Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Spontaneous Pneumothorax/Pneumomediastinum in COVID-19 independent of CT severity index: A case series from Indian subcontinent
Abstract
Spontaneous air leaks consisting of pneumomediastinum and pneumothoraces are rarely reported in non severe COVID-19 disease in India. We hereby report three cases, out of which spontaneous pneumomediastinum developed in severe COVID-19 pneumonia. Two cases of Pneumothoraces developed in patients of nonsevere pneumonia. Moreover Pleuritic Chest Pain secondary to pneumothorax was the presenting complaint in a young patient suffering from mild pneumonia radiologically. In view of recent upsurge of COVID-19 cases, we emphasize adequate monitoring for early detection of spontaneous air leaks independent of severity of lung involvement.
Introduction
Coronavirus diseases officially named as COVID-19 by WHO is the disease caused by Severe Acute Respiratory Syndrome coronavirus 2 (SARS-Cov-2).[1] It is causing repeated outbreaks with emergence of new variants at regular intervals.
Clinical spectrum of disease related to SARS-COV-2 varies from asymptomatic infections to severe disease in form of Acute Respiratory Distress Syndrome. [2], [3]
Radiological assessment in form of Chest radiograph and CT scan imaging plays an important role in prognostication as well as management of patients.
Common computerized tomography (CT) findings in COVID-19 are of patchy ground-glass opacities (GGO’s) with a peripheral or posterior distribution, mainly involving the lower lobes.[4] The 25-point CT severity score categorises lung involvement into mild, moderate and severe variety. [4]
There is scarce data reporting the COVID-19 associated spontaneous air leaks into the pleural space or the mediastinum leading to pneumothorax or pneumomediastinum respectively, which is independent of CT scan severity index.
Here we report one case of spontaneous pneumomediastinum and two cases of spontaneous Pneumothorax associated with COVID-19 disease in non-intubated patients. Characteristically in our case series, Pneumomediastinum occurred in severe disease while spontaneous pneumothoraces occurred in patients which were categorised as mild and moderate disease as per computerised tomography severity index (CTSI). This highlights the importance of being vigilant regarding the possible complications of COVID-19 , even in patients with non-severe lung involvement radiologically. This study carries utmost importance specially when COVID -19 cases on rapid upsurge amid detection of new variant of interest JN.1.
Case Presentation
Case 1
A 57 years old male, non-smoker, with no previous comorbidities, vaccinated against SARS COV2 was admitted with complaints of fever, dry cough and progressive breathlessness for duration of 3 days. On examination, he was tachypnoeic with use of accessory muscles of respiration. His respiratory rate was 34/min, fever of 101ºF, pulse rate of 115 /min, oxygen saturation of 82% on room air and blood pressure of 122/86 mmHg. Chest auscultation revealed bilateral crackles.
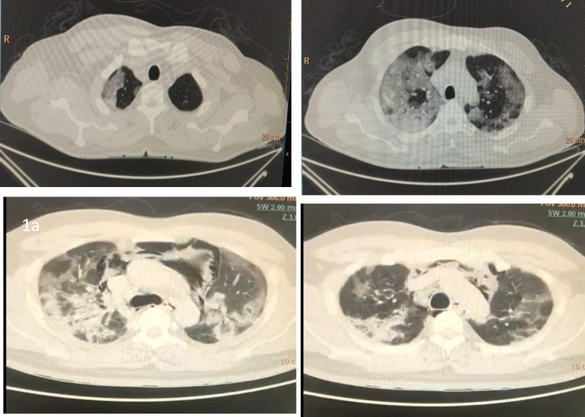
Nasopharyngeal swab taken for SARS COV2 was tested positive by RT PCR. Laboratory work up showed white blood cell count of 4400 /µL, lymphocyte count of 1250/ µL and CRP level was 32ng/ml. CT scan detected severity score of 23/25 ([Figure 1]a,b). He was classified as COVID-19 severe disease. He was managed with oxygen supplementation @ 5 litres /min, COVID awake repositioning protocol (CARP), intravenous Methylprednisolone, Inj. remdesivir and Inj. LMWH as per recommended guidelines.[5] At day 6 of admission he developed pronounced cough followed by respiratory distress with increasing oxygen requirements.
Inflammatory markers work up showed CRP of 110 mg/L, Lactate Dehydrogenase (LDH) of 636 U/L and a ferritin of 521 ng/mL. D-dimer was 760 ng/ml. Colour Flow Doppler study both lower limbs as well as bed side 2 D echocardiography was normal. CT scan showed pneumomediastinum. [[Figure 1]c,d}
HIV was negative. Serum procalcitonin, galactomannan, beta D glucan levels were normal. In view of Cytokine storm syndrome, he was administered single dose of Inj. Tocilizumab 400 mg intravenously. Post tocilizumab therapy, there was decrease in oxygen requirements, tachypnoea improved. CRP levels lowered down to 20 mg/l. He showed gradual improvement & was weaned off the oxygen over the period of next 3 months.
Case 2
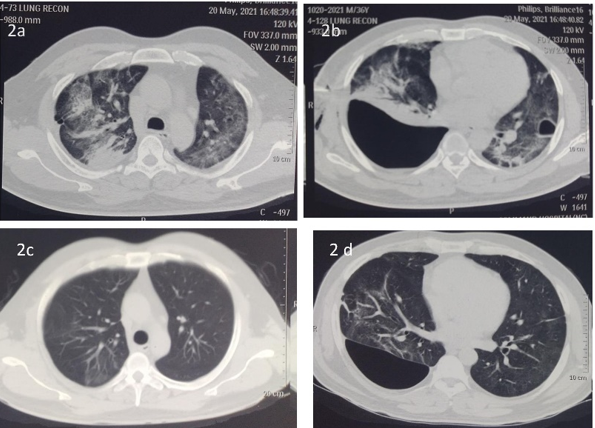
A 38 years old male non-smoker, vaccinated against SARS COV2 presented with complaints of high grade fever, cough, headache, breathlessness on exertion of the duration of 3 days. RT PCR for SARS COV 2 was positive. Clinically he was tachypnoeic (respiratory rate 24/min) and oxygen saturation was 92 % on room air. On Chest auscultation there were crackles bilateral lung fields. Portable Chest radiograph showed bilateral lung infiltrates with predominance in right upper and right middle zone. Blood work up showed WBC count of 12000/mm3 with polymorphs of 84%, Neutrophil to Lymphocyte (NLR) Ratio > 4, CRP level was 19 ng/ml. He was classified as moderate disease and managed with oxygen supplementation @ 5 litres /min, awake proning, intravenous antibiotics, intravenous Methylprednisolone, Inj. remdesivir, and Inj. LMWH as per national guidelines.[5] After showing initial clinical improvement, patient developed sudden onset right sided chest pain followed by breathlessness at rest at Day 7 of admission. On auscultation breath sounds were absent on right side of chest. CT scan showed pneumatocele left lower lobe, diffuse patchy areas of GGO’s Bilateral lung fields and hydropneumothorax right ([Figure 2]Fig 2ab). CT severity index was 14/25. Intercostal chest drain was placed in right pleural cavity. Patient improved clinically with decreasing oxygen requirement. Repeat CT scan ([Figure 2]c,d) imaging showed resolution of GGO with persistence of right sided loculated hydropneumothorax due to misplacement of ICD. Hydropneumothorax was managed with placement of pigtail catheter under real time ultrasound guidance. Intrapleural fibrinolysis with 10 mg alteplase installed intrapleurally twice daily for 3 days was done to break the loculations and hydropneumothorax was drained completely. Patient improved significantly, pigtail was removed and he was discharged to home.
Case 3
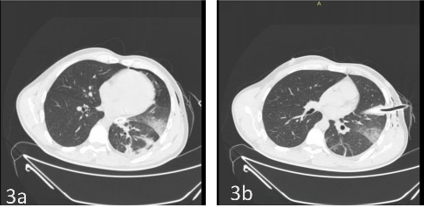
A 35 years old male smoker with smoking exposure of 10 pack years and was fully vaccinated against SARS COV2. He presented to emergency with sudden onset left sided chest pain and breathlessness at rest. Clinically he was tachypnoeic with respiratory rate of 40 /minute, pulse rate of 125 /min, oxygen saturations of 82% on room air, Temp of 99.6 F and blood pressure of 96/66 mmHg. Chest examination showed deviation of trachea to right side, hyper resonant note on percussion and absent breath sounds on auscultation involving left hemithorax. Portable chest radiograph revealed left sided pneumothorax. Immediately intercostal tube drainage was achieved with 32 Fr chest drain. Subsequently nasopharyngeal swab tested positive for SARS COV2 by RT PCR method. Post ICD insertion patient improved significantly and respiratory distress was settled. CT scan showed CT Severity score of 6/25 ([Figure 3]a & b). He was maintaining saturation of 93% on room air, Respiratory rate of 24/minute and blood pressure of 118/70 mmHg. His haematological and biochemical parameters were normal. CRP level was 6 ng/ml. He was treated with systemic steroids and anticoagulation along with oxygen supplementation. ICD was removed after complete resolution of pneumothorax and patient was discharged to home.
Discussion
COVID-19 spectrum ranges from mild to critical illness. Few patients who are mildly symptomatic may progress to severe disease between day 4 and day 10 of illness.[6] Radiological features of COVID -19 Pneumonia as proposed by The Radiological Society of North America (RSNA), involves four categories (i.e, typical appearance, indeterminate appearance, atypical appearance, and negative for pneumonia). Radiologically COVID-19 typically presents with posterior subpleural located rounded GGO with or without consolidation.[7] Pleural involvement in COVID-19 have been rarely reported. Lung cavitation or cysts have been described as atypical features as per RSNA.[7] All our cases had radiological patterns of GGO’s as described by RSNA. In addition to peripheral GGOs, Case 1 developed spontaneous pneumomediastinum and rest of the two cases suffered spontaneous pneumothorax, which are rarely described in literature.
Spontaneous pneumomediastinum occurs due to pressure gradient between the alveoli and pulmonary interstitium leading to alveolar breakdown as described by Macklin. It can be due to an increase in intra-alveolar pressure and overinflation of the alveoli as happens during violent cough. This causes the rupture of fragile alveoli with air leaking to the interstitium which tracks along the venous sheaths to lung hila and then to mediastinum.[8] Our case 1 had extensive lung involvement due to COVID-19 & had bout of cough at Day 7. Sudden increase in intra alveolar pressure due to cough coupled with increased lung frailty caused by COVID-19 lead to development of Spontaneous Pneumomediastinum.[9] Inflammatory process due to COVID-19 causes necrosis as well as wall destruction of neighbouring alveoli and airspaces leading to pneumatocele formation.[10] Our case 2 was detected to be having pneumatocele involving left lower lobe in addition to pneumothorax of right side. In addition to pneumatocele rupture other mechanisms giving rise to pneumothorax may include parenchymal injury, inflammation, ischemia, infarction and sudden increase in intra alveolar pressure due to cough.[11] Both the cases discussed above (case 1 and case 2) suffered from COVID-19 and had deterioration in lung status between 5-8 days of onset of symptoms. This corresponds well to observation that COVID-19 induced extensive lung involvement and prolonged inflammation gives rise to lung frailty,[9] which resulted in the rupture of alveoli in case 1 and 2. Our case 3 in case series had presented with sudden onset breathlessness at the time of onset of disease and was detected to have pneumothorax on initial presentation. He had mild lung involvement and CT severity index was 6. He improved significantly with placement of Intercostal drain. Ayazi et al had documented case series specifying pneumothorax to be presenting manifestation of COVID-19 . [12] Similar to this case series cause-effect relationship of pneumothorax with COVID-19 could not be established in our case also. Our case 1 and case 2 were non smoker with no previous comorbidities. However, case 3 was smoker, enhancing the risk of development of spontaneous pneumothorax. Pneumothorax could have been multifactorial in this case with both smoking and COVID-19 infection playing their role. Pneumomediastinum in case 1 was managed conservatively and Pneumothorax in rest of the cases were drained with intercostal drain. All our cases had shown good recovery and are presently asymptomatic. This is in agreement with the previously published multicentric case series, where authors have warned against therapeutic nihilism in the cases of COVID-19 associated pneumothorax. [13] These cases require intense monitoring and appropriate therapeutic interventions where ever needed. Our cases emphasizes the importance of being vigilant of spontaneous pneumothoraces even if initial presentation of patient as well as CT severity index does not fall into severe category. [14]
Conclusion
In this study we analysis and clearly manifests that monitoring is required in cases of COVID-19 to detect early signs of air leaks irrespective of CT severity of the disease.
Source of Funding
None.
Conflict of interest
None.
References
- . WHO Coronavirus (COVID-19) Dashboard [Internet]. . . [Google Scholar]
- Guan W, Ni Z, Hu Y, Liang W, Ou C, He J. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-20. [Google Scholar] [Crossref]
- Yang X, Yu Y, Xu J, Shu H, JX, Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. [Google Scholar]
- Saeed G, Gaba W, Shah A, Helali AA, ER, AAA. Correlation between Chest CT Severity Scores and the Clinical Parameters of Adult Patients with COVID-19 Pneumonia. Radiol Res Pract. 2021. [Google Scholar] [Crossref]
- . Government of India, Ministry of Health and Family Welfare. Guidelines on management of COVID-19 in adults. . 2021. [Google Scholar]
- Cohen P, Hall L, John J, Rapoport A. The Early Natural History of SARS-CoV-2 Infection: Clinical Observations from an Urban, Ambulatory COVID-19 Clinic. Mayo Clin Proc. 2020;95(6):1124-6. [Google Scholar]
- Simpson S, Kay F, Abbara S, Abbara S, Bhalla S, Chung J. Radiological Society of North America Expert Consensus Statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. J Thorac Imaging. 2020;35(4):219-27. [Google Scholar]
- SK, Houari N, Haloua M, YL, MB, Serraj M. Spontaneous pneumomediastinum occurring in the SARS-COV-2 infection. IDCases. 2020;21. [Google Scholar] [Crossref]
- Lemmers D, Hilal M, Bnà C, Prezioso C, Cavallo E, Nencini N. Pneumomediastinum and subcutaneous emphysema in COVID-19: barotrauma or lung frailty?. ERJ Open Res. 2020;6(4). [Google Scholar] [Crossref]
- Capleton P, Ricketts W, Lau K, Ellis M, Sheaff K, Giaslakiotis. Pneumothorax and Pneumatocoele Formation in a Patient with COVID-19: a Case Report. SN Compr Clin Med. 2021;3(1):269-72. [Google Scholar]
- Hameed M, Jamal W, Yousaf M, Thomas M, Haq I, SA. Pneumothorax in Covid-19 Pneumonia: A case series. Respir Med Case Rep. 2020;31. [Google Scholar] [Crossref]
- Ayazi S, Zebarjadi J, Grubic A, Tahmasbi H, Ayazi K, Jobe B. Pneumothorax as the presenting manifestation of COVID-19. J Thorac Dis. 2020;12(12):7488-93. [Google Scholar]
- Martinelli A, Ingle T, Newman J, Nadeem I, Jackson K, Lane N. COVID-19 and pneumothorax: a multicentre retrospective case series. Eur Respir J. 2020;56(5). [Google Scholar] [Crossref]
- Nunna K, Braun A. Development of a large spontaneous pneumothorax after recovery from mild COVID-19 infection. BMJ Case Rep. 2021;14(1). [Google Scholar] [Crossref]
Article Metrics
- Visibility 9 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.256-259
-
CrossMark
- Citation
- Received Date April 28, 2024
- Accepted Date September 19, 2024
- Publication Date March 13, 2025