Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Twin cases of hereditary spherocytosis: A tale of missed diagnoses
Abstract
Hereditary spherocytosis (HS) is one of the most common hereditary haemolytic anaemia (HA) with variable clinical expression of anaemia, splenomegaly and presence of spherical cells called spherocytes due to the presence of mutations in rbcs membrane protein genes e.g. ANK1 (ankyrin), EPB42 (protein 4.2), SPTA1(α-spectrin), SPTB (β-spectrin) and SLC4A1 (Band 3). There is autosomal dominant inheritance in 75% cases and autosomal recessive in 25% cases.
We report a pair of case of mother and male child; their samples for hemogram were simultaneously received in haematology laboratory. .Both the blood samples showed features of HA with the presence of spherocytes which was confirmed by bed side smear preparation. The value of mean corpuscular haemoglobin concentration (MCHC) was non-contributory to the diagnosis of HS. The bed side smear preparation from finger prick is advantageous as it circumvents the changes due to EDTA excess especially in severely anaemic patients; also the blood cell morphology is better preserved. The advantage of this technique is that there is no time lag between the draw of sample and transit to laboratory, hence no degeneration of blood sample. The study includes review of literature for Red cell indices and Peripheral Blood film (PBF) examination for usage in diagnosis of HS and the current diagnostic protocol for HS.
Introduction
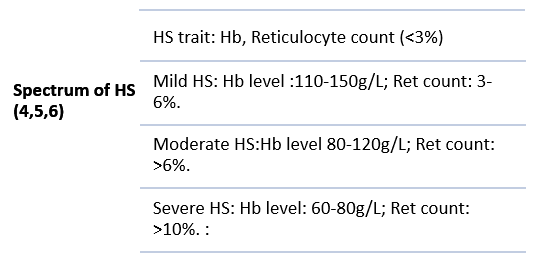
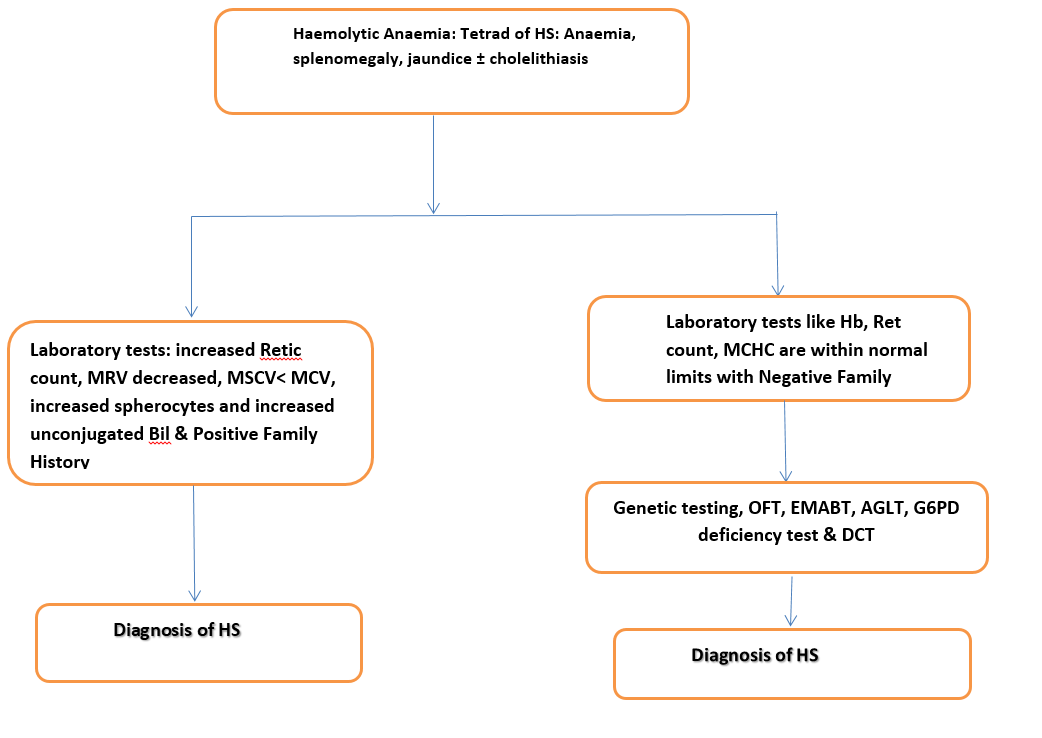
HS is one of the most common hereditary haemolytic anaemia( HHA) with heterogeneous clinical presentation of anaemia, splenomegaly, jaundice, presence of spherocytes, acanthocytes, reticulocytosis and deranged RBC indices like increased Mean Corpuscular Volume (MCV), confirmatory tests like Cryo hemolysis test (CHT), Osmotic fragility Test (OFT), Eosin-5'-maleimide binding test (EMABT) and the molecular tests demonstrating presence of mutations in rbc membrane protein genes e.g. ANK1, EPB42, SPTA1, SPTB and SLC4A1.[1], [2], [3], [4] HS has heterogeneous presentation with the spectrum ranging from HS trait to severe HS as defined in understated [Figure 1] .[5], [6]
Case Presentation
We present twin cases of HS of mother and child. The verbal and written consent was taken in vernacular language and was duly recorded.
Case 1
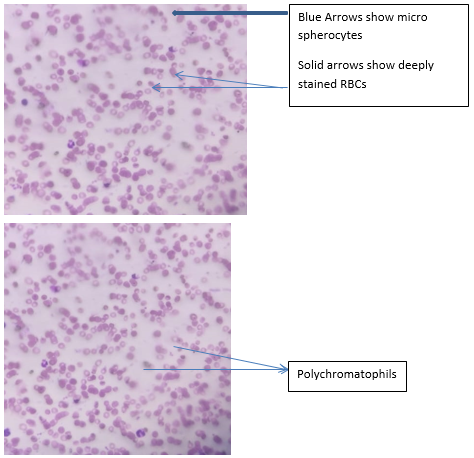
A four year old male child born out of a non-consanguineous marriage reported to the paediatrics casualty department. He had complaints of fever, chills, yellowish discoloration of sclera and urine and poor exercise tolerance .The child had suffered from neonatal jaundice but relevant documents were not available for review. He had history of increasing pallor since 1.5 years of age and received Packed Red Blood Cell (PRBC) transfusion at the same age. The clinician observed the pallor in mother too. On physical examination pallor, yellowish discoloration of sclera and hepatosplenomegaly was observed. The leishman stained PBF examination showed Red Blood Cells (RBCs) showing anisopoikoilocytosis, possibly spherocytes/ high power field(hpf), mild polychromasia, 3 nucleated RBCs/100 WBCs (White Blood Cells) counted- features suggestive of HA. But, the morphology could not be established with confidence. Hence, the bed side smear preparation from finger prick showed approximately 35-38 spherocytes / hpf as shown in [Figure 2]a & b. MCHC was within normal limits (WNL) was not suggestive of HS. All the results of laboratory investigations are described in [Table 1]. The diagnosis of HA was established and the extended work up for HA & HS.
Case 2
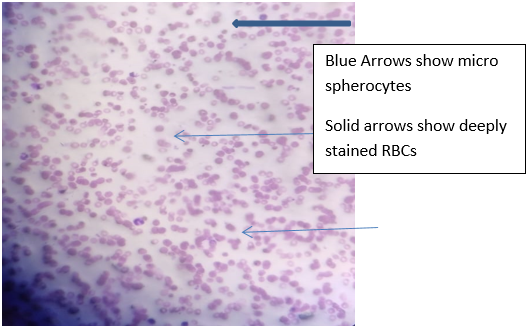
A 23 year old female who was mother of the index case was investigated by the clinician as she appeared pale. There was a past history of jaundice on four previous occasions at the age of 4 years, 8 years, 11 years, and 16 years of age but her old records were not available. There was positive history of passage of orange red urine on few occasions. She gave family history of similar complaint in her paternal uncle. On examination, pallor, yellowish discoloration of sclera and urine and splenomegaly was observed. She delivered a. male child by full term normal vaginal delivery. Her obstetric history was Gravida: 2 Para: 1 Abortion: 1. The leishman stained peripheral PBF showed RBCs showing anisopoikoilocytosis, possibly spherocytes, mild polychromasia, 3 nucleated RBCs/100 WBCs (White Blood Cells) counted- features suggestive of HA. All the results of laboratory investigations are described in [Table 1]. The bed side smear preparation from finger prick showed approximately 15-18 spherocytes as shown in [Figure 3].
|
S.No. |
Investigations |
Result of child |
Result of mother |
|
1. |
Haemoglobin (Hb) |
6.9 gm/dl |
10.1gm/dl |
|
2. |
Peripheral blood smear |
RBCs showed anisopoikoilocytosis, spherocytes (35-38/ hpf), mild polychromasia, 3 nucleated RBCs/100 WBCs (White Blood Cells) counted- features suggestive of HA. WBCs and platelets are WNL |
RBCs (Red Blood Cells showed anisopoikoilocytosis, spherocytes (15-18/hpf), mild polychromasia, 1 nucleated RBCs/100 WBCs (White Blood Cells) counted- features suggestive of HA. WBCs and platelets are WNL. |
|
3. |
Red Cell Indices MCH (pg) :29.4±1.1 MCHC (g/L): 329±5 MCV: 89.5±3.5 |
MCHC: 31.9 gm/dl; MCH: 28.2pg ,MCV: 88.2 fL |
MCHC:32.4 gm/dl; MCH: 31.8 pg ,MCV: 98.2fL |
|
4. |
Reticulocyte count 0.9±0.3 % |
6.56% |
11.42% |
|
5. |
Lactate dehydrogenase(LDH) |
560 units/L |
350 units/L |
|
6. |
Liver function tests |
S. Bilrubin (Bil) total: 6.5 mg/dl, Indirect Bil: 5.5 mg/dl. SGOT:150 I.U/dl SGPT:201 I.U/dl (Unconjugated hyperbilirubinemia) |
S. Bil (Bil) total: 3.0 mg/dl, Indirect Bil: 2.1 mg/dl. SGOT:110 I.U/dl SGPT 170 U/dl ( |
|
7. |
Direct coombs test (DCT) |
Negative |
Negative |
|
8. |
Iron Profile, Folate, Hb High Performance Liquid Chromatography studies(HPLC) |
WNL |
WNL |
|
9. |
Glucose 6 phosphate dehydrogenase (G6PD) |
Negative |
Negative |
|
10. |
RBC distribution width (RDW); |
23.7 % |
19.3 % |
|
11. |
Hb/MCHC |
0.22 |
0.33 |
|
12. |
Hb/RDW |
0.29 |
0.55 |
|
13. |
MCHC/RDW |
1.34 |
1.68 |
|
14. |
CHT |
Positive |
Positive |
|
15.) |
OFT |
Started at 0.70% of NaCl and ended at 0.30% of NaCl (equivocal result). |
Started at 0.60% of NaCl and ended at 0.30% of NaCl (equivocal result). |
Discussion
The child presented with HA, splenomegaly, jaundice with the presence of spherocytes .The smear prepared on bed side provided better RBC morphology, hence rendering the diagnosis easier. The child had significant history of neonatal jaundice and familial inheritance. The suspicion of HS was missed twice during neonatal period and at age of one and half years. The child had severe form of HS that was confirmed by CHT but OFT showed equivocal results. The MCHC was WNL and it did not aid in the diagnosis.
The mother of the child had moderate form of HS with history of jaundice on four occasions that was not meticulously investigated. She had positive history of passage of orange red urine intermittently. There was a missed diagnosis of moderate form of HS till adulthood. She gave a positive family history and a negative history of gall stones. She showed HA, jaundice, splenomegaly and presence of spherocytes. MCHC was WNL and it did not aid in the diagnosis. The diagnosis of HS was confirmed by positive CHT but OFT results were equivocal.
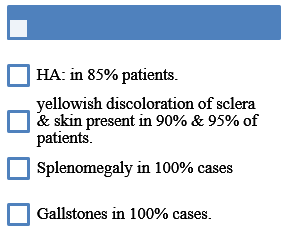
Clinical Presentation
HS has a heterogeneous presentation hence the incidence of mis diagnosis and missed diagnosis is very common. [3], [4]
Tetralogy of HS: [3], [4]
Laboratory investigations
Battery of Tests for the diagnosis of HS:[3], [4]
PBF
RBC indices.
Reticulocyte (Ret) count & indices.
CHT
Acidified Glycerol lysis test (AGLT) 50 on fresh and incubated blood.
SEM
Sodium dodecyl polyacrylamide gel electrophoresis (SDS-PAGE), Western blot to detect erythrocyte membrane skeleton protein deficiency.
Flow cytometric fragility test (FCMOF) & Osmotic fragility test (OFT)
EMABT
Blood film examination
Bolton Maggs et al described spherocytes as RBCs with spherical shape, small size and absence of central pallor. [4] The three types of RBCs can be observed in PBF of HS patients: a.) Darkly stained RBCs, b.) Irregularly shaped RBCs e.g, mushroom shaped cells, helmet / oval shaped cells, acanthocytes .c.) Micro spherocytes. [3] The numbers of spherocytes on PBF ranges from 1%-2% to 60%-70%, generally exceeds 10% (whereas normal value < 5%). [4]
Xue J in his study observed that the proportion of spherical RBCs ranged from14% to 68% and the proportion of concentrated/ deeply stained RBCS ranged from 36% and 89% on PBF examination for diagnosis of HS. [3] Hence deeply stained RBCs are more readily seen on PBF examination rather than spherocytes. [3]
The limitation of PBF examination is that 20% of the HS patients do not present with the presence of classical microspherocytes on PBF. [4] The spherocytes can be observed in other conditions like G6PD deficiency, Auto Immune HA, drug induced HA and other diseases, thus are not specific for HS. [3], [4] The sensitivity of the test depends on pre analytical variables i.e., time of sample placement and the expertise of the observer. [3], [4]
Scanning electron microscope (SEM)
RBC morphology can be observed by SEM, it requires expensive equipment and special methodology. It is used as a screening test for HS. [3]
Relevant RBC indices: [2], [4]
Mean Corpuscular Haemoglobin Concentration (MCHC) estimates the amount of Hb per unit volume, it correlates Hb content with the cellular volume and the values are expressed as g/dl of RBCs, reference value for MCHC: 34 ± 2 g/dl. Wu Y et al reported that when MCHC >355 g/L is used as the cut off for diagnosis of HS, the sensitivity and specificity are 41.07% and 94.47%, respectively, when MCHC ≥334.9 g/L is used as cut off, the sensitivity and specificity are 82.1% and 94.5%, respectively. The increased bilirubin levels leads to false increase in MCHC levels. [4]
Mean sphered cell volume (MSCV)
The RBCs stained with methylene blue are treated with a hypotonic and acidic solution to deproteinize RBCs to yield Spherocytes. The spherocytes can be categorised into mature RBCs and reticulocytes by using technique based on conductivity, volume and light scattering optical detection. MSCV is defined as average volume of both mature RBCs and reticulocytes. [4], [7] Only Beckmann Coulter can report MSCV. [4], [8] Chiron et. al stated that MSCV <MCV can be used as threshold for diagnosis of HS with, the sensitivity and specificity of 100% and 96.7%, respectively. [4]
Mean reticulocyte volume (MRV)
MRV denotes the average volume of all reticulocytes. Few hematology analyzers like Beckman Coulter, Siemens, Mindray and Horiba have the technology to estimate MRV. [4] MRV≤95.77 fL when used as threshold for the diagnosis of HS, the sensitivity and specificity are 86.80% and 91.20%, respectively. [4]
When, Nair et al used MCV-MSCV>10 fL and MRV -MSCV<25 fL are both used as the thresholdfor diagnosis of HS, the sensitivity and specificity are 84.2% and 94.7% respectively for the diffrential diagnosis of HAs. [4] When Arora et al used MCV -MSCV>10 fL as threshold for the diagnosis of HS, the sensitivity and specificity are 82.8% and 95.9%. respectively. MSCV <MCV and MRV ≤95.77 fL is proposed as an ancillary indicator and has been incorporated in the new HS diagnostic protocol owing to high sensitivity and specificity with the ease of usage in clinical practice. [4]
OFT
It is semi quantitative test that detects the resistance of RBCs to different osmotic gradients of hypotonic saline solutions. OFT was considered gold standard for the diagnosis of HS, but the specificity and sensitivity was low. [3], [4] OFT can be positive in other conditions like hereditary elliptocytosis (HE), Auto Immune Haemolytic Anaemia (AIHA), and other pathologies. [3], [4] In a study by Shim et al, a comparison of specificity and sensitivity of OFT in the diagnosis of HS was done and the results showed sensitivity and specificity of 66% and 81.8% respectively. FCMOF has increased sensitivity and specificity of 91.3% and 95.8% respectively in the diagnosis of HS. [4]
EMABT
This is a flow cytometric test in which fluorescent dye; EMA binds to RBC membrane molecules, e.g band 3, with the sensitivity and specificity of 90-95% and 95-99% respectively. EMABT is positive in HE, South Asian ovalocytosis and hereditary pyropoikoilocytosis.[3], [4]
Causes of Mis/ missed diagnosis of HS:[4], [9]
Due to heterogeneous clinical presentation of HS.
The sensitivity and specificity of the routinely used laboratory tests for the diagnosis is not ideal, e.g. MCHC, OFT, PBF examination etc.
Lack of sufficient knowledge of HS amongst health care professionals.
Diagnostic protocol
The updated diagnostic algorithm currently used for the diagnosis of HS in [Figure 5].
Conclusions
It is imperative to address the issue of mis and missed diagnosis of HS in routine practice. This can be achieved by efficient use of first line investigations like RBC indices, PBF exam and OFT with high index of suspicion. In many instances, episodes of jaundice are not fully worked up to lead to the diagnosis of HA & HS. The sensitisation of health care workers towards HS can help reduce the burden of the disease by incorporating molecular diagnostic modalities for disease diagnosis and for antenatal screening of pregnancies in affected individuals.
Abbreviations
HS: Hereditary spherocytosis; HA: haemolytic anaemia; ANK1: ankyrin; EPB42: protein 4.2; SPTA1: α-spectrin; SPTB: β-spectrin; SLC4A1: Band 3; MCHC: mean corpuscular haemoglobin concentration; MCV: mean Corpuscular Volume; MCH: mean Corpuscular haemoglobin; MSCV: mean sphered cell volume; Hpf: high power field; WNL: within normal limits; Hb: haemoglobin; PBF: peripheral blood film; RBCs: Red blood cells; WBCs: White blood cells; RDW: Red cell distribution width; Bil: Bilrubin; LDH: Lactate dehydrogenase; G6PD: Glucose 6 phosphate dehydrogenase; Fl: femtolitres; AIHA: Auto immune haemolytic anaemia; HE: hereditary elliptocytosis; CHT: Cryohemolysis Test.
Patient Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Source of Funding
None
Conflict of Interest
The authors declare that they have no competing interests
References
- Wang X, Zhang A, Huang M, Chen L, Hu Q, Cheng L. Genetic and Clinical Characteristics of Patients With Hereditary Spherocytosis in Hubei Province of China. Front Genet. 2020;11. [Google Scholar] [Crossref]
- Sarma P, Walker H, Hall W, Hurst J. Red Cell Indices. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990. [Google Scholar]
- Xue J, He Q, Xie X, Su A, Cao S. A clinical and experimental study of adult hereditary spherocytosis in the Chinese population. Kaohsiung J Med Sci. 2020;36(7):552-60. [Google Scholar]
- Wu Y, Liao L, Lin F. The diagnostic protocol for hereditary spherocytosis-2021 update. J Clin Lab Anal. 2021;35(12). [Google Scholar] [Crossref]
- Manciu S, Matei E, Trandafir B. Hereditary Spherocytosis - Diagnosis, Surgical Treatment and Outcomes. A Literature Review. Chirurgia (Bucur). 2017;112(2):110-6. [Google Scholar]
- Bolton-Maggs P, Langer J, Iolascon A, Tittensor P, King M. Guidelines for the diagnosis and management of hereditary spherocytosis-2011 update. Br J Haematol. 2012;156(1):37-49. [Google Scholar]
- Broséus J, Visomblain B, Guy J, Maynadié M, Girodon F. Evaluation of mean sphered corpuscular volume for predicting hereditary spherocytosis. Int J Lab Hematol. 2010;32(5):519-23. [Google Scholar]
- Fermo E, Vercellati C, Bianchi P. Screening tools for hereditary hemolytic anemia: new concepts and strategies. Expert Rev Hematol. 2021;14(3):281-92. [Google Scholar]
- Hassan A, Babadoko A, Isa A, Abunimye P. Hereditary spherocytosis in a 27-year-old woman: case report. Ann Afr Med. 2009;8(1):61-3. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 3 Views
- DOI 10.18231/pjms.v.15.i.1.225-230
-
CrossMark
- Citation
- Received Date January 15, 2024
- Accepted Date August 28, 2024
- Publication Date March 13, 2025