Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Navigating the enigma of bone marrow granulomas: A case series exploration
Abstract
Introduction: Granulomatous diseases of marrow can result from a varied group of disorders ranging from infectious diseases to hematological malignancies. Finding granuloma in bone marrow biopsy is a rare finding. Detection of granulomatous disease is possible on Bone marrow biopsy and sometimes it changes the treatment modality.
Aims and Objectives: To study incidence and etiologies of granulomatous diseases of marrow.
Materials and Methods: This was a retrospective study conducted in Department of Pathology, M.K.C.G. Medical College and Hospital, Berhampur. Bone marrow biopsy performed in the period of 1st January 2021 to 31st December 2022 were reviewed along with medical records of these patients.
Results: We reviewed 185 cases of Bone marrow biopsy confirming presence of granuloma in ten patients. The age of the patients varied from 5 years to 55 years. Out of the 10 cases seven (70%) had history of fever, two (20%) with history of pain in abdomen and loss of appetite and (10%) one with weakness. Eight (80%) out of the ten cases had organomegaly. CBC and peripheral smear evaluation of all the cases were done and the finding was pancytopenia in six (60%) cases followed by bicytopenia in four (40%). Seven out of the 10 cases were diagnosed as case of Tuberculosis, one as Hogdkin’s Lymphoma one as Sarcoidosis in Bone marrow trephine biopsy. Despite of thorough investigations no definite etiology was detected in one case.
Conclusion: Bone marrow trephine biopsy is very helpful in finding out Granuloma which is though a non-specific finding may narrow down the diagnosis to various possible differentials.
Introduction
Examination of Bone marrow is considered a significant diagnostic modality for various hematological and non-hematological disorders. This may help in confirmation of a clinical diagnosis and may provide diagnosis of a clinically unsuspected disease thereby changing the treatment protocol.[1] Incidence of bone marrow granuloma ranges 0.3-3% as reported in various literatures. [2] Thus Granulomatous disorders are infrequently detected in bone marrow and they are very nonspecific. However ,presence of granuloma in bone marrow denotes certain diseases like Mycobacterium Tuberculosis, Fungal infections, Sarcoidosis, Mycoplasma, Hodgkin’s lymphoma, Non Hogdkin’s lymphoma and occasionally drug reactions. [3] Granulomatous lesions are detected in bone marrow trephine biopsy, clot preparations and occasionally even in bone marrow aspiration samples. [4]
Most of the studies on granulomatous lesions in bone marrow are conducted in foreign countries but there is paucity of data regarding granulomatous lesions in bone marrow in India. The present study aims at determining incidence and etiologies of granulomatous lesions in bone marrow.
Case Series
This was a retrospective study conducted in Department of Pathology, M.K.C.G. Medical College and hospital, Berhampur in the period of 1st January 2021 to 31st December 2022. All cases that showed granulomatous lesions in bone marrow biopsy were included in the study. Records of all the cases were obtained from Medical Record Department and reviewed. The Bone marrow trephine biopsy and aspiration along with the peripheral blood smears were reviewed by two pathologists to confirm the presence of granuloma.
Bone marrow biopsies were performed under all available aspectic conditions by insertion of Jamshidi needle. Undecalcified bone marrow biopsy samples were put into AZF solution (containing Glacial acetic acid, Zinc chloride, concentrated formaldehyde and distilled water) and allowed to fix overnight. Next day the solution was decanted and the biopsy specimens were washed in distilled water for 30mins and then kept in decalcifying solution (containing 5% formaldehyde and 10% formic acid) for 6 hours. The biopsy specimens were then sent to Histopathology section for further processing. The samples were processed in Automated tissue processor manufactured by Leica and embedded in paraffin wax and cut in thickness of 2µm using a rotary microtome. The sections were stained with Hematoxyline and Eosin (H&E). Fibrosis was assessed using Reticulin stain and Masson’s Trichrome stain. Immunohistochemical stains were performed as per requirement.
Epitheloid granuloma was defined as focal collection of macrophages and epitheloid cells with or without multinucleated giant cells, with or without accompanying cells such as lymphocytes.
Information regarding other serological tests and various radiological investigations were obtained from the medical records.
We reviewed 185 cases of Bone marrow biopsy confirming presence of granuloma in bone marrow biopsy of 10 patients representing incidence of granuloma in bone marrow biopsy of 2.89% and annual incidence of 5 cases per year. Age group of the patients varied from 5 years to 55 years. Out of the 10 patients 3 (30%) were females and 7 (70%) were males.
Most common clinical presentation was fever in 7 cases (70%) followed by pain in abdomen and loss of appetite 2 cases (20%) and weakness in 1 case (10%). Hepatosplenomegaly was present in 8 patients (80%).
Most common hematological alteration was found to be Normocytic normochromic anemia (70%) followed by Macrocytic anemia (20%) and Microcytic hypochromic anemia (10%). Reticulocyte count was low in all cases. Leukopenia was found in 60% of cases and thrombocytopenia in 70%. Pancytopenia was found in 6 (60%) cases and Bi-cytopenia in 4 (40%) cases.
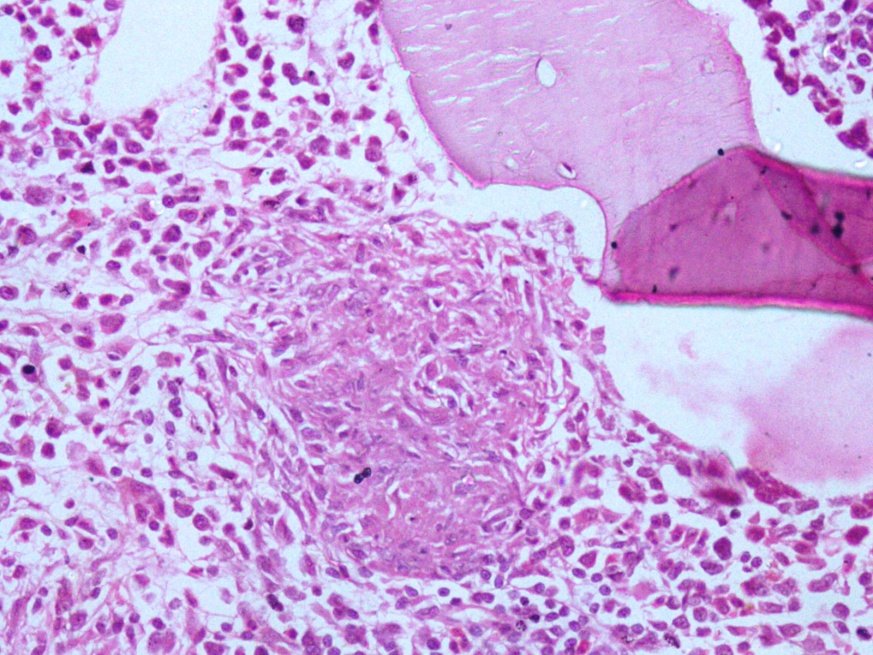
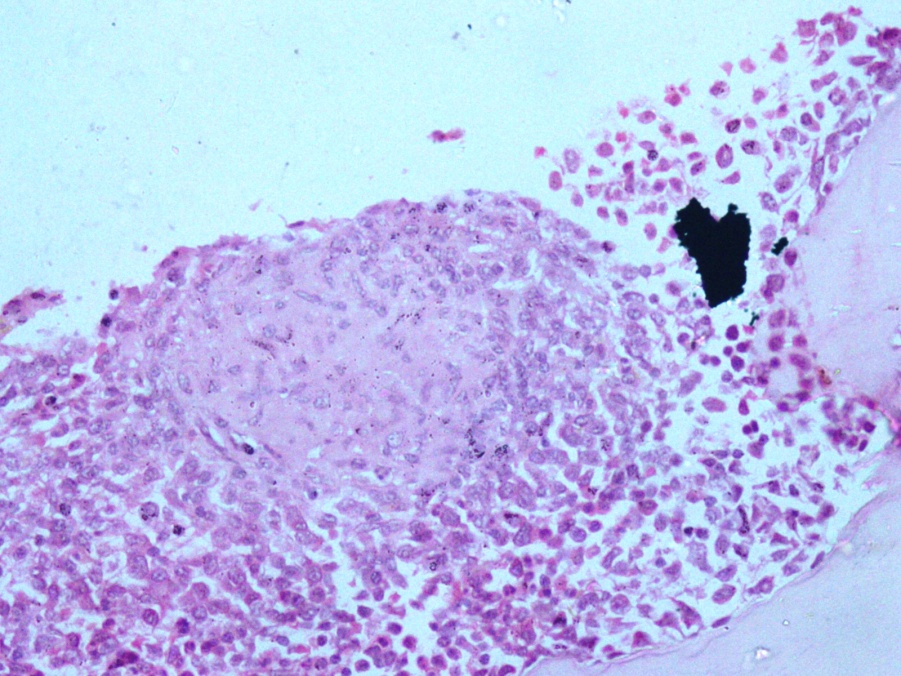
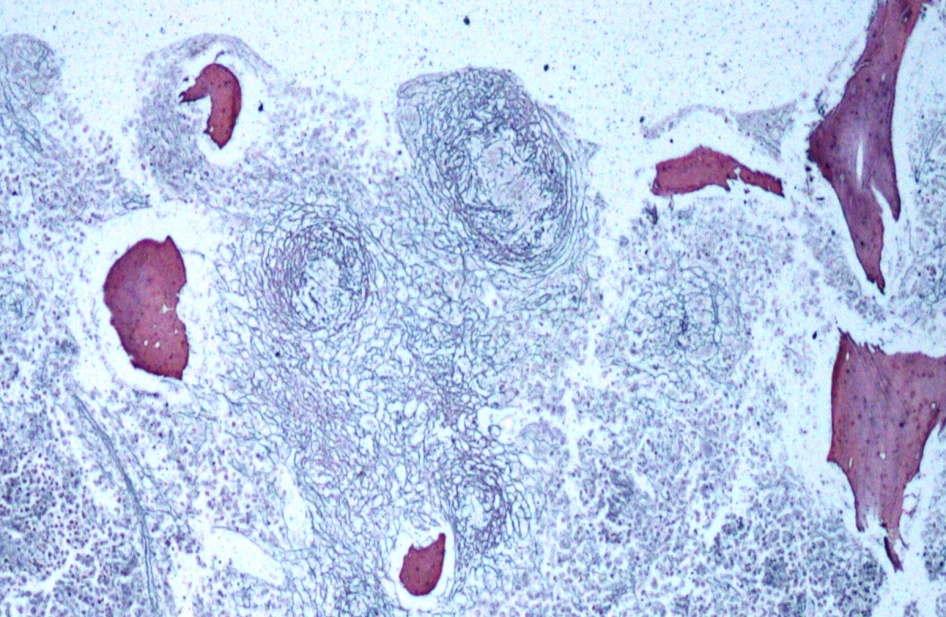
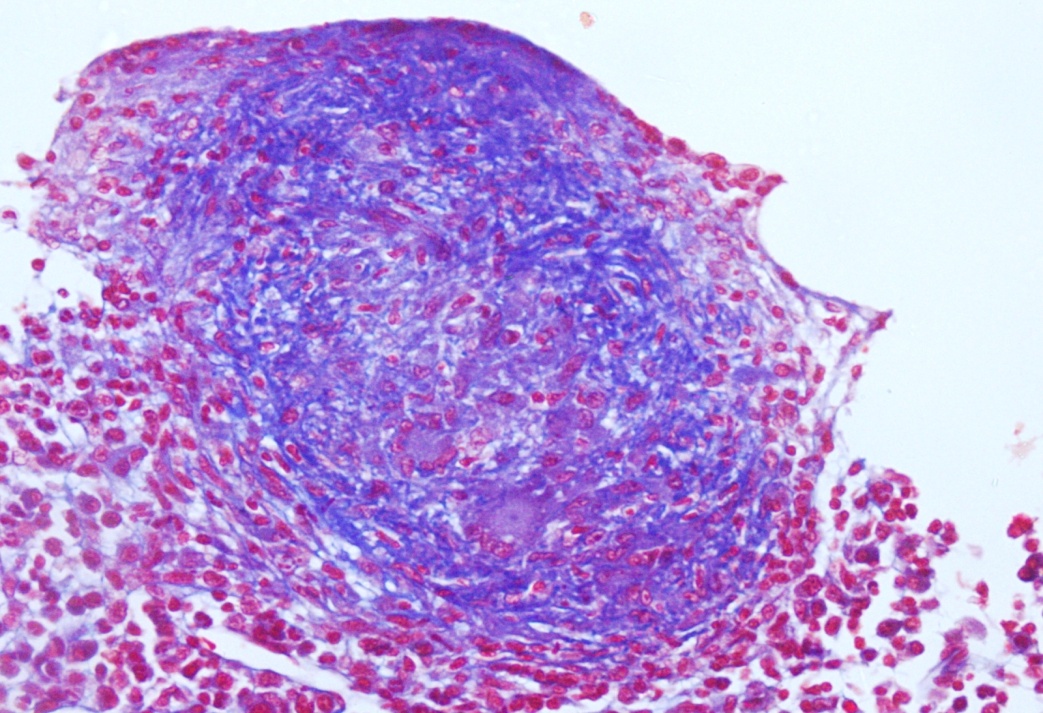
Out of the ten cases seven had well defined epitheloid granuloma with casseous necrosis in H&E stain. ([Figure 1], [Figure 2]) Reticulin and Masson trichrome stain demonstrated bone marrow fibrosis. ([Figure 3], [Figure 4] ) One of these seven cases showed AFB positive bacilli in biopsy. Three of the seven cases were detected as tuberculosis in culture of bone marrow aspirate. Rest three cases were culture negative but empirically treated with ATT and patients responded to treatment and clinico-hematological improvement was noticed. These patients were followed up for a period of 1 year and they were doing well. Thus provisional diagnosis of Tuberculosis was established in these 7 cases.
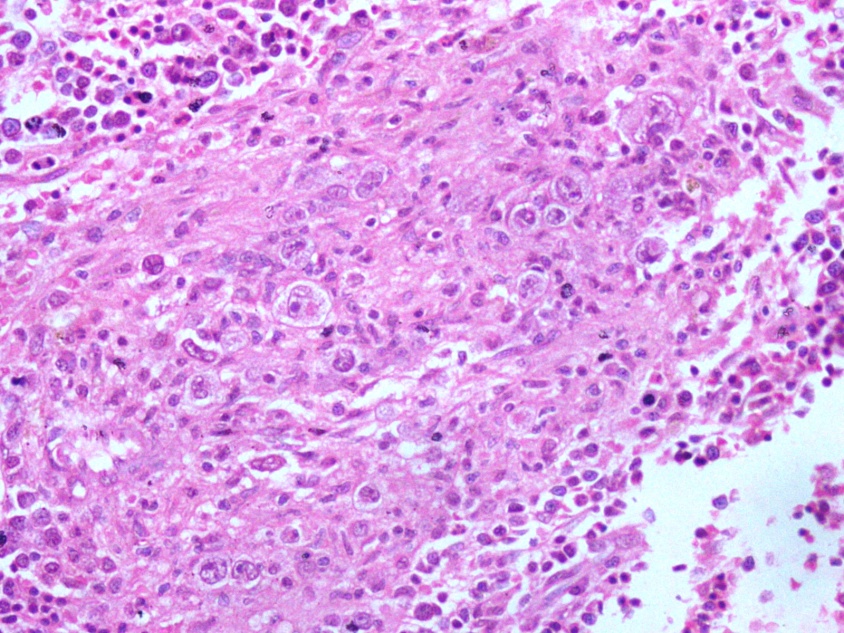
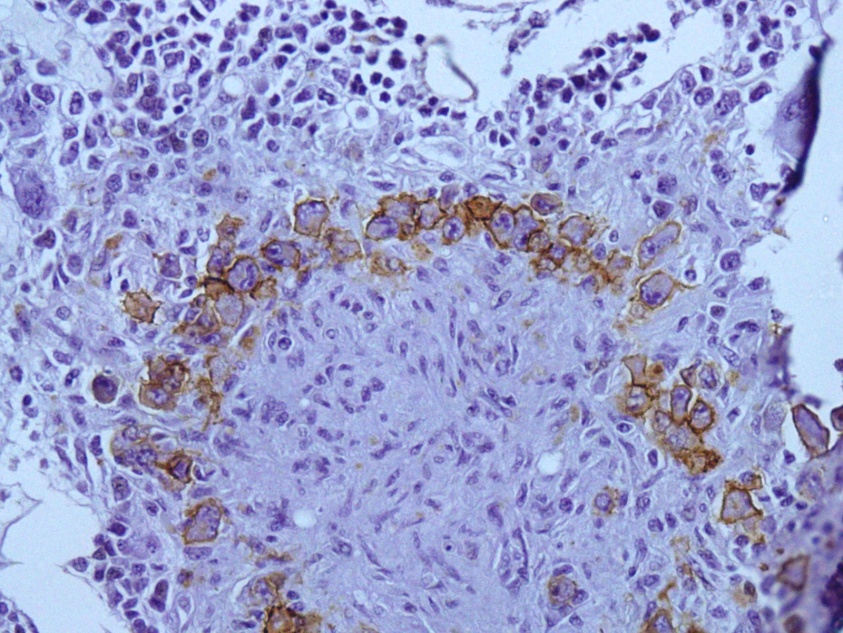
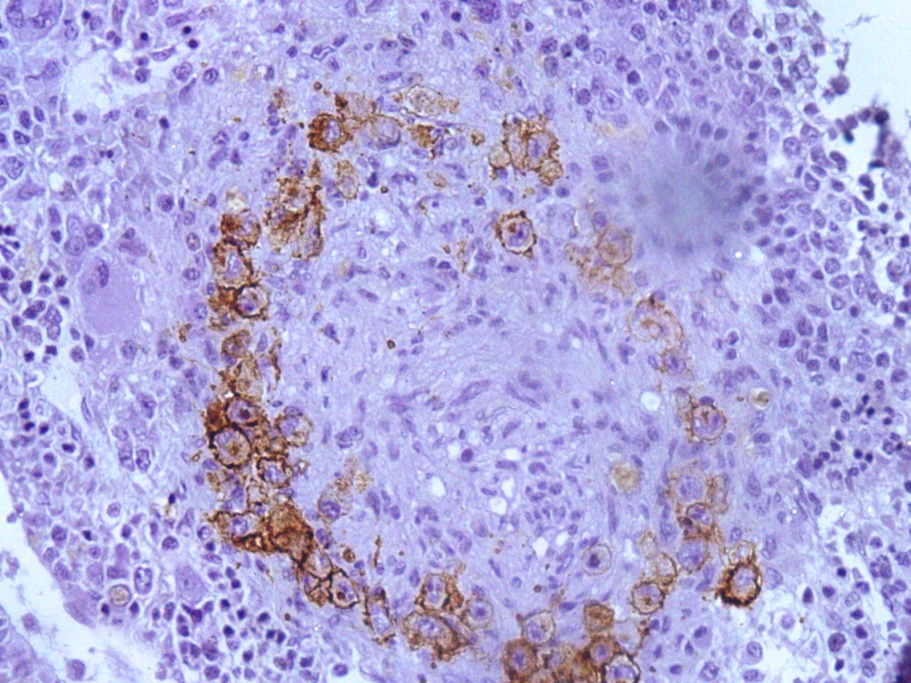
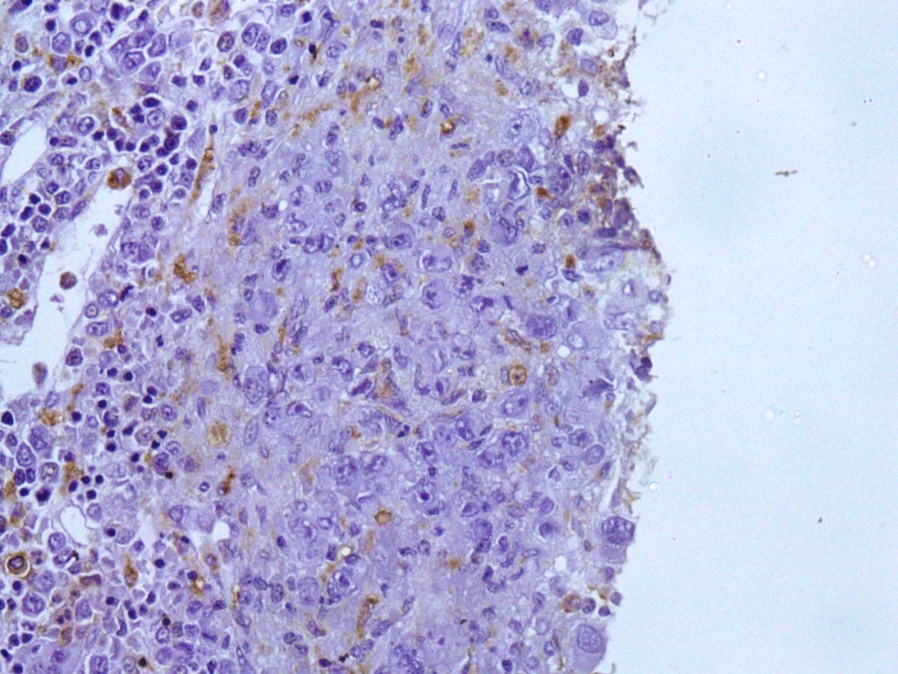
One of the cases having fever and splenomegaly but no lymphadenopathy showed presence of epitheloid granuloma with presence of Reed Sternberg cells admixed with small lymphocytes and macrophages in H&E stain.([Figure 5]) IHC stains further highlighted the Reed Sternberg cells (CD 15, CD30 positive) ([Figure 6], [Figure 7] ) surrounded by CD3 positive T cells. The epitheloid cells and histiocytes were positive for CD 68. ([Figure 8]) CT scan of abdomen and pelvis and CT thorax showed no mesenteric or mediastinal lymphadenopathy. Splenic biopsy was performed but found to be negative for lymphoma. Thus it as confirmed to be a case of primary mixed cellularity Hogdkin’s lymphoma of bone marrow.
One of the cases showed presence of epitheloid granuloma without necrosis. Bone marrow culture was negative for mycobacterium tuberculosis. Chest X-Ray showed diffuse nodular infiltration. Serum calcium and ACE level was elevated. Patient had mediastinal lymphadenopathy. CT guided biopsy of mediastinal lymph node was suggestive of sarcoidosis. Patient was diagnosed and treated in line of Sarcoidosis.
In another case no definitive etiology could be established despite of through investigations.
Discussion
Granulomatous diseases can involve multiple systems including lungs, lymph nodes, liver and spleen [1] However granuloma in bone marrow is an infrequent but nonspecific finding that can denote many systemic diseases. Granuloma formation is a non-specific response by reticuloendothelial system to a persistent antigenic stimulus. [5], [6] Majority of cases of bone marrow granuloma are attributed to infectious sources.
Incidence of bone marrow granuloma in our study was 2.89% which coincides with the reported incidence.[2] Most of the cases in the present study presented with non-specific symptoms like fever, pain in abdomen, weakness, loss of appetite. Other studies also found similar presenting features in patients diagnosed with granulomatous lesion in bone marrow. [3], [7] After thorough history and laboratory investigations a specific diagnosis can be made in most cases. In this study we could establish a specific etiology in 9 out of 10 cases. Similar findings were detected by other studies.[3], [8] Most of the granulomatous lesions in the present case were due to tuberculosis. Other studies have also found infectious diseases like tuberculosis as the most common cause of granulomatous lesions in bone marrow. [3], [9]
One of the cases was reported as primary Hogdkin’s lymphoma of bone marrow. Atypical presentation of Hogdkin’s lymphoma with bone marrow granuloma formation has been reported.[10] These granulomas may present before the onset of primary malignancy and may delay the diagnosis.[11] In lymphomas bone marrow granuloma could be due to invasion of the bone marrow or due to non-specific immunologic change due to malignancy. [12]
Conclusion
Although nonspecific finding, granuloma in bone marrow is helpful to narrow down the differential diagnosis to a group of related disease. Etiology of bone marrow granuloma varies according to the geographic region with tuberculosis still remaining the most common cause despite of various control programmes for tuberculosis. But atypical presentation of Hodgkin lymphoma in bone marrow may get missed if all cases of granulomas of bone marrow are not properly investigated.
Source of Funding
None.
Conflict of Interest
None.
References
- Salkar A, Pankanti S, Pankanti R, Pedakontala V. Granulomatous Lesions in Bone Marrow: A Case Series. IOSR J Dent Med Sci. 2016;15(10):96-100. [Google Scholar]
- Kvasnicka H, Thiele J. Differentiation of granulomatous lesions in the bone marrow. Pathologe. 2002;23(6):465-71. [Google Scholar]
- Farooq S, Bashir N, Angmo D. Granulomatous lesions in the bone marrow-An experience from a tertiary care centre. Int J Med Sci Curr Res. 2018;1(1):62-5. [Google Scholar]
- Vilalta-Castel E, Valdés-Sanchez M, Guerra-Vales J, Teno-Esteban C, Garzón A, López J. Significance of granulomas in bone marrow: a study of 40 cases. Eur J Haematol. 1988;41(1):12-6. [Google Scholar]
- Bodem C, Hamrony B, Tylor H, Kleopfer L. Granulomatous bone marrow disease . A review of theliterature and clinicopathological analysis of 58 cases. Medicine (Baltimore). 1983;62(6):372-83. [Google Scholar]
- AR. Stromal reactions . Histopathology of the bone marrow. 1976. [Google Scholar]
- Feng J, Zhang H, Zhong DR. A clinical analysis of 20 cases with bone marrow granulomas. Zhonghua Nei Ke Za Zhi. 2009;48(6):485-7. [Google Scholar]
- Mirzai A, Hosseini N, Sadeghipour A. Indications and diagnostic utility of bone marrow examination in different bone marrow disorders in Iran. Lab Hematol. 2009;15(4):38-44. [Google Scholar]
- Gandolfo E, Bruno G, Vitali E, Ferrero S, Pagano G. Tuberculosis as a cause of fever of unknown origin in the elderly: a case report. Ann Ital Med Int. 2002;17(2):117-20. [Google Scholar]
- Koo S, Park C. Granulomatous bone marrow involvement of Hodgkin lymphoma, nodular sclerosis type. Blood Res. 2017;52(2). [Google Scholar] [Crossref]
- Daly PA, Briain DS, Robinson I, Guckian M, Prichard JS. Hodgkin's disease with a granulomatous pulmonary presentation mimicking sarcoidosis. Thorax. 1988;43(5):407-416. [Google Scholar]
- Sneha L, Thayammal I, Priyathersini N, Vilvanathan V. Epitheloid granuloma of bone marrow- not always tuberculosis, think beyond what you see. Int J Contemp Pediatr. 2021;8(7):1278-80. [Google Scholar]
Article Metrics
- Visibility 7 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.243-247
-
CrossMark
- Citation
- Received Date September 19, 2024
- Accepted Date December 02, 2024
- Publication Date March 13, 2025