Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

A case series of pancytopenia in adults in a tertiary care hospital-clinical spectrum and etiological overview
Abstract
Pancytopenia is a medical condition where there is decrease in cell count from all three lineages from bone marrow resulting in anaemia, leukopenia, and thrombocytopenia. It is usually due to the underlying disease process affecting bone marrow or peripheral blood cells. To study patients suffering from pancytopenia and evaluate clinical presentation, haematological & biochemical features, complications, and outcome of the patients.
The present study was a prospective observational study. In a series of 6 pancytopenia cases, we found a case of each of methotrexate overdose, vitamin B12 deficiency, complicated vivax malaria, fungal infection, myelodysplastic syndrome, hypoplastic anaemia. We observed different spectrum of presentation, clinical course, complications, response to treatment and outcome of all the cases of pancytopenia.
Introduction
Pancytopenia is a medical condition where there is decrease in cell count from all three lineages from bone marrow resulting in anaemia, leukopenia, and thrombocytopenia. It is usually due to the underlying disease process affecting bone marrow or peripheral blood cells. However the finding of pancytopenia is obtained via hemogram, it may have varied presentation and cause of occurrence.
We observed 6 cases of pancytopenia. All of them were evaluated following a common protocol for pancytopenia. Following diagnosis of the causes of pancytopenia, they were treated accordingly and were followed up. Thus, we conducted a prospective study of 6 pancytopenia cases. ([Table 1])
Case Presentation
We present a series of cases of pancytopenia and their details.
Case 1
A 64-year-old hypertensive female with rheumatoid arthritis came to ER with mucosal bleeding and multiple mucosal ulcers in mouth cavity for 2 days not controlled by any home medication. There were reddish black lesions over nail beds of both upper and lower limbs. She had wrongly taken methotrexate 15 mg tablet for 10 consecutive days. Blood counts and peripheral blood smear revealed pancytopenia (total leucocyte count, TLC-740/cmm; hemoglobin-10.9 gm/dl; platelet count-57000/cmm). Liver function test (LFT), Renal function test was normal. Blood and urine cultures and tropical infection screen was unyielding. Ultrasound of abdomen normal except presence of gall bladder sludge. Keeping with history, clinical presentation and lab findings, diagnosis of methotrexate poisoning was made. Patient was treated with broad spectrum iv antibiotic coverage, anti-fungal, antacid, local mouth care with chlorhexidine mouth wash. Patient was also given injection folinic acid 15 mg iv 6 hourly for 3 days and G-CSF subcutaneous 300 mcg daily. Patient transfused with prbc, and platelet as required. She was monitored strictly and on lesions mostly subsided. Haematologist and rheumatologist opinion was taken and discharged on 10th day. Thus, it was a case of methotrexate overdose induced pancytopenia. Patient was followed up after 2weeks and 1 month, she did not have any discernible pallor. Her Complete hemogram showed a hemoglobin of 11gm/dl, total leukocyte count 7500/cmm and platelets 1.58lakhs/cmm. She was having corrected dose of methotrexate (weekly) and there was no sign of any mucosal ulcer or bleeding.
Case 2
A 19-year-old ([Figure 1]) without any known comorbidity was admitted with complaint of fever for 10 days, which was high grade, documented, 3 to 4 times daily, relieved on taking paracetamol tablet, associated with occasional pain abdomen and diarrhoea. There was no history of any dysuria, headache, neck pain, cough, dyspnoea. There was history gradual loss of weight over long duration. Patient was cachectic and had BMI 17.2. On examination there was severe pallor, and examinations revealed no significant abnormality like organomegaly or lymph node enlargements. Lab values revealed pancytopenia (total leukocyte count, TLC-600/cmm; hemoglobin-3.7gm/dl; platelet count-30000/cmm) with MCV-106.3 fl, MCH- 33.3pg. Peripheral blood smear showed normocytic normochromic RBCs. Liver function test was normal, ANA- negative, LDH-1000unit/L, Vitamin b12-348pg/L, folate 10.2 ng/L, HPLC-no abnormality, triglyceride-160mg/dl, uric acid-2.5mg/dl. Iron-22, TIBC-142, ferritin-4189 in 1/5 dilution, splenoportal doppler-normal study. Tropical fever screening was negative. Patient had absolute neutropenia and so was kept in isolation with barrier nursing. Patient was transfused with PRBC; platelet as required. Patient was given G-CSF (granulocyte colony stimulating factor), broad spectrum anti biotic coverage, anti-fungal and antibiotic level monitored through trough level. Patients counts gradually improved and became afebrile. Bone marrow aspiration and biopsy was done. Bone marrow biopsy revealed granulomatous inflammation. Bone marrow aspiration revealed erythroid hyperplasia with megaloblastic changes, gram stain fungal stain ZN stain and MTB GeneXpert were all negative. But bone marrow aspiration fungal culture revealed growth of Aspergillus niger. Thus, it was diagnosed as a case of Aspergillus infection induced pancytopenia. Patient was treated with inj voriconazole and later discharged. Patient was followed up after 1month when repeat complete blood count revealed improved count.

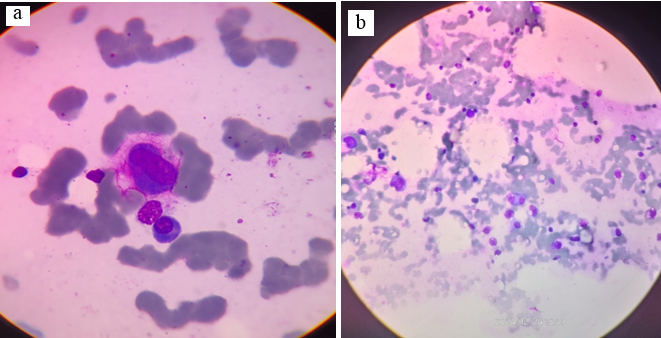
Case 3
A 17-year-old female was admitted with complaint of fever for 7 days associated with chills and rigor. But gradually she developed generalized weakness and was having dizziness while walking. On admission she had severe pallor and hypotension. Initial lab revealed pancytopenia (Total leukocyte count, TLC-1700; hemoglobin-2.3; platelet count-102000/cmm). Tropical fever screening revealed presence of plasmodium vivax trophozoite ([Figure 2]) in peripheral blood smear and dual antigen test for malaria positive for vivax antigen. Thus, it was a case of complicated Vivax malaria. Ldh-467 unit/l, direct coombs test negative, retic count-0.43%, Vit B12-pg/L, Folate 5.7ng/L, transferrin saturation around 30%, ferritin 56, peripheral blood smear suggestive of erythropenia. G6PD assay revealed no enzyme deficiency. Based on fever pattern and lab findings complicated vivax malaria was diagnosed. Patient given 4units of PRBC (packed RBC transfusion) and artesunate and primaquine given in appropriate dosage and recommended regimen. USG revealed mild fatty liver and no splenomegaly. She gradually became afebrile and counts improved. Patient was followed up after 2 weeks

Case 4
72-year-old female patient admitted with complaint of fever along with cough with expectoration for around 5 days. She complained of similar episodes since last 3 months. She also complained of generalized weakness fatigue and weight loss. Fever screen was negative. Sputum study revealed no significant abnormality with absence of any clue of TB. Chest X Ray was suggestive of right sided middle lobe consolidation. Complete blood count revealed: - Hb 4.9 g/dl, MCV 122.4 fl, MCH 34.3 pg., Platelet 5000/cmm, Total leukocyte count was 400/cmm [ Differential count Neutrophils 7%, Lymphocytes 80%, Monocyte 0%, Eosinophils 13%, Basophil 0%]. Vitamin B12 and folate were within normal limit. Investigations to rule out any congestive causes of pancytopenia were within normal limit. Patient was started on piperacillin tazobactam, teicoplanin, fluconazole. Patient was also given G-CSF. Bone marrow aspiration was done to evaluate bone marrow status, and it revealed Reactive marrow with erythroid hyperplasia and dyserythropoiesis suggestive of myelodysplastic syndrome [MDS]([Figure 3]a,b). The patient developed sudden worsening of severe respiratory distress with fever. She had severe hypotension and lab reports revealed Septic shock. Patient was put on ventilator support and all supportive measure given but the patient succumbed to septic shock.
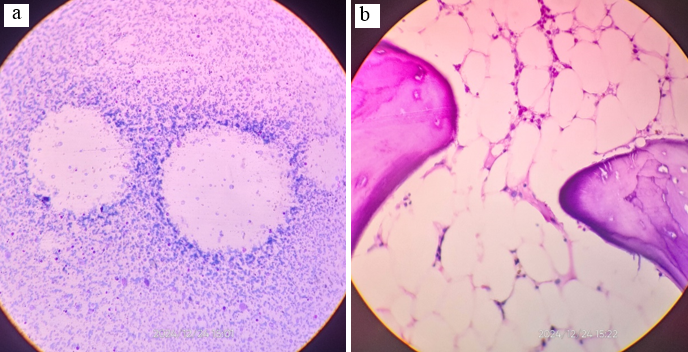
Case 5
Patient admitted with complaint of generalized body weakness, recurrent fever with cough. On examination there was severe pallor. But there was no organomegaly, any palpable lymph nodes or any signs of potential diagnostic clues. Lab evaluation revealed pancytopenia in blood count (Hb-2.7gm/dl, TLC-2700/cmm, platelet count-30000/cmm). Peripheral blood smear revealed normocytic normochromic anemia, Retic counts 0.7, Liver function test within normal limit, USG and Splenoportal Doppler within normal limit. Vitamin b12, folate, iron profile was within normal limit. Bone aspiration and biopsy was done which revealed exclusively hypocellular bone marrow with depression of trilineage haematopoiesis suggestive of hypoplastic anemia without any evidence of granuloma or malignant cells ([Figure 4]a,b). Patient was planned for hematopoietic stem cell transplantation.
|
Case No. |
Presentation |
Initial hemoglobin level (g/dl) MCV (fL), MCHC(%), Platelet level (per cmm), TLC level (per cmm) |
Diagnostic modality |
Diagnosis |
Outcome |
|
1 |
• Mucosal Bleeding • Multiple Oral Ulcers • Reddish Black Lesions in Nail Beds |
Hb-10.9 MCV-90.1 MCHC-29.5 Platelet-57000 TLC-740 |
History of drug intake |
Methotrexate overdose |
Methotrexate was withheld. Patient given folinic acid and GCSF. Pancytopenia was corrected with conservative management. |
|
2 |
• Fever • Chronic Significant Weight Loss • Cachexia |
Hb-3.7 MCV-106.3 MCHC-31.4 Platelet-30000 TLC-600 |
Bone marrow aspiration fungal culture |
Aspergillus niger infection in bone marrow |
Patient was treated with iv voriconazole and pancytopenia was corrected |
|
3 |
• Fever With Chills and Rigor • Visible Pallor • Hypotension |
Hb-2.3 MCV-83.1 MCHC-22.1 Platelet-102000 TLC-1700 |
Peripheral blood smear and malarial dual antigen test |
Complicated vivax malaria |
Pancytopenia corrected on conservative management with antimalarial drugs. |
|
4 |
• Fever With Cough and Expectoration • Significant Weight Loss |
Hb-4.9 MCV-122.4 MCHC-28.0 Platelet-5000 TLC-400 |
Bone marrow aspiration and biopsy |
Myelodysplastic syndrome |
Death due to septic shock |
|
5 |
• Generalized Body Weakness • Recurrent Cough with Fever |
Hb-2.7 MCV- MCHC- Platelet-30000 TLC-2700 |
Bone marrow aspiration and biopsy |
Aplastic anemia |
Planned for hematopoietic stem cell transplant. |
|
6 |
• Dyspnoea On Walking Short Distances • Chronic Diarrhoea |
Hb-6.6 MCV-126.4 MCHC-31.9 Platelet-73000 TLC-3200 |
Vitamin B12 assay |
Hypovitaminosis B12 |
Patient supplemented with methylcobalamine intramuscularly and oral folic acid. Pancytopenia was corrected on follow up |
|
Impaired production |
Peripheral destruction |
Bone marrow infiltration |
|
• Autoimmune diseases (SLE, RA, sarcoidosis) |
• Consumption (DIC, APML) |
• Non malignant |
|
• HLH |
• Splenomegaly |
1. Myelofibrosis |
|
• Aplastic anemia |
• Portal hypertension/cirrhosis |
2. Granulomatous infection (TB, Fungal) |
|
• PNH |
• Infection E.G EBV |
3. Storage diseases |
|
• Drugs (Cytotoxic) |
• SLE/RA |
• Malignant |
|
• Nutritional deficiencies (vitamin B12, Folate, Copper, Alcohol) |
• Myelofibrosis |
1. Leukemias |
|
• Viral infection |
• Storage disorder E.G gaucher |
2. Myelodysplastic syndrome |
|
|
• Malignancies e.g. lymphoma, Myelo-Proliferative neoplasms |
3. Multiple myeloma |
|
|
|
4. Metastasis |
Case 6
Patient admitted with complaint of dyspnoea on walking short distances, anorexia, and history of chronic diarrhoea. There was severe pallor, no organomegaly, no palpable lymph nodes, no abdominal tenderness. Initial lab values revealed pancytopenia (Hb-6.6gm/dl, mcv-126fl, mch37.9, TLC-3200/cmm, platelet-73000/cmm). Peripheral blood smear revealed macrocytic hypochromic RBCs. Anemia evaluation revealed folate-20, vit b12- 152, iron-41, ferritin-125, TIBC- 232, HPLC- normal, DCT-negative, LFT within normal limit, Retic count-0.7. bone marrow aspiration and biopsy revealed reactive marrow with megaloblastic changes. Evaluation for chronic diarrhoea and multiple vitamin deficiency was done. Serum TTG-IgA (Tissue transglutaminase IgA antibody), Intrinsic factor Antibody, anti-parietal cell antibody, D-Gliadin, ASCA were within normal limit. Upper GI endoscopy with duodenal biopsy and long colonoscopy with ileal biopsy revealed no abnormality. Clinical diagnosis of hypovitaminosis B12 induced pancytopenia was made. Patient was given injection Methyl cobalamin in recommended dosage as per protocol. Patient was discharged and followed up after one month when her complete blood counts improved and there was no anaemia.
Discussion
The pathogenesis of pancytopenia includes impaired production, bone marrow infiltration, peripheral destruction or a combination of all the above[1], [2] ([Table 2]). The common cause of pancytopenia varies from place to place all over the world. A study in Mexico showed most common cause to be myelodysplastic syndrome,[3] in Cape town, South Africa it was chemoradiation therapy,[4] in Jodhpur, India acute leukemia,[5] in Kolkata, India it was aplastic anemia.[6]
Diagnosis of pancytopenia is a challenging task as different pathologies and etiologies require different approach and tests. We followed a common protocol for our cases. Once pancytopenia was confirmed, first we ruled out any drugs or toxins, then we did initial work up to get idea about the contributing pathologies e.g. peripheral blood smear, reticulocyte production index. Then we did evaluation to find the cause of exact etiology which included LFT, splenoportal doppler, bone marrow aspiration and biopsy, ANA, SPEP (Serum protein electrophoresis), nutrient assays as and when required.[7], [8] Alongside evaluation of pancytopenia other pathologies were treated e.g. in case 4 patient was managed of neutropenic fever with proper antibiotics and antifungals with inotrope support for sepsis.
Methotrexate is an immunosuppressant drug used for inflammatory or autoimmune diseases. It interferes with cellular proliferation. Previous case reports[9], [10], [11], [12] of methotrexate overdose had similar mucocutaneous and haematological manifestation like our case 1. Such cases need earliest application of leucovorin and GCSF.
Primary bone marrow diseases like aplastic anemia and myelodysplastic syndrome require bone marrow study for diagnosis. Further they need genetic evaluation for congenital syndromic associations and further planning of treatment.[13], [14]
One of the common tropical infections induced pancytopenia is due to complicated vivax malaria. Here the pathology is primarily due to haemolysis by malarial pathogen. These cases respond quickly to conservative management with antimalarials.[15], [16]
Pancytopenia with megaloblastic anaemia due to vitamin deficiency is based on the concordance of anamnestic, clinical, cytological elements and the assay of associated biomarkers. Most common cause of this deficiency is inadequate nutritional intake. Vitamin B12 substitution, traditionally administered intramuscularly, has been shown to be effective. Folic Acid supplementation is administered orally. The importance of early diagnosis and prompt vitamin supplementation is because of potential complications.[17], [18], [19]
Conclusion
We observed 6 cases of pancytopenia in our institution and followed up those patients till recovery where possible. Pancytopenia may be caused by multiple drugs. It very important to explain the possible side effects of such drugs and to follow the patients.[9], [10], [11] Overdosing can be avoided by mentioning day and time of intake per week. A large portion of patients of pancytopenia are first diagnosed during evaluation for infections with fever. These patients must be dealt with caution post pancytopenia detection as they tend to develop severe sepsis due to leukopenia. Pancytopenia due to nutrition deficiencies like hypovitaminosis B12 must be evaluated for chronic diarrhoea and malabsorption syndromes. For evaluation of Pancytopenia with fever the bone marrow aspiration and biopsy must be sent for fungal culture along with CB-NAAT (cartridge based nucleic acid amplification test) and routine culture sensitivity, as fungal infections like Aspergillus, though rare, will be missed otherwise.
Conflict of interest
None
Financial support
None
References
- Gnanaraj J, Parnes A, Francis C, Go R, Takemoto C, Hashmi S. Approach to pancytopenia: Diagnostic algorithm for clinical hematologists. Blood Rev. 2018;32(5):361-7. [Google Scholar]
- Chiravuri S, Jesus O. . Pancytopenia. 2023. [Google Scholar]
- Vargas-Carretero C, Fernandez-Vargas O, Ron-Magaña A, Padilla-Ortega J, Ron-Guerrero C, EB. Etiology and clinico-hematological profile of pancytopenia: experience of a Mexican Tertiary Care Center and review of the literature. Hematology. 2019;24(1):399-404. [Google Scholar]
- Nell E, Chapanduka Z. Aetiology of pancytopenia: Experience of a South African tertiary academic centre. Afr J Lab Med. 2022;11(1). [Google Scholar] [Crossref]
- Patel G, Prajapati G. Spectrum of Pancytopenia in Adults Attending a Clinical Hematology Department: A Four-Year Experience From a Tertiary Care Center of Western India. Cureus. 2022;14(5). [Google Scholar] [Crossref]
- Dasgupta S, Mandal P, Chakrabarti S. Etiology of Pancytopenia: An observation from a referral medical institution of Eastern Region of India. J Lab Physicians. 2015;7(2):90-5. [Google Scholar]
- Das S. Pancytopenia: An Update. J Exp Pathol. 2020;1(1):28-32. [Google Scholar]
- Geissler K. Pancytopenia—a diagnostic challenge?. memo - Magazine Eur Med Oncol. 2021;14(4):1-5. [Google Scholar]
- Srinivasa B, Padmini PS, Kumar P, Philip A, Presannan A, Thomas R. A Case Report on Methotrexate Overdose Induced Pancytopenia and Mucocutaneous Ulcerations. Indian JPharm Pract. 2020;13(4):359-61. [Google Scholar]
- Tel B, Bilgin S, Kurtkulagi O, Kahveci G, Aktas R, Kurt K. Severe Pancytopenia and Stomatitis Case due to the Treatment with High Dose Methotrexate. Nat J Health Sci. 2021;6(1):32-4. [Google Scholar]
- Ajmani S, Singh Y, SP, Chowdhury A, Aggarwal A, Lawrence A. Methotrexate-induced pancytopenia: a case series of 46 patients. Int J Rheum Dis. 2017;20(7):846-51. [Google Scholar]
- Dezern A, Churpek J. Approach to the diagnosis of aplastic anemia. Blood Adv. 2021;5(12):2660-71. [Google Scholar]
- Pratim P, Kumar S, Shilpi S, Krishna G, Biswajit H, Aditi A. Aplastic anemia: A common hematological abnormality among peripheral pancytopenia. N Am J Med Sci. 2012;4(9):384-8. [Google Scholar]
- Lancaster I, Patel D, Sethi V, Connelly W, Namey J. Myelodysplastic syndrome in a case of new-onset pancytopenia. Clin Case Rep. 2022;10(3). [Google Scholar] [Crossref]
- Albaker W. Acute Plasmodium vivax malaria presenting with pancytopenia secondary to hemophagocytic syndrome: case report and literature review. J Family Community Med. 2009;16(2):71-3. [Google Scholar]
- Pandey N, Bhambri A. Prevalence Of Pancytopenia In Patients Of Plasmodium Vivax Malaria In A Tertiary Care Hospital. National J Integr Res Med. 2018;8(1):21-4. [Google Scholar]
- Costanzo G, Sambugaro G, Mandis G, Vassallo S, Scuteri A. Pancytopenia Secondary to Vitamin B12 Deficiency in Older Subjects. J Clin Med. 2023;12(5). [Google Scholar] [Crossref]
- Depuis Z, Gatineau-Sailliant S, Ketelslegers O, Minon J, Seghaye M, Vasbien M. Pancytopenia Due to Vitamin B12 and Folic Acid Deficiency-A Case Report. Pediatr Rep. 2022;14(1):106-14. [Google Scholar]
- Gladstone E. Pernicious Anemia Presenting With Pancytopenia and Hemolysis: A Case Report. J Med Cases. 2019;10(4):81-3. [Google Scholar]
Article Metrics
- Visibility 9 Views
- Downloads 2 Views
- DOI 10.18231/pjms.v.15.i.1.260-265
-
CrossMark
- Citation
- Received Date April 13, 2024
- Accepted Date January 21, 2025
- Publication Date May 13, 2025