November 20, 2024
- Accepted Date January 22, 2025
- Publication Date March 13, 2025